Flat feet
Information for patients from Trauma and Orthopaedics (T&O)
You have been given this leaflet because you have flat feet. This leaflet will explain:
what the condition is
what your treatment options are
what the risks are to having surgery; and
what happens if I choose not to have this procedure.
We hope this leaflet helps to answer some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
What is flat foot?
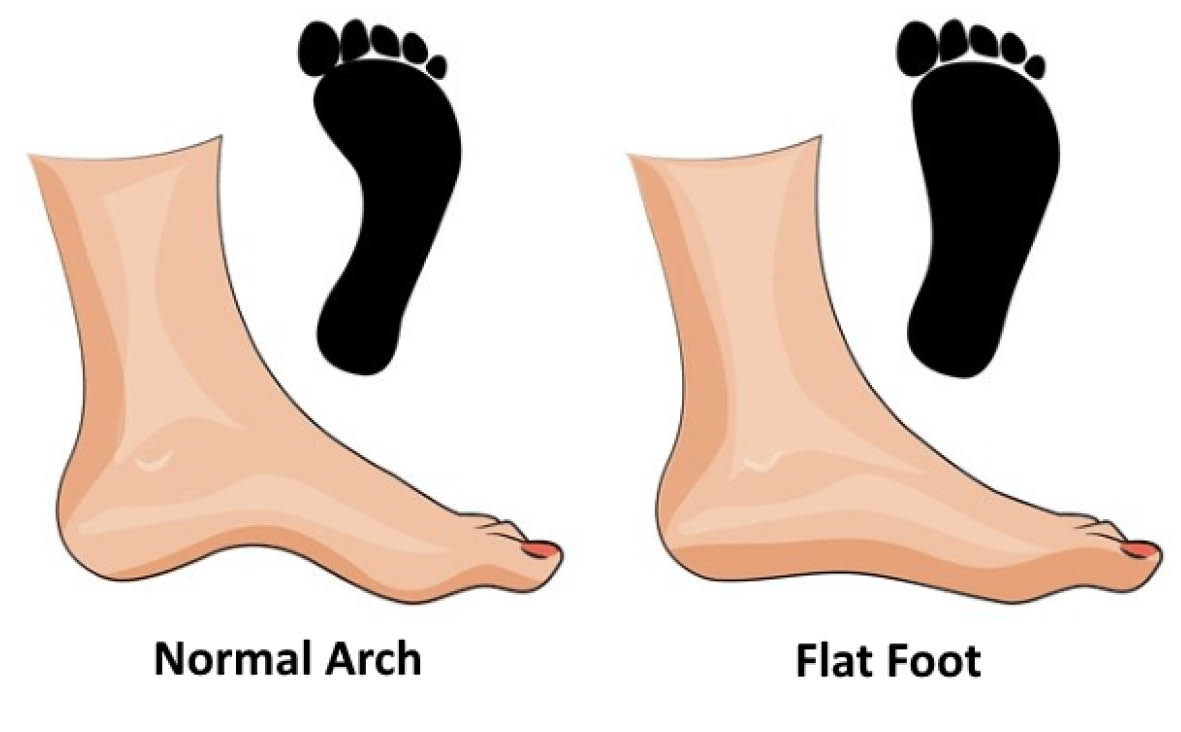
Patients with flat feet do not have a normal foot arch.
This may not cause problems on its own, but it can cause other problems if it progresses. These problems can include:
the toes of the foot turning in
the middle of the foot slanting out
the heel turning out; or
a tight tendoachilles.
What causes flat feet?
Flat feet can be congenital (you have had the problem since childhood) or you may have acquired it. It can also be flexible or rigid.
What are the treatments for flat feet?

In the early stages of acquired flat foot, you can manage your symptoms by:
changing your activities; and / or
using shoe orthotics / insoles.
You should only consider surgery after you have tried the treatments listed above.
What happens during surgery?
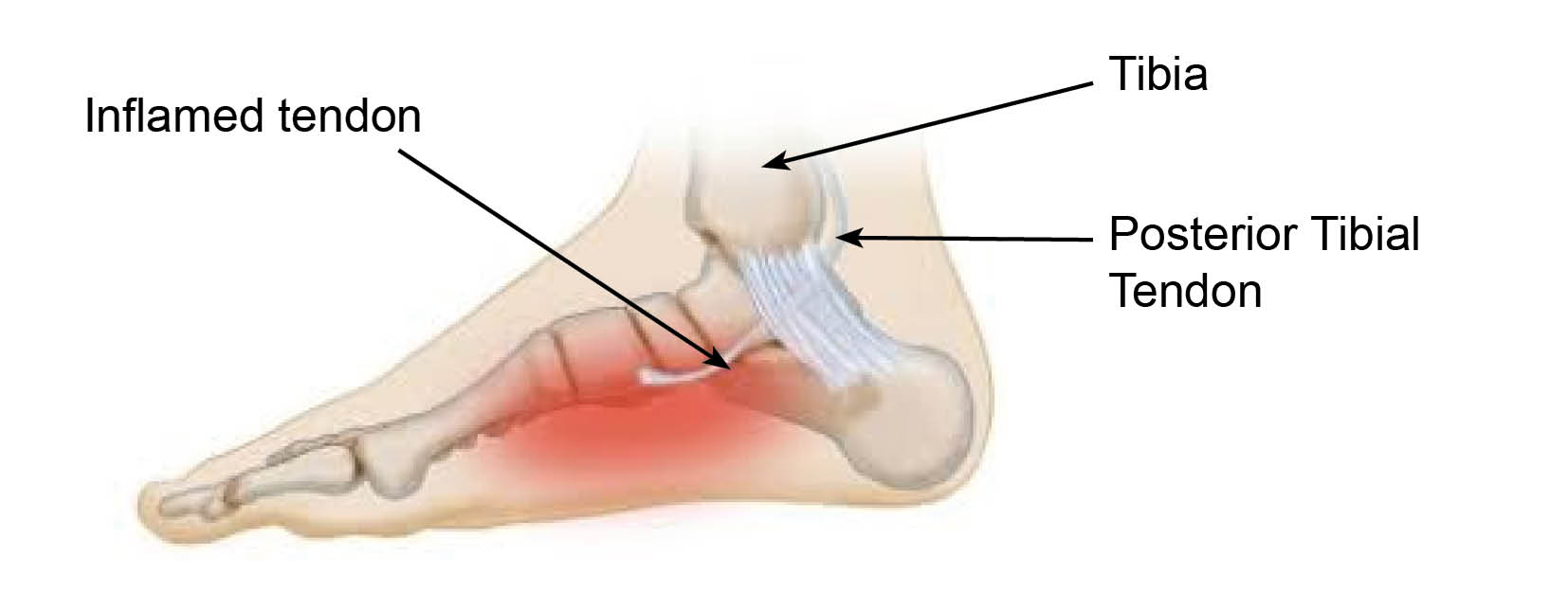
If your posterior tibial tendon is abnormal but your foot remains flexible, the surgeon will cut out the unhealthy tendon and move another tendon to replace it. This may be performed with a calcaneal osteotomy (break in the heel bone and move it inwards).
In more severe cases, if your foot is not flexible you may need a fusion type procedure.
You will discuss these procedures with your surgeon before any treatment is decided. Your surgeon will discuss which is more appropriate for your condition. You will have an opportunity to ask any questions or raise any concerns you may have.
Will I have a general anaesthetic?
Surgery is normally carried out under general anaesthesia (you will be asleep).
You will be told at your pre-assessment appointment:
when to stop eating and drinking
what to do with your medications; and
where to go on the day of your surgery.
What happens if I ignore my condition?
The reason(s) why you came to the appointment may not get better and sometimes can get worse. It is difficult to predict.
How long will I have to stay in hospital?
This surgery is usually performed as a day case procedure (you will able to go home the same day). If you have fusion surgery, you may need to stay in hospital for one night.
You will need someone to drive you home after your surgery, and someone must stay with you overnight.
What happens when I arrive at the hospital?
When you arrive at the hospital you will be seen by the nurses, a physiotherapist, and doctors who will explain your procedure. Please use this time to ask any questions.
You will be asked to change into a hospital gown and stockings.
How will I feel after surgery?
You will be given painkillers to help with any discomfort after your operation. Everyone reacts to the anaesthetic differently. Feeling sick is common, and we do our best to avoid this.
Whilst the pain you felt before your operation should be a lot better, the shape of your foot may not have changed.
What happens after posterior tibialis tendon surgery?
Your foot will be heavily bandaged and you will be fitted with a walking boot before you go home.
One of the healthcare team will give you crutches for support. Please use these as advised by your doctor.
You must elevate (raise) your ankle as much as possible in the first few weeks after your surgery. We recommend you move your ankle as much as possible.
Two weeks after surgery, the walking boot will be removed and your wound is checked.
Physiotherapy will also start at this time.
After the swelling has settled, to protect your foot you may need to wear orthotics.
What happens after tendon transfer and calcaneal osteotomy or fusion procedures?
Your leg will be placed in a below-knee cast for 2 weeks.
Two weeks after your procedure your wound will be checked at the hospital. A complete below-knee cast is fitted for a further 4 weeks.
Do not put any weight on your leg for the first 6 weeks after your operation. A member of staff will give you crutches for support when moving around.
When sitting, you must elevate (raise) your affected leg above your heart level, as much as possible.
After 6 weeks you will be fitted with a walking boot. You can put weight on your affected foot while wearing this boot for a further 6 weeks. You will also start physiotherapy.
After the swelling has settled, to protect your foot you may need to wear orthotics.
When can I start driving again?
This is a difficult question to answer. Your healthcare professionals are not able to take responsibility for this.
You need to check with your insurance company about when they will be willing to insure you to drive again. You must not be in a cast or boot when driving. You must be able to do an emergency stop safely before driving again.
When can I return to work?
When you can return to work depends on the amount of weightbearing needed in your job. If you sit down a lot at work and you can keep your foot elevated, you can return 6 to 12 weeks after your operation. Otherwise you should expect to return to work after 12 to 16 weeks.
What are the risks?
As with any surgery there are risks. Your surgeon will discuss these with you in more detail before your procedure.
Common complications of this type of surgery include the following.
You can expect swelling for up to 6 months, particularly in the evenings.
Infection rates are low, and antibiotics are given before any surgery. If you do develop an infection, this can cause problems.
A skin infection can be managed with antibiotics.
If you develop a deep infection, we may need to remove all the metalwork and unhealthy bone. You will also need a long course of antibiotics.
Nerve injury can result in numbness or tingling across your foot area. This does not usually cause any problems with how your foot works.
Non-union can sometimes happen with fusion surgery. Non-union is when the bones do not join together successfully. There is more risk of this happening in smokers. It may result in pain if the metalwork then loosens. If you smoke, stop before surgery and do not start again until the fusion has healed.
If you need support to stop smoking, please contact One You Kent on 0300 123 1220, or email.
Although rare, metalwork can become noticeable through your skin. This can cause pain from irritation. If this continues, we may need to remove the metalwork.
Stiffness is common after having a plaster cast and using a walking boot. Most patients improve with physiotherapy.
Complex Regional Pain Syndrome (CRPS) can develop when the nerves around the operation site become overly sensitive. Swelling, skin changes, and stiffness can happen and can be debilitating. This is uncommon, but if it does happen it is usually managed by a specialist in pain management.
Deep Vein Thrombosis (DVT) / Pulmonary Embolism (PE) is rare with this surgery. Anticoagulation medication is given after surgery, to try to prevent clots forming whilst you are not able to move your leg. This is a preventative measure, but a clot can still form.
If you have any concerns or questions about any of these risks, please speak with your doctor before your surgery.
What if I have any questions or concerns once I return home?
If you have any questions before your surgery, contact the team secretary through the hospital switchboard.
After surgery you can call the team secretary, the ward, or your GP if you have any further concerns or questions. If you have concerns and cannot get in touch with anyone, go to your nearest Emergency Department.
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email