Expressing and handling breast milk in hospital
Information for women, birthing people, and their families
Congratulations on the birth of your baby. This leaflet has been produced to help support you with breastfeeding your baby.
You have been given this leaflet because your baby is not yet breastfeeding effectively. As well as helping you with expressing, we will support you to maximise your breast milk. This can help you to achieve effective breastfeeding.
This leaflet includes information on:
expressing breast milk
storing breast milk
how your breast milk can be given to your baby.
If you have any questions, please talk to a member of the healthcare team caring for you and your baby.
How can I express breast milk?
There are two ways of expressing breast milk – hand expression or using a breast pump. You can discuss which method is best for you with your midwife.
Hand expression is a useful technique for everyone to learn. It is free and needs no special equipment. Hand expression helps increase your milk-producing hormones.
Hand expression is the preferred way of expressing milk in the first 72 hours following birth. During this time there is only a small amount of colostrum (the first milk). These small amounts are perfect for your baby, but can get lost if you use a pump.
If you and your baby are separated, our staff will support you to begin hand expressing. This should be within the first 2 hours. We will encourage you to continue hand expressing at least 8 times in 24 hours. This should include during the night. Early and frequent expressions help to make sure you are able to maximise how much milk you produce.
Before you start expressing, wash your hands with hot soapy water. Dry them thoroughly.
It may be useful to massage your breasts before you start to express. This is what babies often do before they breastfeed.
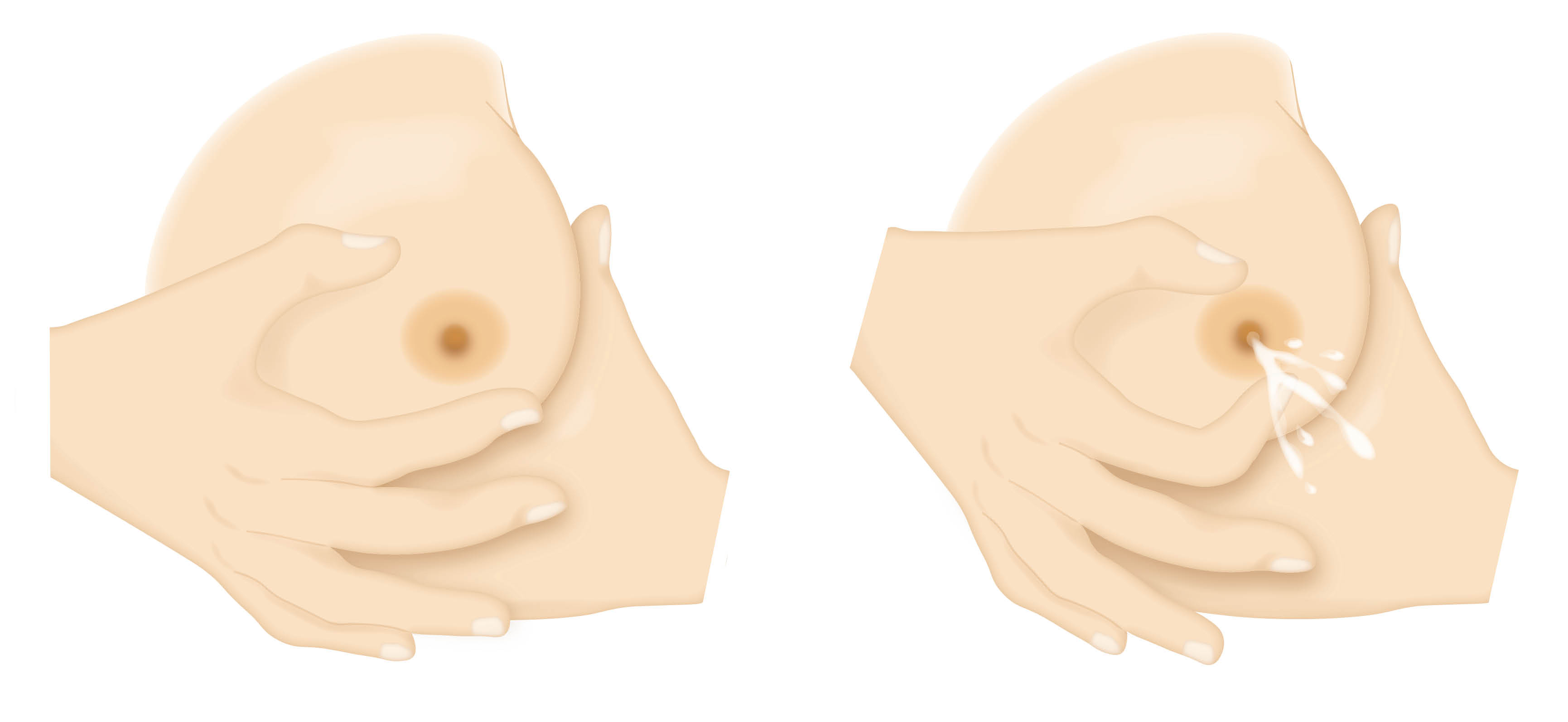
Cup your breast and place your thumb and finger about 2 to 3cm from the base of your nipple (see diagram).
Use your thumb and fingers in a C shape and gently squeeze. Pressure should be firm but not painful.
Release the pressure, and repeat again and again. Do not slide your fingers over your skin, as this can cause soreness and damage to your skin.
Move your fingers around your breast and repeat on a different part of your breast.
Small drops of colostrum should begin to appear, but this may take practice and a few tries.
The colostrum can be caught in a small syringe or sterile container, which we will give to you.
You may find moving your fingers slightly forward toward the nipple or further away may work better for you.
For more information on hand expression, please watch the following UNICEF video.
Breast pump
You may wish to start using a breast pump:
once you are able to hand express more than 5mls of milk at each expression
after 72 hours following birth.
The hospital will give you your own single person use pump kit. Pump kits need to be washed with hot soapy water after each use and sterilised before you use them again. If you use a breast pump in the hospital, staff will wash and sterilise your pump kit for you.
The suction strength can be altered on electric pumps. Build up slowly. Setting the strength too high may be painful or cause damage to your nipple. There are different funnel sizes available to fit different size nipples. The pump should never cause bruising or catch your nipple as it is sucked into the funnel.
Your midwife will be able to help you to use the breast pump.
How much breast milk will I express?
It is expected that you will see increases in the amount of breast milk you express over the first 8 days. To get an increase you will need to express around 8 to 12 times in 24 hours.
In the first 24 hours after your baby is born it is common to get a few drops. Some will get around 2 to 10mls total each time they express. You might get none the first time.
By the next day you might find this increases to around 5 to 15mls.
If you have a healthy term baby this will be plenty. Talk to a member of staff if you:
have any worries
have a baby that was born early, and / or
have a baby that was given an orange or red hat.
Over the first few weeks the amount you express may stabilize. You may be able to express between 700 and 900mls each day.
There are many reasons that might affect the amount of milk you can express. The amount you express is rarely an indication of how much milk you actually make. The focus should be on celebrating every drop, however much you manage to get.
Whilst you are in hospital, your midwife will help you use an expressing assessment form. This will make sure that you are expressing effectively. It will give you the opportunity to speak to staff about any issues.
You will be given a daily expressing log to complete and share with your midwife. This will help you to keep track of how expressing is going.
An assessment form and expressing log can be found at the end of this leaflet.
Tips to help you maximise the amount of milk you can express
Breast massage and relaxation methods support milk flow. They both increase oxytocin, a milk making hormone.
The following can help your milk making and flow.
Try expressing close to baby.
Have a photo or piece of baby’s clothing close by.
Have frequent and prolonged skin-to-skin contact with baby. If this is not possible, interact and care for baby. This will further support an emotional connection and increase your milk making hormones.
You may wish to try cluster expressing, rather than a strict 3 to 4 hour routine. Cluster expressing means expressing 2 to 3 times in a 4 hour period. Where possible, do not have long gaps between expressions; no longer than 4 hours in the day and 6 hours at night.
Try to make time to express at least once every night. Night time expression is important. This is the time that milk making hormone levels are higher. This is very important to support long-term milk production.
The following may increase the amount of milk you express.
Double pumping.
Using hand expression and pumps together.
Using expressed breast milk in hospital
Expressed colostrum or breast milk is stored in the hospital fridge or freezer. When taken from the fridge or freezer, it should be checked with you and a member of staff. This is to make sure the correct milk is being given to the correct baby. The label and your name bands must be compared before using the milk.
How should breast milk be stored in hospital?
Breast milk can be stored in a sterilised container, breast milk storage bags, or the syringe or pot provided:
for up to 24 hours in the fridge
for 2 weeks in the ice compartment of a fridge, or
for up to 3 months in a freezer.
Please take any unused expressed milk home in a cold bag. If you don’t, it will be disposed of by hospital staff in line with the above times.
Do not store breast milk in disposable bottle liners or plastic bags that are not meant for storing breast milk.
Defrost frozen breast milk in the fridge. It can be kept in the fridge for 24 hours.
Store breast milk in small amounts, to help avoid waste.
Once baby has drunk from a bottle of breast milk it should be used within the hour and anything left over thrown away.
Does my breast milk need to be labelled?
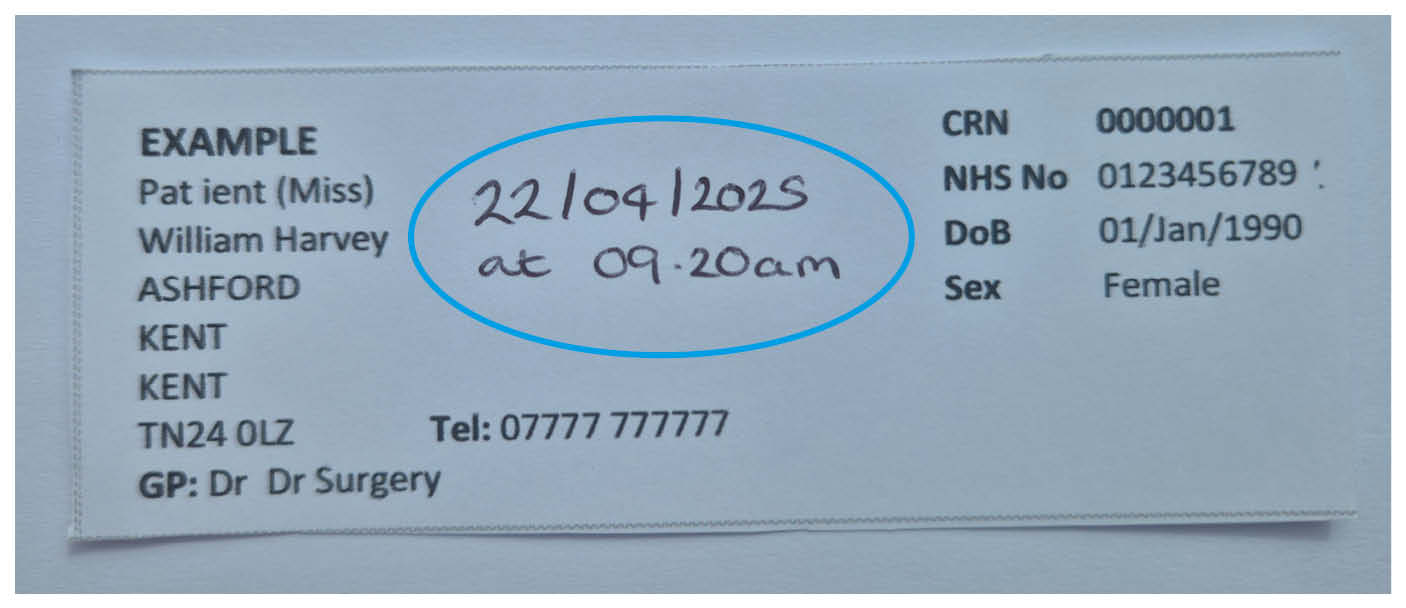
Yes. All expressed breast milk must be labelled with your patient identification label. Make sure the date and time expressed is written clearly on the label.
How do I feed baby my expressed breast milk?
There are different ways you can feed baby your expressed breast milk. Your midwife can help you decide which is the most suitable for you and baby. If baby is on the Neonatal Unit, the team there will be able to discuss the best way for baby to be given your expressed breastmilk.
Syringe feeding
Syringe feeding is a short-term way of feeding baby. It can be used to give your breastmilk to baby when it is in amounts less than 5ml. Syringe fed babies must not be given more than 5ml of breast milk during one feed. If baby needs more than this, a cup or bottle should be used (see below for more information). Staff will show you how to syringe feed safely.
Before using the syringe.
Wash your hands with hot soapy water. Dry thoroughly.
Hold baby in an upright position.
Gently syringe no more than 0.2mls of milk into baby’s mouth at a time.
Feed the milk in between their gum and cheek, or onto their tongue.
Allow baby to swallow before giving them another 0.2mls. Continue to do this until the feed has ended.
Cup feeding
Cup feeding is not recommended for volumes below 5mls.
Baby must be awake and alert to be cup fed.
Make sure baby is calm and not overly hungry when cup feeding begins.
Cup feeding will encourage baby to use their tongue and lower jaw, in a similar way to breastfeeding.
It allows baby to smell and enjoy the milk.
A baby with a tongue-tie may find it difficult to cup feed. Please discuss this with a member of staff.
Before cup feeding
Wash your hands with hot soapy water. Dry thoroughly.
Use a pre-sterilised, once-only cup at each feed provided by the hospital.
Wrap baby securely in a blanket to keep their hands out of the way, so that they do not knock the cup out of your hands.
Sit baby in an upright position on your lap to prevent choking. Place a bib or muslin square around baby’s neck.
Place the cup so that it is gently resting on baby’s lower lip. Do not press it down; the cup should be tipped so that the milk touches baby’s lip.
Wait and baby will sniff the milk, push their tongue forward and start to lap or drink the milk.
Do not tip the milk into baby’s mouth, as this may cause them to choke.
Keep baby sat upright and the cup still. Do not move the cup away when they stop drinking.
Do not cup feed for more than 30 minutes.
Baby will drink at their own pace, with breaks when they need to rest. At the end of the feed they may close their mouth to show that they have finished.
Bottle feeding your expressed milk
You may need to be supported to understand baby’s feeding cues and to hold baby close during feeds. Bottle feeding should be done in a way that is as acceptable and stress free for baby as possible. This also reduces the risk of overfeeding baby.
Offer the bottle in response to feeding cues, gently inviting baby to take the teat.
Pace the feeds. Do not force baby to finish their feed.
Reduce the number of people who give feeds.
Useful information
Potential amounts of expressed milk
| Age of baby | Amount per feed | Volume in 24 hours |
|---|---|---|
| First 24 hours | 2 to 10mls | 38mls |
| Day 2 | 5 to 15mls | 175mls |
| Day 2 to 6 | 15 to 30mls | |
| Day 8 | 650mls |
Expressing Assessment Tool
An assessment should be carried out once within the first 12 hours following birth, and then every 24 hours whilst in hospital. This will make sure that you are expressing effectively. It will also give you the chance to address any issues or concerns.
| Assessment (yes or no) | Assessment (yes or no) | Assessment (yes or no) | Assessment (yes or no) | |
|---|---|---|---|---|
| Date: | ||||
| Time: | ||||
| Number of expressions in 24 hours At least 8 to 10 times in 24 hours, including one in the night. | ||||
| Timing of expressions Timings work around lifestyle - if cluster expressing no gaps longer than 4 hours (day time) and 6 hours (night time). | ||||
| Stimulating milk ejection Uses breast massage, relaxation, skin contact and/or being close to baby. Photos of baby or items of clothing to stimulate oxytocin. | ||||
| Hand expression Confident with technique. Appropriate information provided. | ||||
| Using a breast pump Access to a breast pump. Effective technique including suction settings. Correct breast shield fit, double pumping, or switching breasts to make sure good breast drainage, use of massage/breast compression to increase flow. | ||||
| Breast condition Breast fullness that softens following expression. No red areas or nipple trauma. | ||||
| Milk flow Good milk flow, breasts feel soft after expression. | ||||
| Milk volumes Gradual increases in 24 hour volume at each assessment. See previous page for Potential amounts of expressed milk table. | ||||
| Name and signature of assessor | ||||
| Care Plan documented in notes? Please note page number. |
Expressing Log
Name:
Hospital number:
Date:
Today's total mls (millilitres) expressed in 24 hours:
| Time | How many minutes of expressing | Using pump or hand? | mls expressed (left breast) | mls expressed (right breast) | How are you feeling about it? |
|---|---|---|---|---|---|