Frozen shoulder (stiff shoulder / adhesive capsulitis)
Information for patients from the Trauma and Orthopaedics (T&O) Department
You have been diagnosed with a frozen shoulder, also called stiff shoulder or adhesive capsulitis. This leaflet will explain what a frozen shoulder is, the signs and symptoms, and how it can be diagnosed. Although the exact method of treatment will differ from patient to patient, the most common treatments used by East Kent Hospitals and their likely outcomes are also covered here. It will also give you information about what you need to do through the process.
If after reading this leaflet you still have questions or concerns, please speak to your surgeon or anaesthetist at your next appointment.
Contents page
What is a frozen shoulder?
How does frozen shoulder develop?
Who is more likely to develop a frozen shoulder?
What are the available treatment options?
What are the non-surgical (conservative) treatments?
What are the surgical treatments?
How can I prepare for my surgery?
What happens on the day of my surgery?
What kind of anaesthetic will I need?
What are the complications and risks?
How long will I stay in hospital?
Will I be in pain after my surgery?
What painkillers will I be sent home with?
How do I care for my wound(s) at home?
How long will my wound(s) take to heal?
What if my wound bleeds at home after keyhole surgery?
If I had keyhole surgery, can I have a bath or shower?
Why am I wearing a sling after my surgery?
What is the best position to sleep in?
When can I drive again? When can I return to work?
When can I start my normal activities?
When should I start noticing improvement?
Will I have a follow-up appointment?
What if I have any questions or concerns?
Exercises and physiotherapy advice
Contact details
What is a frozen shoulder?
A frozen shoulder is a condition that causes the shoulder to become stiff and often painful. The lining of the shoulder joint becomes inflamed (red, hot, swollen, and / or painful) and scarred, resulting in shoulder stiffness. The reasons why this happens are not clear.
-
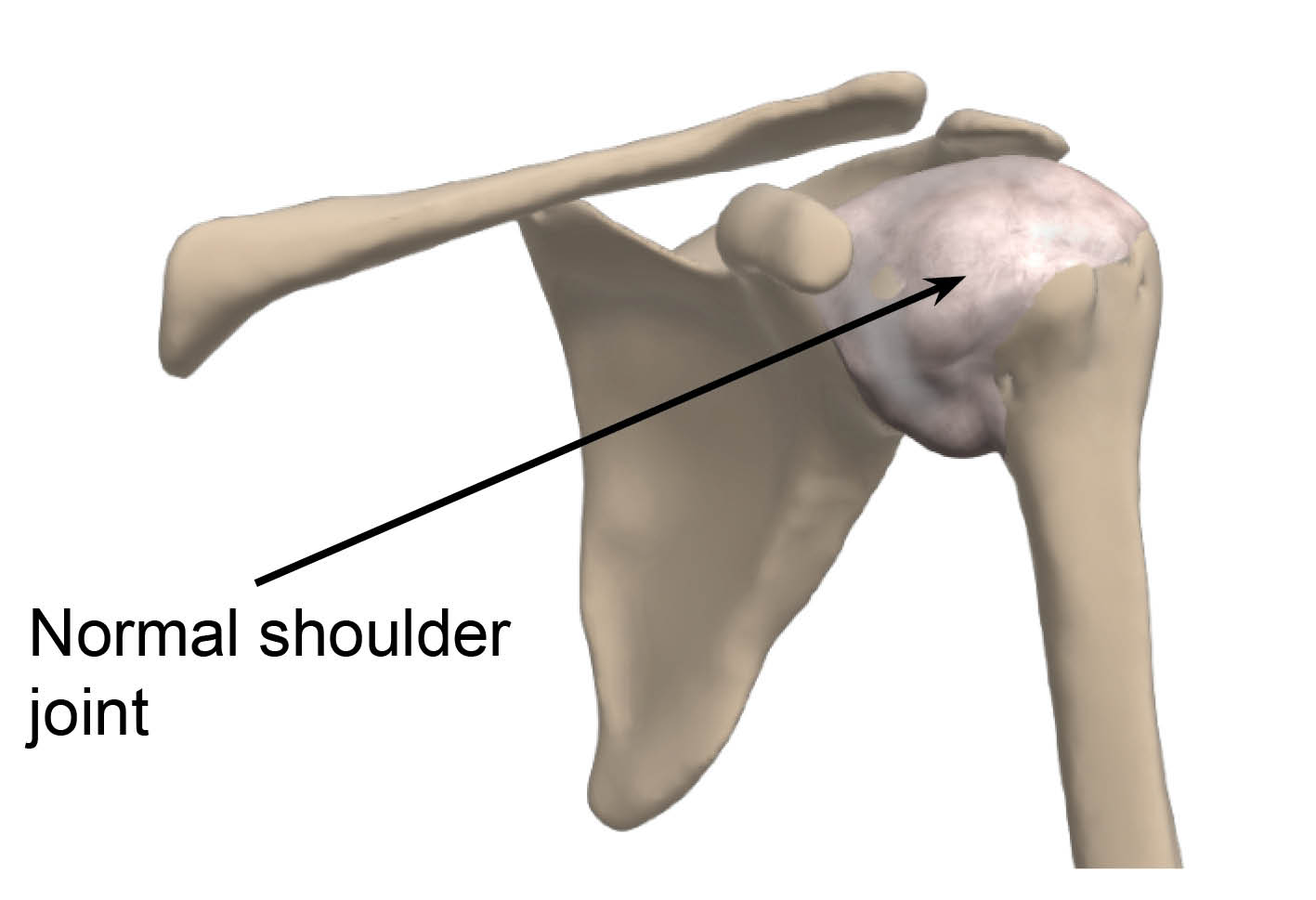 Normal shoulder joint
Normal shoulder joint -
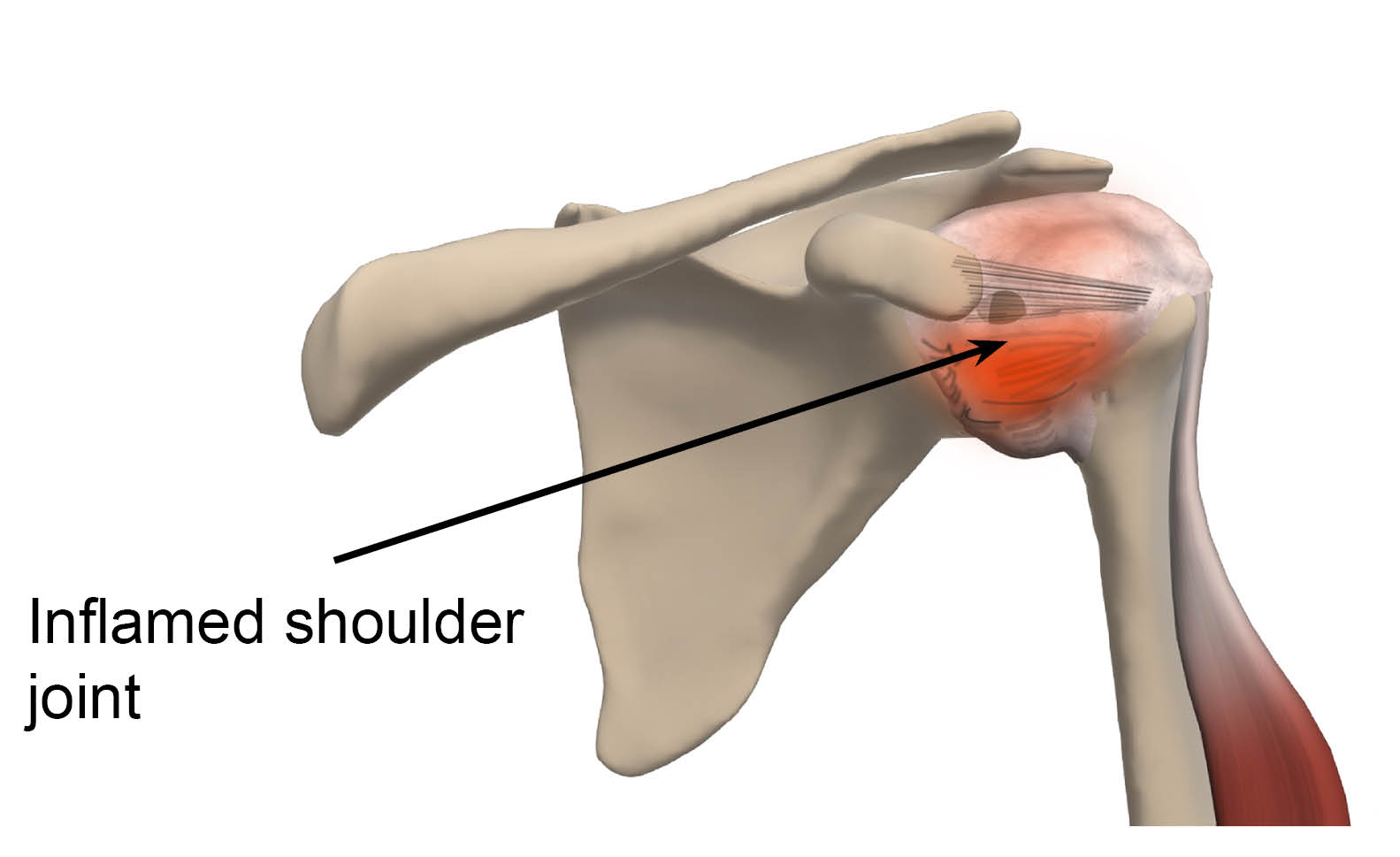 Inflamed shoulder joint
Inflamed shoulder joint
How does frozen shoulder develop?
Early on in the condition, pain seems to be the most common problem. This is due to the inflammation of the lining of the joint. The movement of the shoulder is often still normal.
As the condition progresses, the lining of the shoulder joint becomes scarred, and stiffness begins to set in. Although all parts of shoulder movement can be affected, external rotation or moving your hand away from your body with your elbows tucked in, is the most often affected, even as the pain tends to ease.
The condition lasts for 18 to 24 months, so it needs to be dealt with patiently. Most patients move through three phases.
The first phase is ‘freezing’ when the shoulder starts getting stiff and there is severe pain.
The pain begins to settle in the second phase, but the movement remains restricted.
The final or the ‘thawing’ phase includes a gradual return to normal movements. However, some stiffness may remain.
Who is more likely to develop a frozen shoulder?
Frozen shoulder is more likely to develop in middle aged females.
There are certain conditions which can mean you are more likely to develop frozen shoulder. These include diabetes, hypothyroidism, trauma, and certain medications. However, in most patients the condition develops quietly without any obvious cause, hence the term ‘idiopathic’ (the cause is unknown) frozen shoulder.
What are the available treatment options?
There are some important points to remember about what will happen if you have frozen shoulder.
Over time the condition tends to resolve by itself in most patients with pain management and physiotherapy. However, the time from pain setting in to return of movement can take 18 to 24 months. Sometimes the movement of the affected shoulder may not completely return to normal.
Because of this, there are several things we can offer to make things more comfortable for you while the condition runs its course. Treatment options may also help with the stiffness that you are left with after having frozen shoulder.
What are the non-surgical (conservative) treatments?
Pain relief and physiotherapy are the main treatments for frozen shoulder.
Pain relief should be taken in a timely and adequate manner to allow the physiotherapist to work with you to resolve your stiffness in a more comfortable way.
As your movement is restricted, the aim of physiotherapy is to slowly help stretch the tight shoulder lining that causes your restriction of movement, as well as strengthen the muscles of your rotator cuff. A steroid injection can also be used alongside physiotherapy.
What are the surgical treatments?
In some cases, the stiffness can limit your day-to-day activities to a point where you may need to consider surgery.
Surgery involves a gentle examination and manipulation of your shoulder under general anaesthetic (you are asleep during the operation), followed by keyhole surgery. This surgery is called an arthroscopic release and synovectomy of the shoulder.
The aim of the manipulation under anaesthetic is to reduce the recovery time. The way this is performed is by having the joint stretched by the surgeon in a controlled manner, to gain a full range of movement. This is combined with an injection of local anaesthetic and steroid to reduce inflammation and pain.
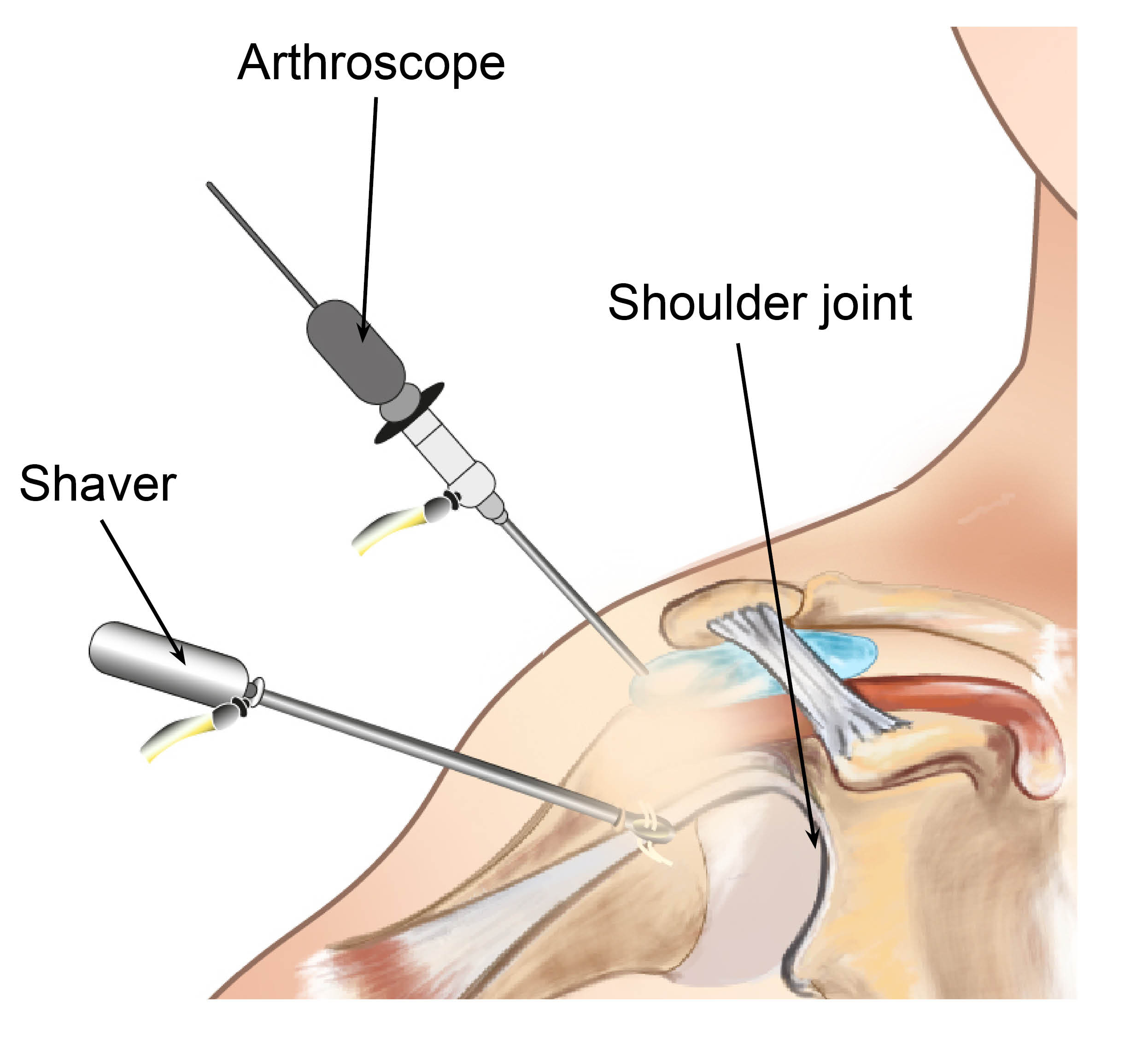
If manipulation does not work, it may be necessary to perform further arthroscopic release of your tight tissues. This is done using keyhole surgery, which usually involves having two or three small cuts around your shoulder. Your surgeon will use those cuts to insert a small camera and the instruments needed to examine your joint, and perform the operation to surgically release the tight tissues.
How can I prepare for my surgery?
You will have a preassessment appointment before your surgery, to check if you are ready and fit for surgery. You will also be swabbed for MRSA and Covid-19, if necessary.
Before surgery it helps if you try to get as fit as possible to avoid anaesthetic risk and / or failure of the surgery. It is important that you lose weight if you are above your ideal weight.
Smoking advice
It is important to stop smoking at least 30 days before your surgery. Studies have shown that wound healing is significantly delayed by smoking / nicotine, and the infection rate is much higher. Smoking also harms how your tendon heals following a repair, so smoking after your operation is also not advised.
If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
How does eating a healthy diet help my recovery?
Recovering from surgery can take a long time and it is normal to get frustrated and anxious. But remember that while you are recovering, there are some things you can do to help your wound to heal. We suggest limiting the amount of alcohol you drink, stopping smoking, eating a healthy diet, drinking plenty of fluids (especially water), and staying active. If you need any extra support, do not hesitate to get in touch with us on the contact numbers listed at the end of this leaflet.
Some painkillers (especially those containing Codeine) can cause constipation. To avoid this, please follow a healthy well-balanced diet rich in fruit, vegetables (including green leafy vegetables), nuts, seeds, wholegrains, and legumes, which contain the necessary fibre, and drink plenty of water. More information is available on the NHS 5 A Day: what counts? web site.
While you wait for your surgery date, you can start preparing for your operation. Research shows that fitter patients, who are able to improve their health and activity levels before surgery, recover more quickly. Taking an active role in planning and preparing for your operation will help you:
feel in control
leave hospital sooner, and
get back to normal more quickly.
To help with this, you may be contacted by a member of the One You Kent (OYK) team. OYK work in the community, and help patients improve their general health. This includes help and advice on:
Stopping smoking
Losing weight
Getting more exercise
More information can be found on the following web sites.
One You Kent (Kent Community Health)
Fitter Better Sooner Toolkit (Royal College of Anaesthetists)
What happens on the day of my surgery?
Please arrange for someone to pick you up from the hospital after your surgery, as you will not be able to drive yourself. Please make sure to arrange this before your surgery.
To avoid complications with your anaesthetic, you should not eat anything for six hours before your surgery, or drink anything for two hours. You will be given further instructions during your preassessment.
On the day of your surgery, you can take your usual medication as advised during your preassessment. If possible, do not take non-steroidal anti-inflammatory medication, such as ibuprofen and naproxen, for at least 10 days before your surgery, as they can affect how your wound heals. Please bring any medications that you are taking into the hospital with you.
If possible, please wear loose-fitting clothes, as after surgery you will be wearing a sling.
Bring your appointment letter with you, so you know which department to come to when you arrive at the hospital.
At arrival, you will be asked to put a hospital gown on, and maybe a pair of compression stockings.
You will see the anaesthetic and surgical team before your surgery to go through the consent form and discuss any questions you may still have. Remember you can withdraw your consent for treatment at any time.
You may be tested for Covid-19. All appropriate precautions will be taken during your admission to minimise the risk of contracting the illness as per Healthcare England Guidelines.
What kind of anaesthetic will I need?
This procedure is usually performed under general anaesthetic (you will be asleep for the procedure).
In addition, a local anaesthetic or nerve block is used during your operation. As a result, your shoulder and arm may feel numb for a few hours after your operation. It is important to take your pain medications during this time, to allow a gentle and easier control of pain when the nerve block wears off and your shoulder is likely to be sore and uncomfortable.
What are the complications and risks?
As with all surgery, there are a few risks and complications. These are rare and will be discussed with you before your surgery.
Anaesthetic risks will be discussed with your anaesthetist on the day of your surgery.
Wound infection (with keyhole surgery): we do everything we can to avoid this but an infection might still happen. If your wound becomes increasingly red or swollen after your surgery, please contact your GP or surgical team for advice as soon as possible.
Bleeding (with keyhole surgery): we will do our best to stop this as soon as possible, but some oozing may happen after your surgery.
Deep vein thrombosis (DVT) and / or pulmonary embolism (PE). These are blood clots which form in the blood stream and can be serious conditions. Compression stockings and other measures might be taken by the hospital to avoid them.
Soft tissue (nerve / tendon / blood vessel) injury could happen during surgery. We will try our best to avoid any damage.
Continued pain and Complex Regional Pain Syndrome (CRPS). CRPS is a condition where a person has persistent, severe, and debilitating pain. Although most cases of CRPS are triggered by an injury, the resulting pain is much more severe and long-lasting than normal.
Prolonged stiffness. Your shoulder could go back to being painful and stiff beyond the usual period expected for the stiffness to recover from a simple procedure. This could be avoided or improved if you take adequate pain relief and do the exercises listed at the end of this leaflet as your pain permits.
Fracture. The upper arm bone (humerus) might break during the surgery, but we will try to avoid this from happening.
The operation may fail to reduce the pain or movement in your shoulder. There should be about 75% improvement in symptoms in the first four to six weeks, however it is also possible that your symptoms do not improve as much and / or as fast. Further physiotherapy and treatment options can be discussed with your surgeon at your follow-up clinic appointment.
If the results are not good enough we may need to repeat the surgery.
If you have any questions or concerns about these complications, please speak to your doctor either during your preassessment appointment or before your surgery.
How long will I stay in hospital?
This procedure is usually carried out as a day operation, so you should be able to go home the same day.
After your operation, you will be taken to the ward until it is safe for you to be discharged home.
You will be seen by your surgeon, surgical care practitioner, and / or physiotherapist before you go home. They will show you what exercises to do and give you further advice to guide you through your recovery.
If you need to stay in hospital overnight, this will usually be explained to you during your preassessment appointment. If you have to stay overnight, make sure you bring with you items you may need, such as hygiene items (toothpaste and toothbrush), a dressing gown, slippers, and your usual medication. Also, we suggest you bring a book or magazine, in case there is a delay.
Will I be in pain after my surgery?
This type of surgery may be uncomfortable, and you will need appropriate pain relief afterwards. If your anaesthetist has given you a nerve block, your shoulder and arm may feel numb and weak. You may not feel any pain immediately after your surgery, as the block may take 12 to 24 hours to wear off completely.
You will be given painkillers when you leave the hospital, to take at home; these should last for at least two weeks. It is very important that you take your pain relief as advised and as early as you can before the nerve block wears off; this will help you to keep on top of your discomfort. It is advisable to take your painkillers regularly for the first few days. If possible, avoid non-steroidal anti-inflammatory medication, such as ibuprofen and naproxen, for at least 10 days before your surgery and six weeks following surgery. This is because anti-inflammatory medication could slow down the healing process.
Take pain relief regularly to try and keep your level of discomfort at a bearable level at all times. This allows the inflammation (redness, swelling, and heat) and pain to settle. Do not wait until your shoulder is very painful to take the pain relief, as it is then more difficult to control.
What painkillers will I be sent home with?
Surgical patients might be given some of the following painkillers, depending on their age, body weight, and individual circumstances, unless told otherwise by their doctor.
Take each painkiller as advised on your prescription.
Tablet paracetamol, 1g every four to six hours (no more than 4g per day).
Codeine Phosphate, 30 to 60mg every six to eight hours.
Tablet Tramadol, 50 to 100mg every eight hours.
Oramorph, 10 to 20mg every hour, as needed.
Anti-inflammatories may be prescribed; but you should try and take as few as possible immediately after your surgery.
Please note that Codeine, Oramorph, and Tramadol should not be taken together; you should only take one of the three at any one given time.
Ice packs or bags of frozen peas may also help reduce your pain. Wrap the pack / bag with a cloth and place it on your shoulder for up to 15 minutes. Do not eat these peas once they have defrosted.
If your pain continues and is not controlled with the medication you have been advised to take, then please contact your GP. You may also contact the East Kent Upper Limb Team if you need further help.
If you notice your wound area is becoming more painful, red, hot, and / or discharging pus (thick yellow discharge), you may be developing an infection. Contact your GP or surgical team for advice as soon as possible.
How do I care for my wound(s) at home?
If you had a repair through keyhole surgery, there will be few (three to five) wounds.
It is important to keep your wound and dressing dry and in place until your wound is well healed, and have your stitches removed at your two week follow-up appointment with your GP practice nurse or at the hospital, with your surgeon or your nurse practitioner (surgical care practitioner). You will be told where your follow-up appointment is going to be before you leave the hospital.
If the dressing gets wet or bloodstained, you can change them yourself by carefully placing a dressing from a pharmacy. If you are unable or have difficulties doing this yourself, you can ask a relative or a friend to change it for you, or you can make an appointment with your GP practice nurse to do it for you.
If you are being seen by your GP practice nurse for a wound check 10 to 14 days after your surgery, please make sure the nurse reads the following. These instructions are for healthy looking surgical wounds only.
*Colourful stitches are non-absorbable and need to be completely removed to avoid them getting buried under the patient’s skin.
*White / clear stitches are absorbable. If any suture knots have been made outside the patient’s skin, please remove these to avoid suture abscesses. Thank you.
*The appearance and material of the sutures can be different from Trust to Trust, but these are the most common.
If a wound does not seem to be healing appropriately, please leave the stitches / knots in place and make another appointment to remove them in few days.
How long will my wound(s) take to heal?
Wounds usually take between 10 to 14 days to heal.
The area around your wound(s) may have some numbness, which is usually temporary. You may feel occasional sharp pains or ‘twinges’, as well as itching near the scar as it settles.
What if my wound bleeds at home after keyhole surgery?
Occasionally there can be minor bleeding or clear fluid ooze in the first day or two after your surgery. If your dressings get wet or bloodstained, you can change them yourself by carefully placing a dressing from a pharmacy over your wound. If you are unable to this yourself, you can ask a relative or a friend to help or you can get an appointment with your GP practice nurse to do it for you. This bleeding or oozing should be controlled by pressing firmly but gently on your wound for 15 minutes.
If you are worried about the bleeding, you can contact the hospital on the number given to you (during normal working hours) or go to a walk-in centre or Emergency Department (after hours).
If I had keyhole surgery, can I have a bath or shower?
You should have a ‘dry wash’ or a shallow bath instead of a shower. This keeps your arm in the correct position and prevents your dressing and sling from becoming wet.
You should have a ‘dry wash’ or a shallow bath instead of a shower. This keeps your arm in the correct position and prevents your dressing(s) and sling from becoming wet.
While your wound is still healing:
do not use soaps, lotions, creams, or powders on your wounds, to avoid any infection getting in to your wound(s); and
keep your wound(s) dry at all times.
It is very important to remember to keep your armpit on your operated side clean and dry. Lean forward so you can reach your armpit, as separating it from the body sideways may be difficult or painful and is not allowed for the first four to six weeks.
You can wash and clean the area as normal once your wound is completely healed.
Why am I wearing a sling after my surgery?
You will return from surgery wearing a sling, to help keep your arm comfortable. It may be taken off as much as you wish and discarded as soon as possible. You will be encouraged to use your arm. You must begin moving and exercising your arm on the day of your surgery. Pain relief will enable you to carry out the exercises your physiotherapist has shown you. Wherever possible try to use your arm for normal daytime activities.
What is the best position to sleep in?
It might be difficult to sleep on your operated side, especially if you have had keyhole surgery. However, the pain will ease with time.
Take regular painkillers and try to support your shoulder by placing pillows behind it. If you lie on your back, a pillow under your arm and elbow may make you feel more comfortable. You may find it easier to lay on your non-operated side.
When can I drive again?
You can drive as soon as you feel comfortable and capable of doing the required emergency manoeuvres. The advice from the DVLA is that you should not drive until you are physically capable of controlling a motor vehicle and can perform an emergency manoeuvre safely and confidently.
Please arrange for someone to collect you from hospital and take you home after your surgery.
When can I return to work?
This will depend on your job. If you are in a sedentary job that does not need you to use much force you may return as soon as you feel able to, usually after two weeks. If your job involves heavy lifting or using your arm above shoulder height you may need more time off.
Your surgeon will advise you on how long you will need to be off work; you can ask for a sick note before you leave the hospital.
When can I start my normal activities?
This will depend on the range of movement and strength in your shoulder. It is possible to do most things as long as your shoulder feels comfortable and as your pain allows. Please discuss specific activities with your physiotherapist.
When should I start noticing improvement?
In the first few weeks after surgery your shoulder will be sore, although your movement will be better. Do not be surprised if the soreness affects your daily activities.
You should continue to move and use your arm normally, as your pain allows. Over the weeks following your surgery you will notice a gradual improvement in your movement and pain levels.
Will I have a follow-up appointment?
Before you leave hospital, an appointment will be made for you to have a follow-up appointment at the Upper Limb Unit. You will be seen by a member of the team who will check your progress, make sure you are moving your arm, and give you further exercises as appropriate.
This appointment will usually be four to six weeks after your surgery. You will be monitored by a physiotherapist throughout your rehabilitation.
What if I have any questions or concerns?
If you have any questions or concerns, please contact your surgical care practitioner, surgeon, or physiotherapist. Their contact details are listed at the end of this leaflet.
If you notice your wound area is becoming more painful, red, hot, and / or discharging pus (thick yellow discharge) you may be developing an infection. Contact your GP or your surgical team for advice as soon as possible.
Exercises you can do after surgery, before your first physiotherapy appointment
Before starting the following exercises, please take painkillers and use ice, if needed. It is normal to experience some pain and discomfort when you perform any exercises. If you experience prolonged pain or discomfort when moving, then do the exercises less forcefully or less often. If this does not help, speak to your physiotherapist.
It is best if you do a few short sessions (two to four times a day, for five to 10 minutes each time) rather than one long session. Gradually increase the number of repetitions you do.
Physiotherapy guidelines while you are still in the hospital
An outpatient physiotherapy referral will be arranged by a member of the inpatient physiotherapy team. Outpatient physiotherapy will start within two weeks of your surgery, unless you are told otherwise.
You will be shown how to put on and care for your sling, and how to keep your armpit clean.
You will be given advice on how to manage your pain, including using ice.
You will be shown the following exercises on the ward:
elbow, wrist, and hand exercises
shoulder girdle and posture exercises
shoulder range of movement exercises.
Hand exercises
Open and close your fist 20 times.
Wrist exercises
Move your wrist up and down 20 times.
Forearm exercises
Turn your palm up and down 20 times.
Elbow exercises
Bend and straighten your elbow 20 times. This can be completed with help from your other arm.
Shoulder girdle and posture
Try not to slouch after your surgery.
Try pulling your shoulder blades back and down 20 times.
Pendular exercises
Lean forwards, supporting yourself with your other arm.
Swing your operated arm forwards and backwards gently, like a pendulum.
Do this 20 times.
Shoulder exercises (1)
Lay down and lift your operated arm up, with help from your other arm.
Do this 10 times.
When you are able, do this exercise sitting up.
Shoulder exercises (2)
Gently reach around your back, with help from your other arm.
Hold for 10 seconds.
Repeat three times.
Shoulder exercises (3)
Holding a stick or rolling pin, gently rotate your operated arm out to the side, helped by your other arm.
Repeat 10 times.
Shoulder exercises (4)
Walk your fingers up a wall, you may need to help your hand down with your other arm.
Repeat 10 times.
Isometric static contractions (1)
Gently rotate the operated side out to the side, resisting with your other hand.
Hold for 10 seconds.
Do this three times.
Isometric static contractions (2)
Gently push your operated arm out to the side, resisting with your other hand.
Hold for 10 seconds.
Do this three times.
Isometric static contractions (3)
Gently push your operated arm forwards, resisting with your other hand.
Hold for 10 seconds.
Do this three times.
Physiotherapy guidelines once you leave the hospital
You will be shown further exercises at your outpatient physiotherapy appointment or clinic appointment. If you have any questions, please contact the physiotherapists listed below.
Contact details
Consultants and their secretaries
The teams listed below work at Kent and Canterbury Hospital as well.
| Hospital name | Consultant | Secretary | Contact number |
|---|---|---|---|
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Sathya Murthy | Tracy Blackman | 01843 235068 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Mr Georgios Arealis | Donna Cannon | 01843 235083 |
| William Harvey Hospital, Ashford | Mr Paolo Consigliere | Heather Littlejohn | 01233 616280 |
| William Harvey Hospital, Ashford | Mr Jai Relwani | Dione Allen | 01233 616737 |
| William Harvey Hospital, Ashford | Surgical Care Practitioner | Alphonsa Augustine | 07929 375381 |
Physiotherapists
| Hospital site | Physiotherapist | Contact number |
|---|---|---|
| Buckland Hospital, Dover | Abi Lipinski | 01304 222659 |
| Kent and Canterbury Hospital, Canterbury | Sarah Gillet (inpatient) | 01227 866365 |
| Kent and Canterbury Hospital, Canterbury | Darren Base | 01227 783065 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Caroline Phillipott (inpatient) | 01843 234575 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | Martin Creasey | 01843 235096 |
| Royal Victoria Hospital, Folkestone | Ailsa Sutherland | 01303 854410 |
| William Harvey Hospital, Ashford | Cindy Gabett (inpatient) | 01233 633331 |
| William Harvey Hospital, Ashford | Chris Watts | 01233 616085 |
Surgical Preassessment Units
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783114 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235115 |
| William Harvey Hospital, Ashford | 01233 616743 |
Fracture Clinics
| Hospital site | Contact number |
|---|---|
| Kent and Canterbury Hospital, Canterbury | 01227 783075 |
| Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate | 01843 235056 |
| William Harvey Hospital, Ashford | 01233 616849 |