Endometrial ablation
Information for patients from Women's Health
Heavy periods (heavy menstrual bleeding / menorrhagia) is one of the most common reasons for gynaecological consultations. Heavy periods can take a physical, social, and emotional toll on a person. It is estimated that heavy menstrual bleeding affects more than 1 in every 5 women, that is about 3.5 million women in the UK [1].
About 1 in 20 women aged between 30 and 49 years speak to their GP each year because of heavy periods or menstrual problems [1]. Endometrial ablation is one of the surgical options to treat heavy periods.
What is endometrial ablation?
Endometrial ablation is a one-time, five-minute procedure. It can lighten or end heavy periods.
The operation will thin or remove the endometrium permanently, to try to treat heavy periods. The endometrium is the inner lining of the uterus or womb.
A tissue biopsy may be taken from the womb lining before or during the ablation. The biopsy is taken to rule out endometrial cancer.
Who can have endometrial ablation?
Endometrial ablation may be suitable for women who have heavy periods, and:
have not been helped by medicines, such as non-hormonal tablets, hormonal tablets, or Mirena coil
do not wish to try medicines; or
do not wish to have children in the future.
Endometrial ablation is not for women who:
have or are suspected to have uterine cancer; or
currently have a genital, urinary, or pelvic infection.
Endometrial ablation is not a sterilisation procedure.
What if I want to get pregnant in the future?
Endometrial ablation involves destroying the inner lining of the womb, so we do not recommend this treatment if you wish to become pregnant in the future. Getting pregnant after this procedure can be dangerous for both mother and baby.
The treatment is not a contraceptive, so you still need to use contraception after your procedure. Please discuss your contraceptive options with your doctor before treatment.
Are there alternatives?
The following are alternatives to endometrial ablation. If you have any concerns or questions, please speak to your surgeon.
Hysterectomy is a surgical procedure that removes the uterus. For more information, please read the Hysterectomy leaflet.
Success rate: 100%
Advantages
Eliminates problem bleeding.
One-time procedure.
Permanent.
Disadvantages
Cost, major invasive surgery.
Risks associated with major surgery.
Patient has a general anaesthetic.
2 to 8 week recovery time.
Non-reversible, lose fertility.
Many cause early onset of menopause.
Typically the last option for women who have not responded to other treatments.
Mirena coil. The coil is placed in the uterus to prevent pregnancy for 5 years. It can also decrease heavy menstrual blood loss.
Success rate
67 in every 100 women (67%) notice a reduction in normal bleeding after 1 year.
20 in every 100 women (20%) have no bleeding after 1 year.
Due to their symptoms returning, after 5 years 42 in every 100 women (42%) choose to have a hysterectomy.
Advantages
Effective for 5 years.
Reduces / eliminates problem bleeding.
It is also a contraceptive.
Fertility returns after the coil is removed.
Disadvantages
Mirena may take up 6 months to provide relief from heavy bleeding.
3 in 10 women (30%) have hormonal side effects.
7 in 10 women (70%) have bleeding between their periods.
Mirena needs to be replaced every 5 years.
Tranexamic acid tablets help to normalise clot breakdown in the uterus.
Success rate
66 in every 100 women (66%) report a third reduction in menstrual blood loss.
Advantages
Non-invasive treatment.
Tablet taken by the patient (self-administered).
Remain fertile while taking tablets.
Disadvantages
The patient must take 2 tablets, 3 times a day.
Using alongside other hormonal products may increase the chance of blood clots, stroke, or heart attack.
Will not stop menstrual bleeding.
Source: Hologic Novasure® Endometrial Ablation
What if I choose not to have any treatment?
If you decide to have no treatment and just monitor your symptoms, you will see no change until you reach menopause. The average woman reaches menopause at 51 years.
Does endometrial ablation work?
Eight in 10 women (80%) treated are satisfied or very satisfied with their results following treatment. Most women have lighter periods, and around 1 in 3 women have no periods at all. [1]
There is a chance that the inside lining of the womb can re-grow after this procedure. As a result, 1 in 10 women (10%) may need another medical or surgical treatment after 2 years. [1]
How does ablation work?
At our Trust, we offer two methods of endometrial ablation.
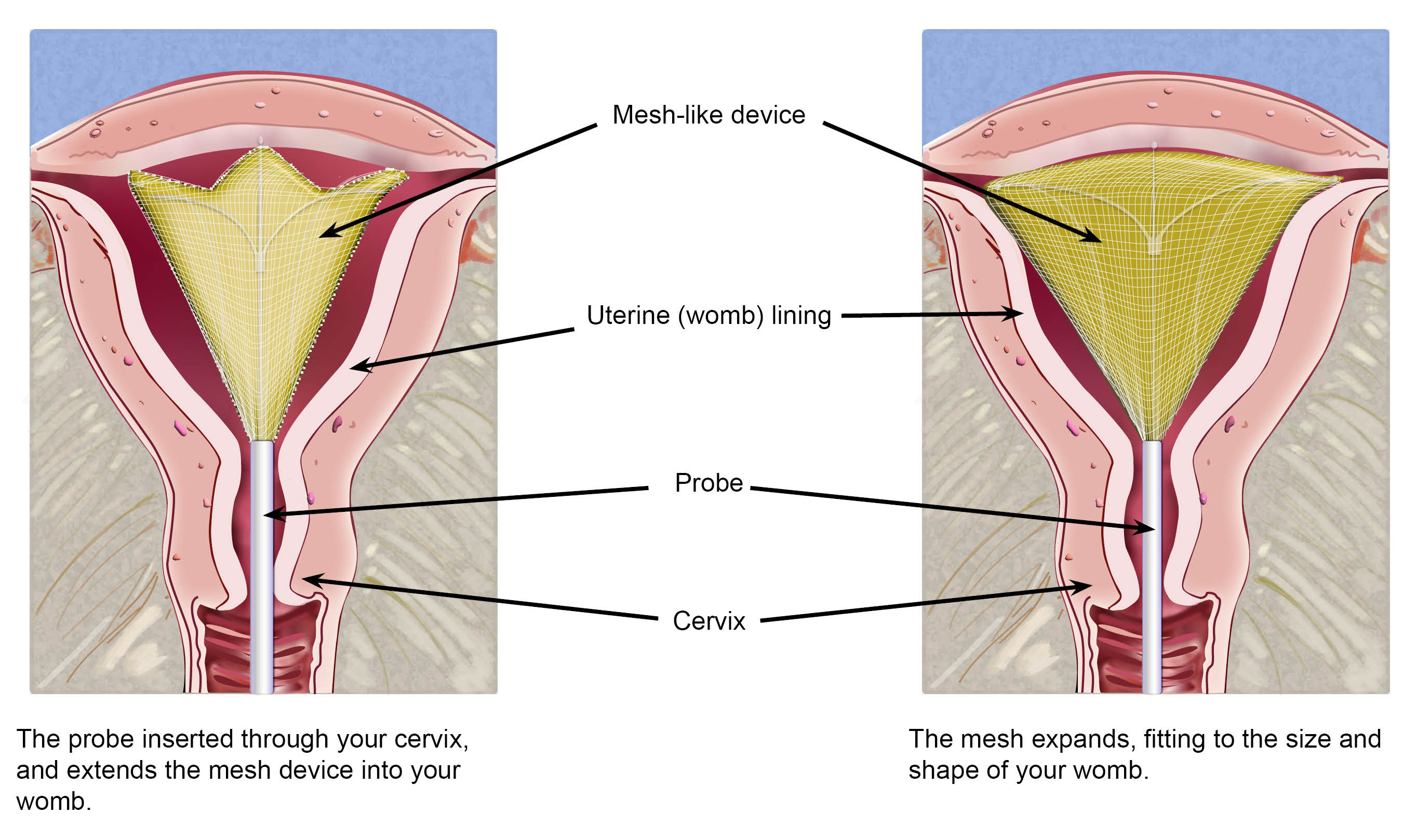
1.NovaSure® radiofrequency ablation
A probe is inserted inside the womb.
The tip of the probe expands into a mesh-like device, that delivers radiofrequency energy into the lining of the womb. The womb is preserved and not affected by the energy, only the inside womb lining is melted away.
The treatment takes around 5 minutes to complete.
2.Thermablate uterine balloon system
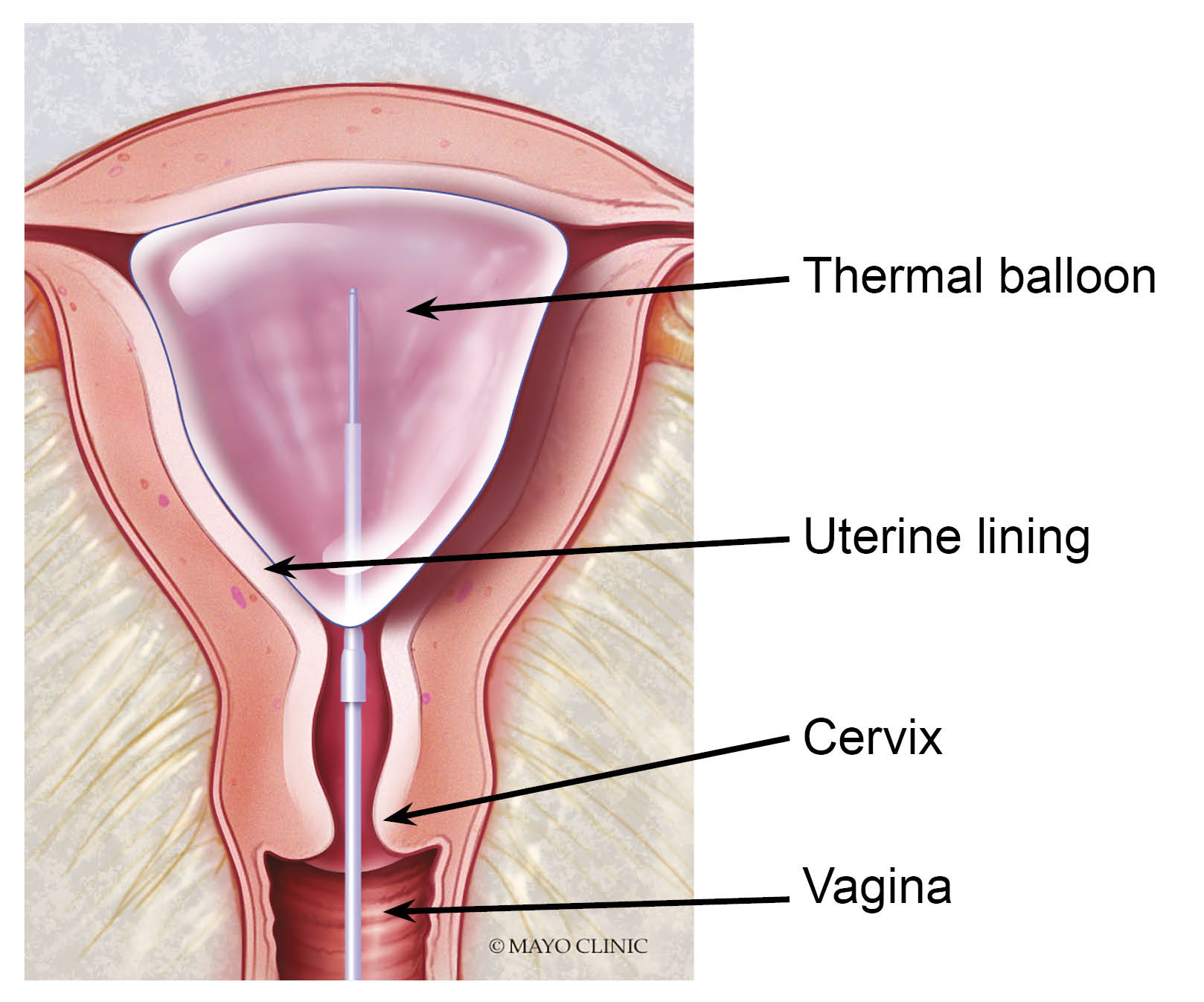
A soft balloon attached to a thin catheter (tube) is inserted into your vagina, through the cervix and placed gently into your uterus.
The balloon is inflated with a sterile fluid. It expands to fit the size and shape of your uterus.
The fluid in the balloon is heated to 87 degrees celsius (188 degrees fahrenheit). It is kept at that temperature for 2 minutes and 38 seconds, while the uterine lining is treated.
When the treatment is complete, the fluid is withdrawn from the balloon and the catheter removed. Nothing stays in your uterus.
Your uterine lining has been treated. It will come away like a period in the next 7 to 10 days.
Both of these options will be discussed with you before your procedure.
What are the benefits to having endometrial ablation?
The procedure is quick. It usually takes less than 5 minutes.
For 91 in every 100 women (91%) menstrual bleeding reduces or stops within 1 year. 41 in every 100 women (41%) report that their periods stop completely. [1]
97 in every 100 women (97%) report that they had no pelvic pain after their procedure. [1]
There are no cuts made during the procedure.
Endometrial ablation can be performed at any time during your menstrual system. Patients can have the procedure even if they are bleeding.
Patients do not need to take any medication before the procedure.
It's a one-time procedure. It does not need to be repeated.
What are the risks?
NovaSure® radiofrequency ablation and Thermablate uterine balloon system both carry very small risks. The risk of a person experiencing one of the following is less than 1 in 10,000 (0.01%). [1]
Womb infection.
Excessive bleeding from the womb.
Making a small hole in the wall of the womb (called uterine perforation).
Bradycardia (an abnormally slow heart beat).
Burn or thermal injury to nearby tissue.
Very small risk of injury to the bowel, bladder, or major blood vessels. If any injury is suspected, your surgeon may perform another procedure called a laparoscopy. A laparoscopy will check and repair any damage. A laparoscopy involves inserting a special thin telescope into your belly button, to check your pelvic organs. For more information, please read the Laparoscopy leaflet.
Tell your doctor if you have cardiac pacemaker or any other electrical device in your body.
How long will I be in hospital?
If you have had a general anaesthetic, you will usually need to stay in hospital for 3 to 4 hours after your procedure. This is to make sure you are fully awake and comfortable before you go home.
Will I have a general anaesthetic?
The procedure can be performed under:
general anaesthetic (you are asleep); or
local anaesthetic (you are awake but the area is numbed).
Your doctor may use local anaesthetic to numb your cervix and uterus. You will discuss these options with your anaesthetist before your procedure.
How will I feel after my endometrial ablation?
Immediately after their procedure, some women have cramping, mild pain, nausea, and / or vomit.
After one day of rest, most women return to their normal activities, including work and exercise.
A watery and / or bloody discharge following the procedure is normal. This can start immediately after the procedure, or a couple of weeks later. The discharge may last only briefly, or for up to a month.
Effects of having general anaesthetic
During the first 24 hours, you may feel more sleepy than usual and your judgement may be impaired. This should not last for more than 24 hours. You must not drive for 24 hours after a general anaesthetic. If you are having a general anaesthetic, please arrange for someone to take you home from hospital. If this is not possible, please tell a member of hospital staff.
Vaginal discharge and bleeding
You can expect some vaginal bleeding for a few days after your procedure, usually like a light period. The bleeding will gradually lessen and become like a heavy discharge, and may darken in colour. For some women, this discharge can last for 3 to 4 weeks. Use sanitary towels rather than tampons, as tampons can increase your risk of infection.
Pain and discomfort
You can expect some cramps (similar to period pains) in your abdomen for a day or so after your operation. Most women will not need to take painkillers after this time. It is a good idea to have some simple pain relief, such as paracetamol or ibuprofen, at home just in case. Please refer to the patient information that comes with the painkillers, for advice on how many you can take.
Painkillers that contain Codeine can make you sleepy, slightly sick, and constipated. If you do need to take these medications, eat extra fruit and fibre to reduce the chances of becoming constipated.
When will I know what my periods will be like after the procedure?
Every woman is different. Plan to give your body about 3 months to fully heal on the inside and resume its normal cycle. After this time, you and your doctor should be able to tell what your cycle and your periods will be like from that point on.
When can I eat and drink again?
If you have had a general anaesthetic. Once you are awake you will be offered a drink of water or cup of tea, and something light to eat before you go home.
If you have had a local anaesthetic. You will usually be able to eat and drink as normal following your operation.
What can I expect after I go home?
After one day of rest, most women return to their normal activities, including work and exercise.
Most women have a pinkish and watery vaginal discharge for a few days after their procedure. This can sometimes last for a month.
You can have sex again after the bleeding or discharge settles, and you feel comfortable.
In some cases, the first few periods after the procedure may continue to be heavy but will begin to improve after that.
When should I ask for medical advice after an endometrial ablation?
Very few patients have complications following this procedure. But, call Day Surgery immediately if you develop any of the following symptoms.
A fever higher than 100.4°F.
Worsening pelvic pain, that is not relieved by ibuprofen or other prescribed medicine.
Nausea (feeling sick), vomiting, shortness of breath, and / or dizziness.
Bowel or bladder problems.
A greenish vaginal discharge (red, yellow, or brown discharge is normal).
Source: Hologic. Is your heavy period affecting your life? NovaSure Endometrial Ablation.
If an infection is suspected, the treatment is usually a course of antibiotics. Occasionally, you may need to come back to hospital, where the antibiotics can be given as a drip.
Contact details
Canterbury Day Surgery Centre, Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783114 (7am to 8pm)Day Surgery, Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234499 (Monday to Friday 7am to 9pm)
Telephone: 07887 651162 (Monday to Friday 9pm to 7am) (Bank Holidays and weekends, 24 hours a day)Channel Day Surgery, William Harvey Hospital, Ashford
Telephone: 01233 616263 (24 hours a day, 7 days a week)
References
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email
We have used the terms ‘women’ and 'mother' throughout this leaflet. When we use these terms we also mean people with female reproductive organs who do not identify as a woman or mother. East Kent Hospitals is committed to supporting people of all gender identities. Please tell your doctor how you would like them to address you, so we can be sure to get this right.