Gynaecology tests and symptom relief procedures
Information for patients under the care of the Gynae-Oncology Team
You have been contacted by the hospital to come for a biopsy or procedure. This leaflet tells you about the various tests you may need, so that we can find out what is causing your symptoms and plan your future treatment. It also includes information on some of the procedures we can use to treat your symptoms. It does not replace any information given to you by your doctor or specialist nurse.
Who will be performing the tests?
Each of the procedures mentioned in this leaflet is carried out by a specially trained doctor (radiologist).
Where will the tests take place?
The procedures usually take place in the Radiology Department in one of the scan rooms.
In an emergency, some of the procedures may be performed on the ward.
How do I prepare for my appointment?
Please make sure you bring a list of your current medications with you to your appointment, especially those that affect blood clotting like aspirin or blood thinners.
You may be asked not to eat or drink anything for a few hours before your biopsy. Details of this will be included in your appointment letter or given to you by your clinical nurse specialist.
Your doctor or clinical nurse specialist will tell you whether to take your regular medications during your fasting period, and they may give you other special instructions as well.
Do I need to bring anything to my appointment?
Along with a list of your medications, depending on which procedure you are having, you might be told to bring an overnight bag to your appointment.
To make sure that all patients get the best care and attention during their procedure, your appointment may be delayed. We often arrange appointments at short notice, which means that the Radiology Department is not always able to honour the time slot given. It is extremely rare for anyone to have their procedure cancelled on the day for this reason. We would recommend bringing some reading material or light entertainment, especially if you are likely to need four hour bed rest after your procedure.
Can I bring someone with me to hospital?
Yes, a relative or friend can come with you to hospital, but they will not be able to stay with you for your procedure or wait on the ward. They will be allowed to visit during allocated ward visiting hours.
What is a biopsy and why might I need one?
A biopsy is a procedure where a small sample of cells or body tissue is taken, so that it can be examined under a microscope. This is often done with a needle, after you are given local anaesthetic to numb the skin in the area the biopsy is to be taken.
Below is a list of the possible biopsies you may have. The biopsy you will be having will have been explained to you in detail before we ask for your consent to continue. Please use the time before your procedure to speak to the radiologist if you have any last minute questions or concerns. Remember you can withdraw your consent for treatment at any time.
Omental biopsy
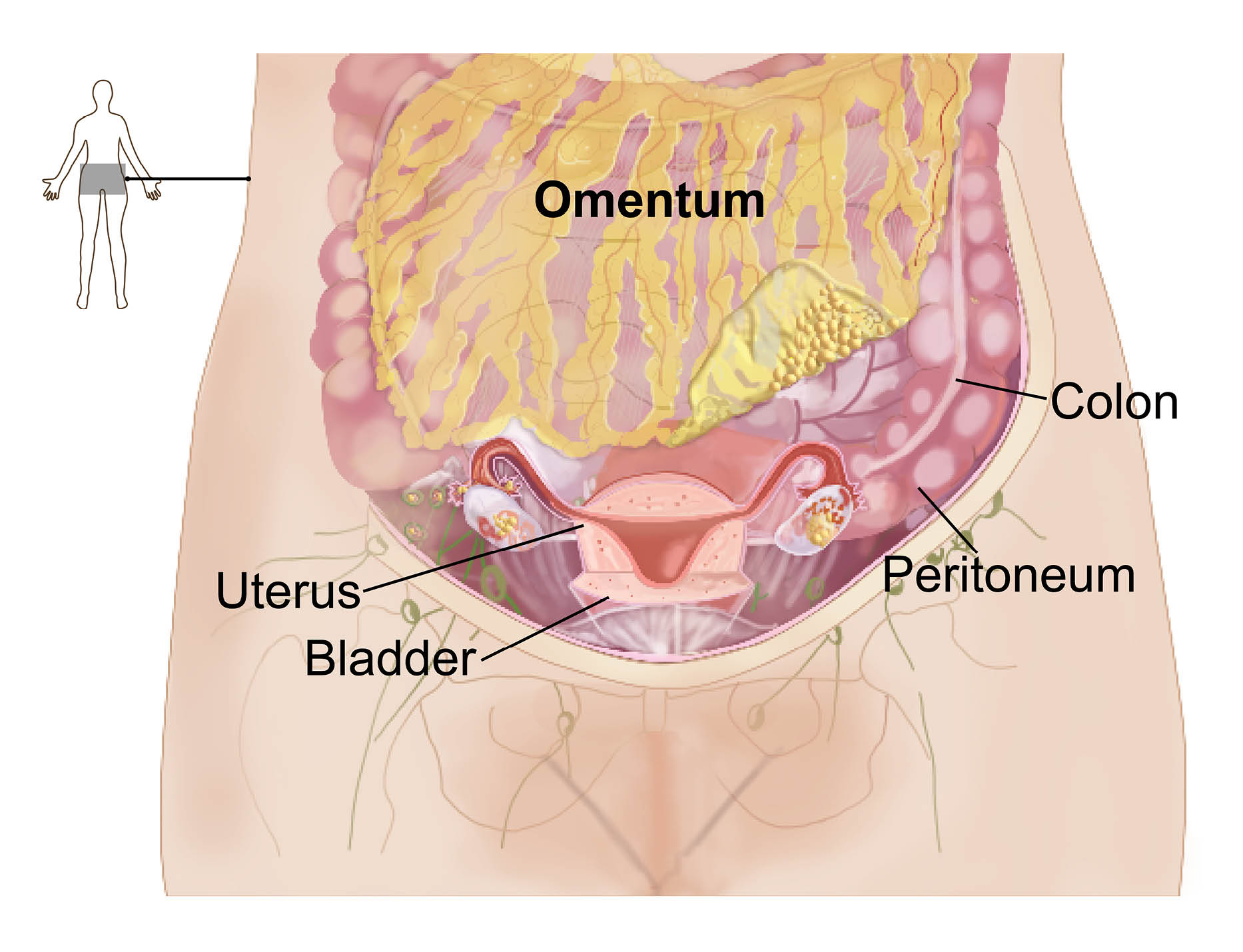
The omentum is a large fatty tissue layer that lines the organs in your abdomen. It is very often not the cause of your symptoms, however as it is in close contact with most of the organs in your abdomen, it tends to collect evidence of most conditions and can help us diagnose your condition.
We recommend a biopsy of the omentum, when there is evidence of deposits on your scans, as we can get easy access to it. An ultrasound scanner is used to find the right place to take the biopsy and reduce the risk of injury to your surrounding organs.
After giving you a local anaesthetic to numb your skin, a needle is used to take a small amount(a biopsy) of the omental tissue. You should stay in bed for the first four hours after this procedure. If you feel well after this period, you will be allowed home.
Common risks include tenderness and bruising after your procedure, but these will pass quickly. Rare complications include infection, bleeding, and injury to internal organs.
Peritoneal biopsy
The peritoneum is the lining of the abdomen (see diagram above). It can sometimes collect evidence of conditions in the abdomen, so we occasionally recommend a biopsy of the peritoneum when there is evidence of deposits on your scans.
An ultrasound or CT scanner is used during your procedure, to find the right place to biopsy and reduce the risk of injury to your surrounding organs. After giving you a local anaesthetic to numb your skin, a needle is used to take a small amount of the peritoneal tissue (a biopsy).
You should stay in bed for the first four hours after this procedure. If you feel well after this period, you will be allowed home.
Common risks include tenderness and bruising. Rare complications include infection, bleeding, and injury to internal organs.
Groin node biopsy
Lymph nodes (gland) are small round organs that are part of the body’s lymphatic system. They swell in response to infection, immune conditions, and cancer.
Swollen nodes in the groin are easy to access for biopsy. After giving the local anaesthetic to numb your skin, a needle is used to take a sample of the cells in your lymph node. This is a short procedure and you will be allowed home immediately afterwards.
Common risks include tenderness, bruising, or bleeding.
What other procedures might I have?
Ascitic tap
This is where a small amount of ascitic fluid (abnormal fluid build-up of the abdomen) is removed from your abdomen. The fluid is removed using a needle, after your skin has been numbed with a local anaesthetic.
An ultrasound scanner is used during the procedure to find an area with a large amount of fluid. This will reduce the risk of injury to your internal organs. The cells in the fluid are collected and sent to a laboratory for examination.
You will be allowed home shortly after your procedure.
Tenderness and mild bruising around the area where the needle was inserted is normal for the first few days after your procedure. Ascitic fluid may also leak from the area of the sample in the first 72 hours.
Ascitic drain
The main aim of this procedure is to remove the excessive amounts of ascitic fluid you currently have in your abdomen. This should help relieve the tightness, swelling, and shortness of breath you are feeling.
To do this, a drain is placed in your abdomen to remove as much ascitic fluid (abnormal fluid build-up of the abdomen) as possible. This involves numbing your abdomen with a local anaesthetic, before placing a fine tube into your abdomen.
An ultrasound scanner is used during the procedure to find an area with a large amount of fluid, in order to reduce the risk of injury to your internal organs.
For most people this can be done as a day case procedure. However, as the aim is to relieve you of as much fluid as possible, you might need an overnight stay in hospital to allow all the fluid to drain. Please pack an overnight bag in case this happens.
The cells in the fluid are collected in the laboratory and examined under the microscope.
Common risks include tenderness, mild bruising, a drop in blood pressure, and leakage of ascitic fluid from the area the drain was sited. More serious but rare complications include an infection in your abdominal cavity and injury to internal organs.
Pleural drain
A pleural effusion is when fluid gathers between the two layers of membrane covering your lungs. A drain is placed into your lungs to remove as much pleural fluid as possible.
This involves placing a fine tube in your chest. An ultrasound scanner is used during the procedure to find an area with a large amount of fluid to reduce the risk of injury to your internal organs.
Common risks include tenderness and bruising. More serious but rare complications include shortness of breath from air getting into the pleural space (pneumothorax) and injury to the lungs. As the aim is to relieve you of as much fluid as possible, you will need an overnight stay in hospital to allow all the fluid to drain. Please pack an overnight bag if you are having this procedure.
What happens next?
Once the laboratory has contacted us with your results, we will be in touch with you either by phone or letter to let you know what will happen next.
What if I feel unwell at home?
If you feel unwell or develop any of the common complications mentioned for your procedure when you return home, contact the Gynaecology Assessment Unit on 01843 235009 and speak to a member of the team.
If you develop a temperature, abdominal pain, or breathing problems, go to your nearest Emergency Department.
Contact details
If you have any questions or concerns either before or after your procedure, please contact either of the following.
Gynaecology Assessment Unit, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235009Clinical Nurse Specialist
Telephone: 01227 868666