Expressing breast milk for your baby in the neonatal unit
Information women, birthing people, and their families
Congratulations on the birth of your baby. This information has been produced to help support you with expressing breast milk for your baby whilst they are cared for on the Neonatal Unit.
This leaflet includes information on:
Expressing breast milk.
Storing breast milk.
Bonding squares.
If after reading it you have any concerns or questions, please talk to a member of the team caring for you and your baby.
What are the benefits of breast milk for my baby?
If your baby is born prematurely or is sick, breast milk is like “medicine” that only you can provide.
Colostrum is the early breast milk that your body makes. Breast milk has many benefits, in addition to helping your baby grow.
It helps protect your baby from infection.
It protects a premature baby’s gut from inflammation, known as Necrotising Enterocolitis (NEC). This can be a very serious condition.
It helps baby’s brain, immune system, and lungs to develop.
When should I start expressing breast milk?
Staff will support you to begin hand expressing within the first two hours after birth. You will be encouraged to continue hand expressing at least eight times in 24 hours. This includes during the night. Early and frequent expressing is important. This will help you maximise how much milk you make.
How can I express breast milk?
There are two ways of expressing breast milk:
hand expression; and
breast pump.
You can discuss with your midwife which method is best for you.
Hand expression
Hand expression is a useful technique for everyone to learn. You do not need any special equipment. Hand expression helps increase your milk-producing hormones.
Hand expression is the preferred way in the first 72 hours following birth. Colostrum comes in small amounts. These small amounts are perfect for your baby, but can get lost in a pump.
Before you start expressing, wash your hands with hot soapy water and dry them thoroughly.
It may be useful to massage your breasts before you start to express. This is what babies often do before they breastfeed.
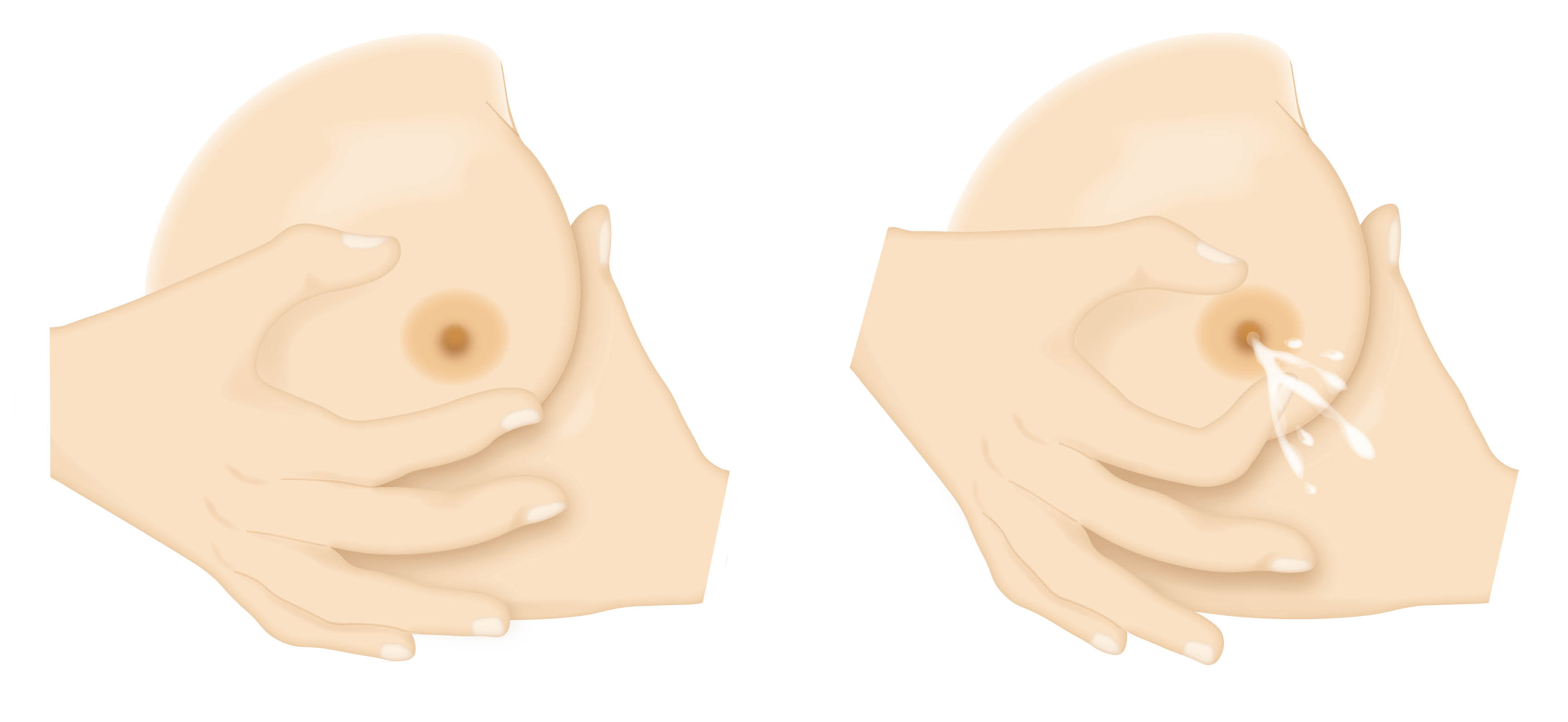
Cup your breast and place your thumb and finger about 2 to 3cm from the base of your nipple (see diagram).
Use your thumb and fingers in a C shape and gently squeeze. Pressure should be firm but not painful.
Release the pressure, and repeat again and again. Avoid sliding your fingers over your skin, as this can cause soreness and may damage skin.
Move your fingers around your breast and repeat on a different part of your breast. Small drops of colostrum should begin to appear. This may take practice and a few tries.
The colostrum can be caught in a small syringe or sterile container, which we will give you to use.
You may find moving your fingers slightly forward toward the nipple or further away may work better for you.
For more information on hand expression, please watch the following UNICEF video.
Breast pump
You may wish to start using a breast pump.
When you are able to hand express volumes greater than 5mls at each expression.
72 hours following birth.
You will be given your own single person use pump kit in the hospital. Pump kits need to be washed with hot soapy water after each use and sterilised before you use them again. Staff will do this for you on the postnatal ward.
Your midwife will be able to help you to use the breast pump.
How often should I use the breast pump?
You will need to express around 8 to 12 times in 24 hours. Aim to pump for around 20 minutes per breast or until the milk flow slows or stops.
The suction strength can be altered on electric pumps. Build up slowly. Setting the strength too high at first may be painful or cause damage to your nipple. There are different funnel sizes available to fit different size nipples. The pump should never cause bruising or catch your nipple as it is sucked into the funnel.
How much breast milk will I express?
It is expected that you will see increases in the amount of breast milk you express over the first eight days.
In the first 24 hours after your baby is born, it is common to get a few drops or around 2mls to 10mls total each time. You might get none the first time.
By the next day you might find this increases to around 5mls to 15mls.
Over the first few weeks the amount you express may stabilise. You may be able to express between 700 and 900mls per day.
There are many reasons that might affect the amount of milk you can express. It is rarely an indication of how much milk you actually make. The focus should be on celebrating every drop, however much you manage to get.
Whilst you are in hospital your midwife will help you use an expressing assessment form. This will make sure that you are expressing effectively. It will also give you the opportunity to speak to staff about any issues. This will be kept with your postnatal notes.
You will be given a daily expressing log to complete and share with your midwife. This will help you to keep track of how expressing is going. You can keep this at your bedside.
Tips to help you maximise the amount of milk you can express
Breast massage and relaxation methods support milk to flow.
Try expressing close to your baby. Look at photos or videos of your baby when you are away from them.
Have a piece of baby’s clothing or a bonding square close by. You can read more about bonding squares further down in this leaflet. This can help with your milk making and flow.
Skin-to-skin contact. If this is not possible, interacting with and caring for your baby will help support an emotional connection. This can increase your milk making hormones.
You may wish to try cluster expressing rather than a strict three to four hourly routine. Cluster expressing means expressing two to three times in a four-hour period. However, avoid long gaps between expressions where possible. Leave no longer than four hours in the day and six hours at night time.
Try to make time to express at least once every night. Night time expression is important. Milk making hormone levels are higher at night. This helps to support long-term milk production.
Double pumping may increase the amount of milk you can express.
Using hand expression and pumps together can increase the amount of milk you express.
Using expressed breast milk in hospital
Expressed colostrum or breast milk is stored in the hospital fridge or freezer. Your expressed breast milk will be kept on the same ward as your baby.
How should breast milk be stored in hospital?
Breast milk can be stored in a sterilised container, breast milk storage bags, or the syringe or pot provided:
in the fridge for up to 24 hours
for two weeks in the ice compartment of a fridge; or
for up to three months in a freezer.
You will be encouraged to take any unused expressed milk home in a cold bag. If you don’t, it will be disposed of by hospital staff in line with the above times.
Never store breast milk in disposable bottle liners or plastic bags that are not intended for storing breast milk.
Defrost frozen breast milk in the fridge, and use within 24 hours.
Store breast milk in small amounts to avoid waste.
Does my breast milk need to be labelled?
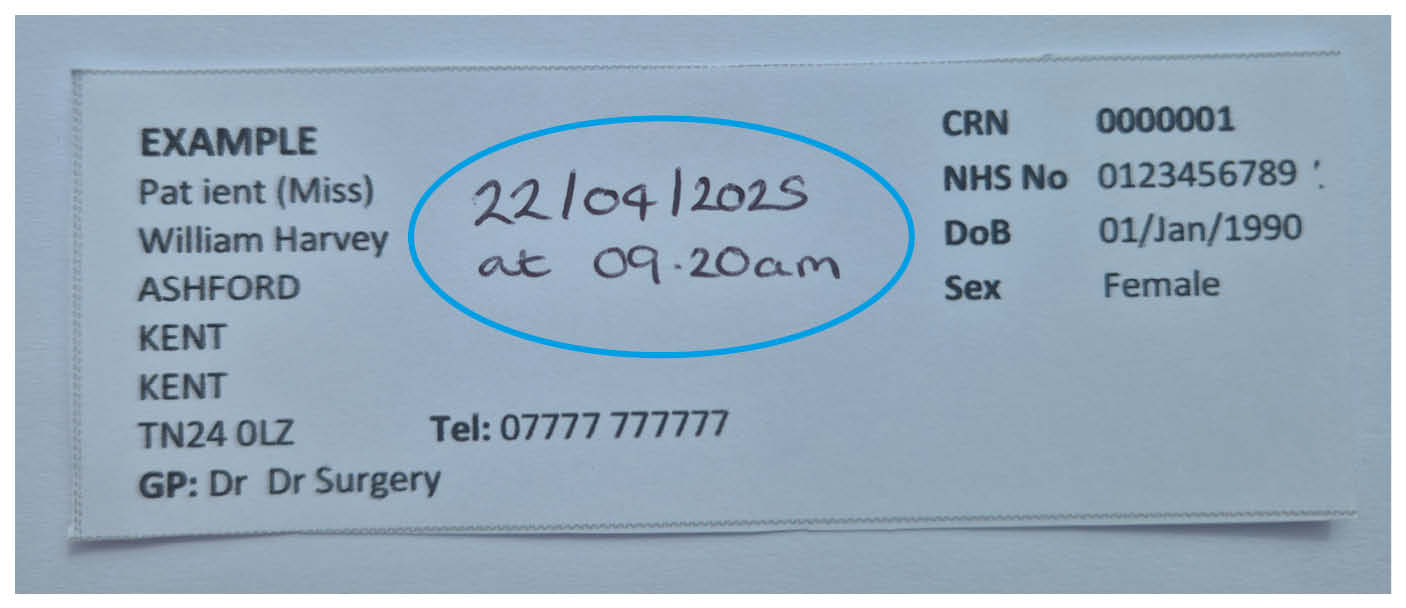
Yes. All expressed breastmilk should be labelled with your patient identification label. Make sure the date and time the milk was expressed is written on the label.
How do I get my expressed milk to the Neonatal Unit?
You can take your expressed milk to the Neonatal Unit. Maternity staff can support you by taking your milk to the Neonatal Unit, if needed. Please make sure it is taken to the Neonatal Unit as soon as possible after it has been expressed.
How do I feed my baby my expressed breast milk?
Staff caring for your baby will talk to you about how your baby will be given the milk you have expressed.
What is a bonding square?

A bonding square is a small piece of fabric, stitched into a shape. They may be square, some will be round or heart shaped. You can wear the bonding square in your clothing, close to your skin. Baby will also have a bonding square close to them. The bonding squares can then be swapped. You will have your baby’s scent and they will have yours.
Why use a bonding square?
Whilst your baby is in the Neonatal Unit you may be separated from them at times. You may not be able to hold your baby as much as you would like. Using a bonding square can support attachment whilst you are away from your baby. Staff on the Neonatal Unit will be able to give you bonding squares to use.
What are the benefits of using a bonding square?
It helps to build a bond between you and your baby.
Familiar scents can be calming for baby. They can help regulate heart rates and reduce stress levels.
It helps you to feel involved in your baby’s care. You will have an active role in the bonding process. This can help support your wellbeing.
Useful information
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email