Endo-venous radiofrequency ablation (RFA) of varicose veins
Information for patients from the Vascular Surgery Department
Your surgeon has suggested endo-venous radiofrequency ablation (RFA), an operation to treat your varicose veins. This leaflet provides information about the benefits and risks of RFA, to help you make an informed decision about your treatment. If you have any questions that this leaflet does not answer, it is important that you ask your surgeon or your healthcare team. Once all your questions have been answered and you feel ready to go ahead with the procedure, you will be asked to sign a consent form. This is the final step in the decision-making process. However, you can still change your mind at any point.
What are varicose veins?
Varicose veins are enlarged veins in your leg. They are common, affecting up to three in 10 people and can result in leg ulcers. Varicose veins tend to run in families, and are made worse by pregnancy and if you do a lot of standing.
-
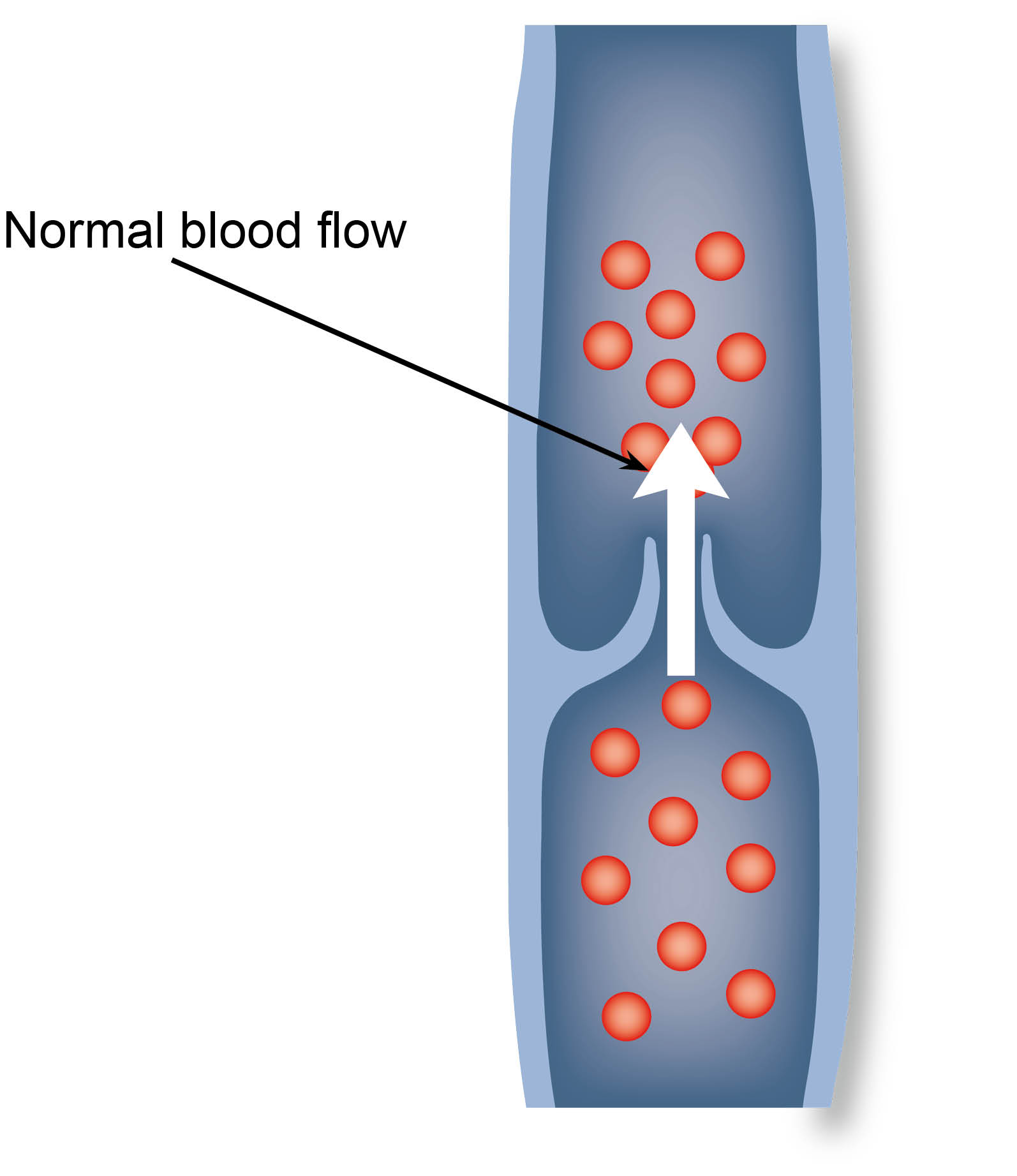 Normal blood flow in a vein
Normal blood flow in a vein -
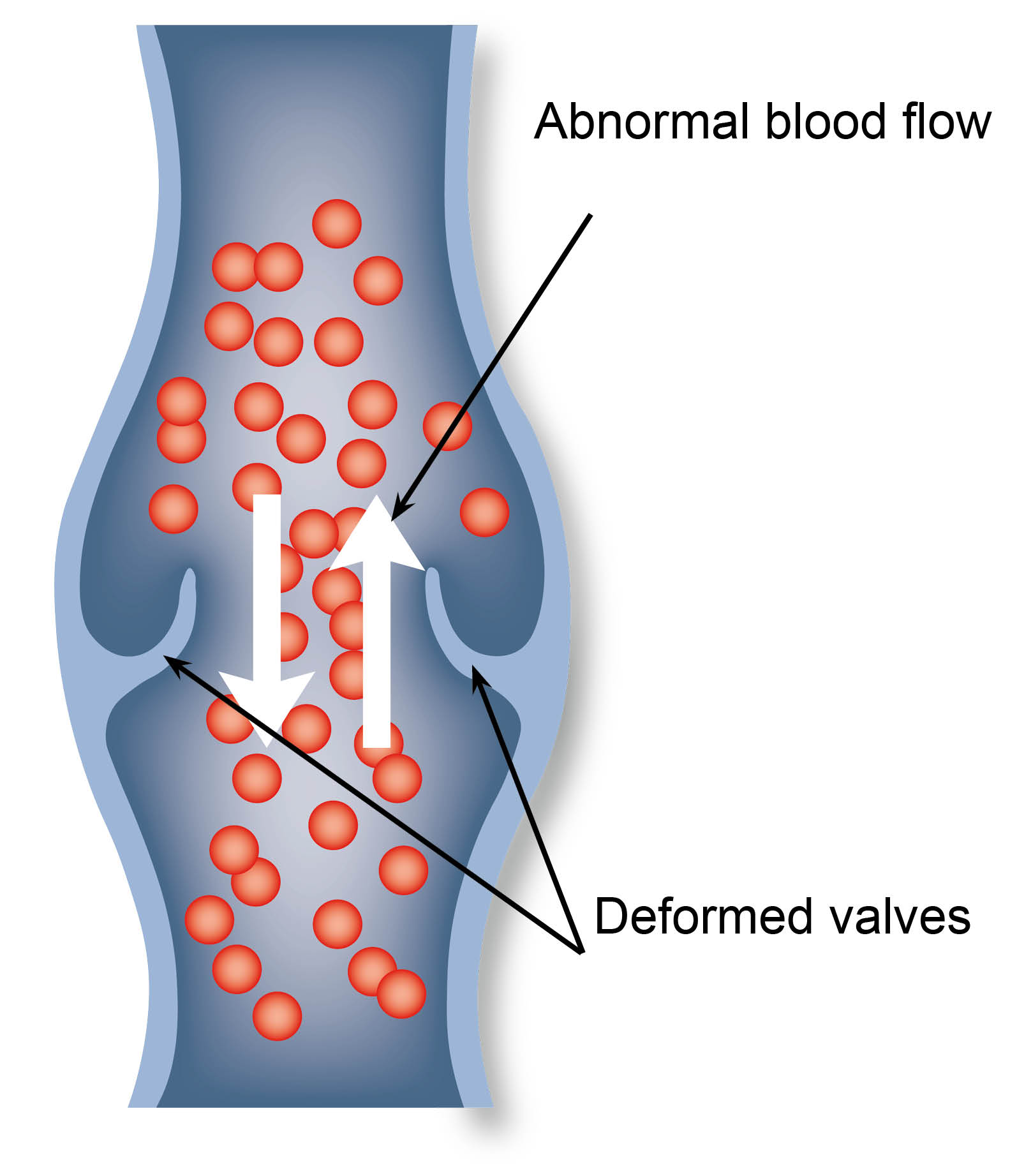 Abnormal blood flow and deformed valves in a vein
Abnormal blood flow and deformed valves in a vein
How are varicose veins treated?
Your treatment options for varicose veins may include the following.
Conservative measures may help prevent your condition from getting worse. These include:
Losing weight, if you are overweight or obese.
Elevating (raising) your legs, whenever possible.
Avoiding tight fitting clothes.
Avoiding long periods of standing and sitting.
Compression stockings are usually the first treatment to be used. The stockings are worn all day. They squeeze your legs and help the leg veins and muscles to circulate blood more effectively.
The following are the treatment options for severe varicose veins, when the treatment options listed above have not worked.
Sclerotherapy is an injection which destroys the inner lining of the vein and converts it into a thick fibrous cord. For more information on sclerotherapy, please ask a member of staff for a copy of the Trust leaflet Injection sclerotherapy for varicose veins.
Radiofrequency ablation (RFA).
Ambulatory phlebectomy, which is the removal of the affected veins during surgery.
What can happen if I decide not to have treatment for my varicose veins?
Your legs and veins can look unsightly.
Varicose veins can cause itching, aching, and pain in your legs.
Pigmentation (dark discolouration) of the skin can develop around your ankle.
You may develop an infection in your skin (cellulitis).
Your veins can become inflamed (phlebitis).
Ulcers (or sores) can develop on your legs.
Your varicose veins may bleed.
What are the benefits of RFA surgery?
Your symptoms should improve.
RFA should help prevent the symptoms and complications that varicose veins cause.
RFA will not remove fine thread veins. The NHS does not offer cosmetic treatment.
What should I do before my surgery?
Make sure you tell your healthcare team about all the medication you take, and follow their advice on which medication you should continue to take after your surgery. This includes all blood-thinning medication as well as herbal and complementary remedies, dietary supplements, and medication you can buy over the counter.
In the week before your operation, do not shave or wax the area where a cut is likely to be made.
Take a bath or shower either the day before or on the day of your operation.
If you are diabetic, keep your blood sugar levels under control around the time of your procedure.
If you have not had the coronavirus (Covid-19) vaccine, you may be at an increased risk of serious illness related to Covid-19 while you recover. Speak to your doctor or healthcare team if you would like to have the vaccine.
What can I do to help make my operation a success?
If you smoke, stopping smoking now may reduce your risk of developing complications after your surgery and will improve your long-term health. If you need support to stop smoking, call One You Kent on 0300 123 1220, or email.
Try to maintain a healthy weight. You have a higher risk of developing complications after surgery if you are overweight.
Regular exercise should help to prepare you for your operation, help you to recover afterwards, and improve your long-term health.
If you are taking the oral contraceptive pill or hormone replacement therapy (HRT), you should consider stopping taking these tablets four weeks before your operation. This is to reduce your risk of developing a deep vein thrombosis (DVT). If you do stop taking your oral contraceptive pill, you will need to use a different contraceptive.
What happens before my operation?
.jpg)
Before your operation, you will have a Doppler ultrasound scan (Duplex scan) of your legs.
What does the operation involve?
Your surgeon may need to mark the veins on your leg. The healthcare team will carry out a number of checks to make sure you have the operation you came into hospital for, and that the surgery is on the correct side.
The procedure usually takes about 30 minutes and is performed under local anaesthetic (the area is numbed but you will be awake).
-
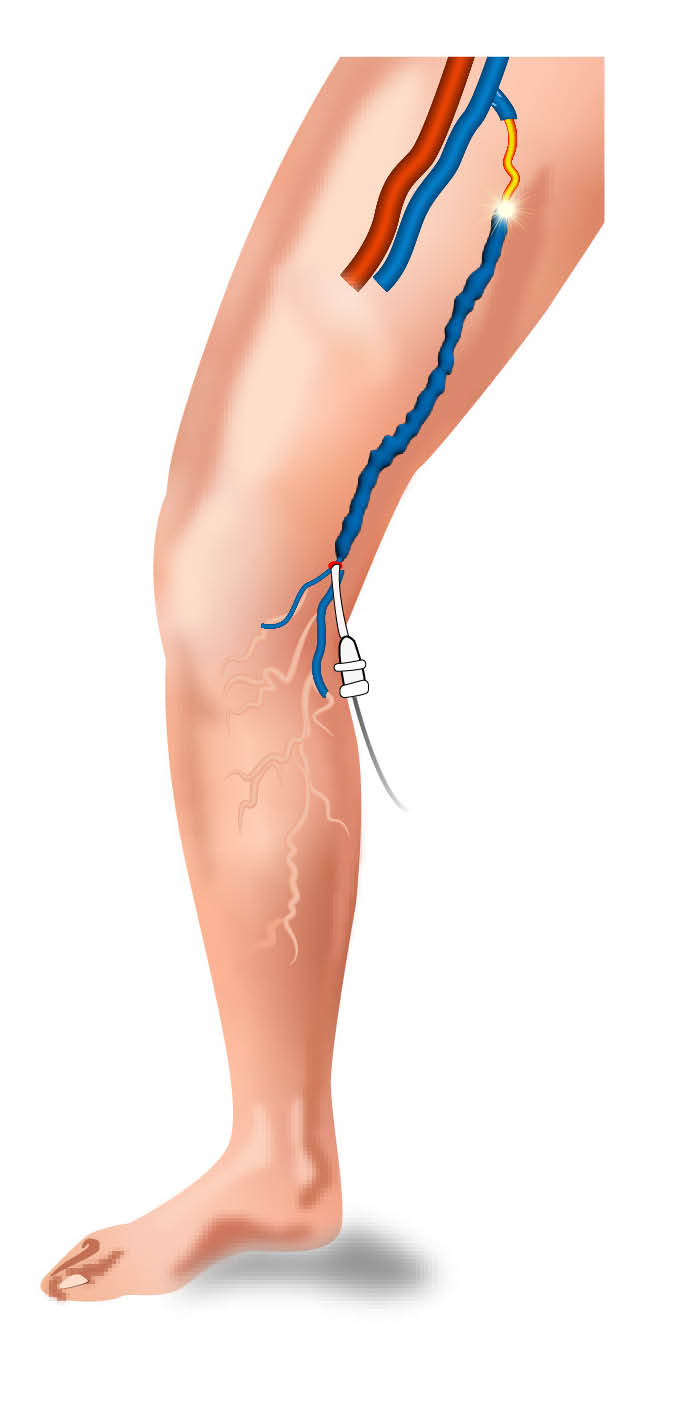 Disposable catheter inserted into greater saphenous vein
Disposable catheter inserted into greater saphenous vein -
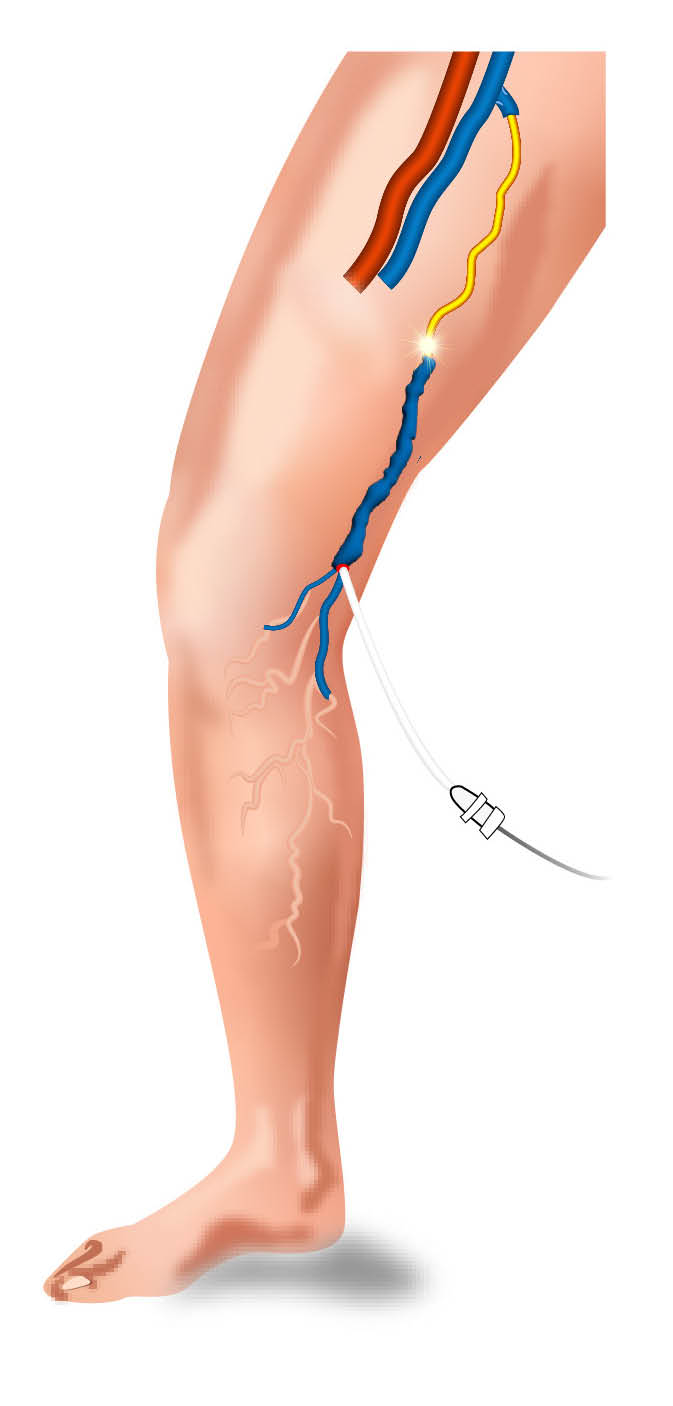 Veins heats and collapses
Veins heats and collapses -
 Catheter withdrawn, closing vein
Catheter withdrawn, closing vein
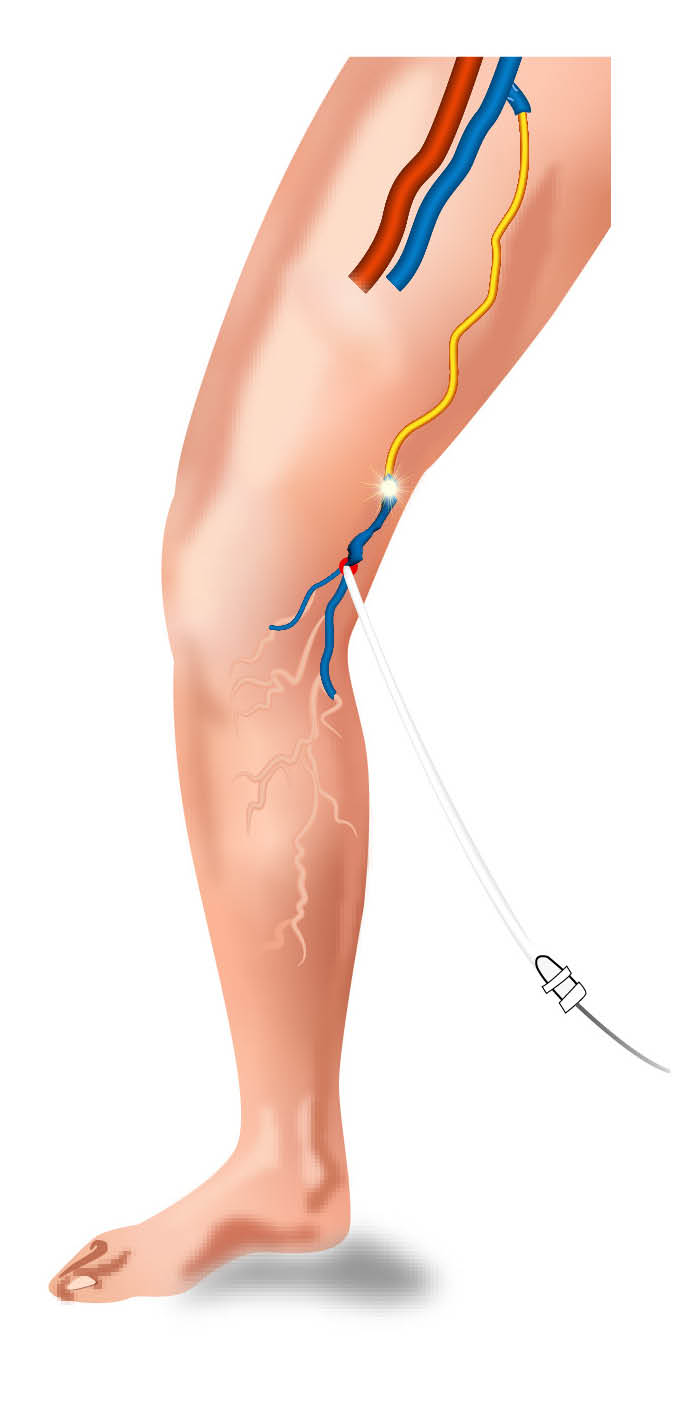
RFA is done by inserting a radiofrequency ablation catheter into the great or small saphenous vein.
Surgeons will use an ultrasound scan as a guide, to move the catheter to the point where the saphenous and deep veins meet.
They will inject a local anaesthesia to numb the area and compress the walls of the vein onto the catheter.
The catheter has an electrode that heats the walls of the vein using radiofrequency energy. Your surgeon will slowly remove the catheter while radiofrequency energy is sent down the electrode. The radiofrequency energy causes the saphenous vein to close.
During your operation, your surgeon may need to remove other varicose veins through small cuts, or close some veins using injections.
After surgery, you will be given a compression bandage or stocking to wear.
What are the possible complications of RFA?
Bleeding during or after your operation.
It is common for your leg to be bruised. You may also feel a lump under your wound. This is caused by the bruising and settles within a few weeks.
A haematoma may develop. This is a lump under your wound caused by blood collecting in the area. This develops in three in 100 patients.
Pain is usually controlled with simple painkillers, such as paracetamol.
One in 100 patients will develop a wound infection. Let the healthcare team know if you get a high temperature, notice pus in your wound, or if your wound becomes red, sore, or painful. An infection usually settles with antibiotics, but you may need special dressings and your wound may take time to heal. In some cases another operation might be needed. Do not take antibiotics unless you are told you need them.
An allergic reaction to the equipment, materials, or medication. Let your doctor know if you have any allergies or if you have reacted to any medication or tests in the past.
Deep vein thrombosis / DVT (heat-induced thrombosis) happens to between one and five in every 100 patients). This can cause pain, swelling, or redness in your leg, or the veins near the surface of your leg appear larger than normal. Let the healthcare team know straightaway if you think you might have a DVT.
A blood clot in your lung (pulmonary embolus) may develop if a blood clot moves through your bloodstream to your lungs. If you become short of breath, feel pain in your chest or upper back, or you cough up blood call an ambulance (if you are at home) or go immediately to your nearest Emergency Department.
If you have your operation within six weeks of catching Covid-19, your risk of developing a chest infection is increased pain.
Up to two in 100 patients will have numbness or a tingling along the vein that has been treated. This usually improves after a few weeks.
Burns to your skin happen to less than one in every 100 patients. This is unusual as your surgeon uses fluid to protect your skin.
The ablation device may crack or break. If this happens your surgeon will need to make a cut on your leg to remove the broken device. This affects less than one in 1000 patients.
If the nerve to your foot is damaged (peroneal nerve) you may have difficulty walking. You may also have numbness or burning in the skin over your shin. This affects less than one in 1000 patients.
If your arteries are damaged you may need another operation. This affects less than one in 1000 patients.
Recurrence, your varicose veins may occur again. start exercising again speak to your healthcare team or GP for advice.
What happens after my operation?
After your operation you will be taken to a ward. You should be able to go home the same day.
What happens when I go home?
You should be near a telephone in case of an emergency.
Do not drive, operate machinery or do any potentially dangerous activities (this includes cooking) for at least 24 hours and not until you have fully recovered feeling, movement, and co-ordination. After this 24 hour period, do not drive again until you can control your vehicle (including an emergency stop), you have checked your insurance policy, and you have spoken to your healthcare team. Do not drive while you are taking painkillers that make you drowsy.
To reduce your risk of developing a blood clot, make sure you carefully follow the instructions of your healthcare team. This includes making sure you are drinking enough and not getting dehydrated, being active, and wearing the compression stockings for two weeks.
When you go home you may have bandages on your legs. Keep the bandages dry for 24 hours before removing them.
You may need to wear support stockings during the day for two more weeks, removing them when you go to sleep.

Once at home, move around as much as possible and try to return to your normal activities, unless you are told otherwise. Regular exercise should help with your recovery, but before you start exercising again speak to your healthcare team or GP for advice.
When you are resting, keep your legs raised on a stool.
It is usually safe to shower two days after surgery, but check with your healthcare team first.
How will I feel after my surgery?
Most people make a full recovery after RFA.
Any aching, swelling, or discomfort caused by the operation should gradually improve over the first six weeks.
If you had surgery for ulcers, these should gradually heal.
Any skin pigmentation will stay but is less likely to get any worse.
You will notice that your varicose veins have gone as soon as the support stockings or bandages are removed.
Varicose veins can come back, either in the same place or in other parts of your leg. This happens to three in 10 patients within five years of surgery.
Contact details
If you have any concerns or questions about anything either in hospital or at home, please contact your healthcare team (during the working day, ask to speak to one of the vascular nurses).
Vascular Nurse Practitioners, Kent and Canterbury Hospital
Telephone: 01227 864137 (9am to 5pm)
EmailKent (Vascular) Ward, Kent and Canterbury Hospital
Telephone: 01227 783102