Factor XI deficiency
Information for patients, parents, and carers from the Haemophilia Centre
What is factor XI deficiency?
Factor XI deficiency is the most common of the rare bleeding conditions that affect blood clotting. It affects around 1 in 100,000 people in the UK.
People with a factor XI deficiency do not bleed any faster, but may bleed for longer than expected.
Having factor XI deficiency should not affect everyday life. Most of the bleeding problems that happen tend to be after an injury, surgery, or dental treatment.
How does factor XI affect clotting?
Factor XI is a protein made by the liver and helps to make your blood clot when there is injury to a blood vessel. If you have factor XI deficiency you do not make enough factor XI for your blood to clot normally, or what you do make might not work as well as it should.
How do you get factor XI deficiency?
Factor XI deficiency is an inherited condition, you are born with it.
One set of our genes is inherited from our mother and the other set from our father. Mutations can happen, which mean the gene is unable to make enough factor XI or that what it does make may not work as well as it should.
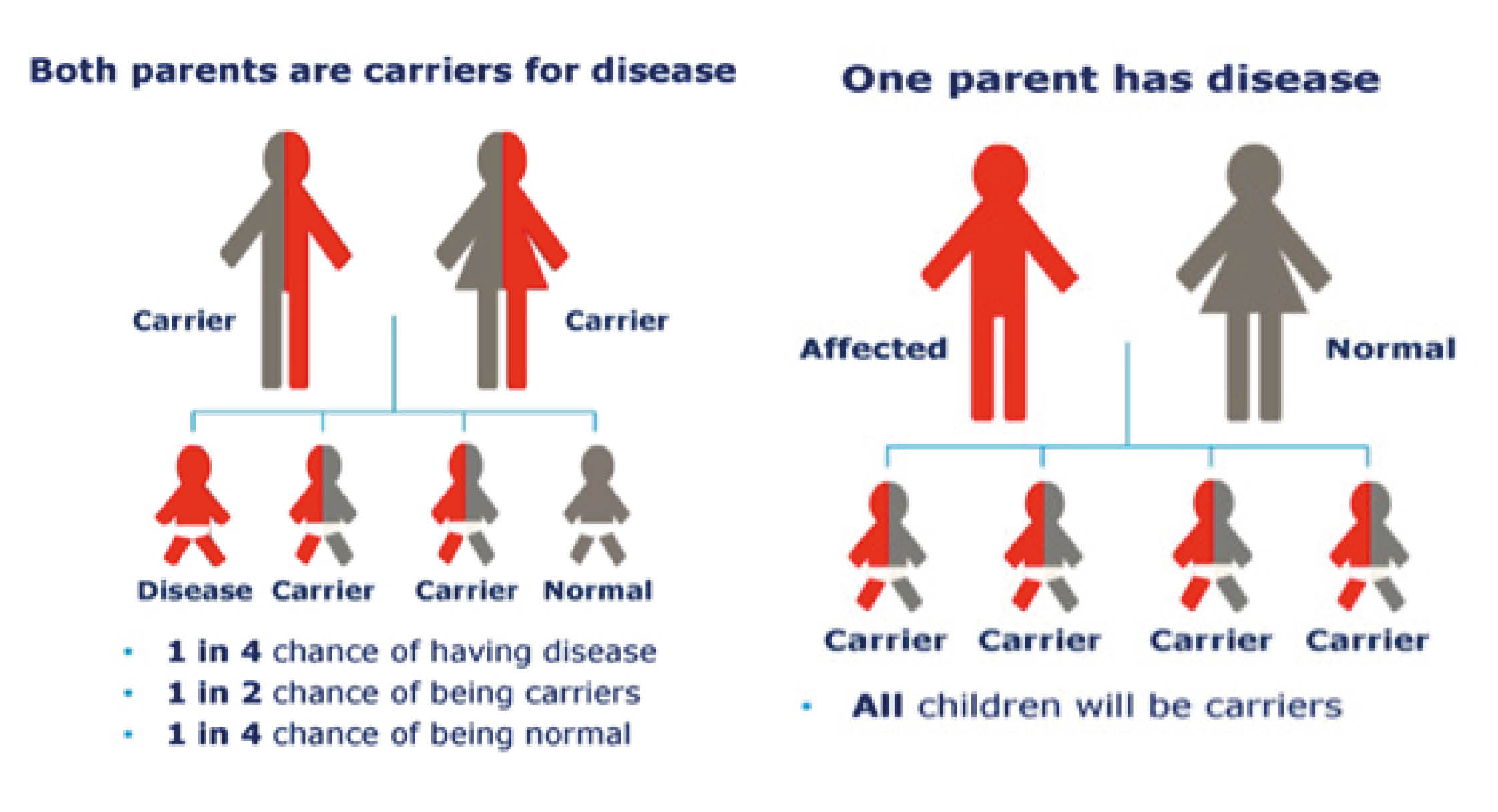
In conditions such as factor XI deficiency people who have one mutated factor XI gene may have a low factor XI level. Where both parents carry the mutated factor XI gene, there is a one in four chance their child will have both mutated factor XI genes and have a more severe factor XI deficiency.
What are the symptoms of factor XI deficiency?
Many people with factor XI deficiency have little in the way of bleeding problems. Spontaneous bleeding (bleeding that happens for no apparent reason) is rare.
With most bleeding tendencies we see that the lower the factor level the higher the risk of bleeding. However, factor XI deficiency is different, some people with a very low factor XI level do not have any bleeding problems, whereas other people with factor XI levels closer to normal have more bleeding problems than someone with a lower level.
Common symptoms
In women and girls, heavy and prolonged bleeding during menstruation (known as menorrhagia)
Nose bleeds
Bleeding from gums
Easy bruising
Bleeding after surgery
Bleeding after trauma or injury
Bleeding in the mother at childbirth.
Rare symptoms
Blood in your urine (known as haematuria)
Bleeding in your stomach or intestines (blood in stools (poo) or black tarry stools)
Bleeding in to your muscle
Bleeding in to your joints (known as haemarthrosis)
Bleeding in to your brain.
How is factor XI deficiency treated?
Day-to-day treatment is not needed for factor XI deficiency. It may however be necessary before and after surgery, dentistry, or trauma.
The need for treatment will depend on:
how severe your bleeding is
the type of surgery or dental treatment you are having
your previous history of bleeding
your family’s history of bleeding; and
your factor XI level.
What are the treatments for factor XI deficiency?
Antifibrinolytic Agents (Tranexamic Acid)
Solvent detergent Fresh Frozen Plasma (FFP)
Antifibrinolytic Agents (Tranexamic Acid)
Tranexamic Acid works by stopping the early breakdown of a clot that has been made after injury to your blood vessel. Fibrin is a protein that gives the blood clot stability. Tranexamic Acid stops the substances that destroy the fibrin within the clot.
Often it is the only treatment needed for some people with factor XI deficiency and for some procedures. It is particularly useful for mouth bleeding and therefore a very good preventative treatment when you are having a dental procedure.
This treatment is usually given as tablets. You may be asked to crush the tablets in a small amount of water and swish it around your mouth, before either swallowing it or spitting it out (you will be advised by the haemophilia team which is best for you).
Tranexamic Acid is not used when there is blood in your urine, as small clots can occur which can then block your urinary tract and cause you pain.
Are there any side effects?
Common side effects are:
nausea (feeling sick) and vomiting
diarrhoea
joint or muscle pain
muscle cramps
headache or migraine
runny or stuffy nose
stomach or abdominal pain.
Other side effects may include skin rash and changes to your colour vision.
Solvent detergent Fresh Frozen Plasma (FFP)
Fresh Frozen Plasma (FFP) is a sterile, frozen solution of pooled human plasma (blood) from several donors, that has lots of clotting factors in it, including factor XI.
As FFP is made from donated blood, there is also an extremely small risk that you may get a blood-borne virus. There are ways in which these risks are minimised by the drug company. The first is that donors are carefully screened to make sure they do not carry these viruses. Secondly, testing for signs of viruses at each donation. And finally, the FFP has been treated with a solvent detergent process to inactivate or remove any possible viruses.
FFP is always given in hospital, either in an outpatient unit or on a ward. It is given to you after thawing through a cannula (a small tube into a vein in your arm) directly in to your vein over one to two hours.
Are there any side effects?
The possible side effects are:
breathlessness
dizziness
chest discomfort
skin itchiness and rashes
headache
tingling feelings.
You will be closely monitored while you are given FFP. If you do have any side effects tell the nursing team straight away.
Where can I find more information about factor XI deficiency?
There are several sources of useful information about factor XI deficiency, including the following.