Diverticulosis and diverticulitis
Information for patients from the Department of Colorectal Surgery
You have been diagnosed with diverticular disease. This leaflet will:
explain the condition, and it's causes and symptoms
outline the treatment options, and
explain what will happen if you need surgery.
If you have any questions after reading this leaflet, please speak to your GP.
What is diverticular disease?
The colon (or large intestine) can develop small pouches. These pouches bulge outward through the colon’s muscular wall. They develop in areas where blood vessels are entering the muscular wall. This area is a weaker spot that allows these pouches to form.
Each pouch is called a diverticulum. Pouches are called diverticula. The condition of having diverticula is called diverticulosis.
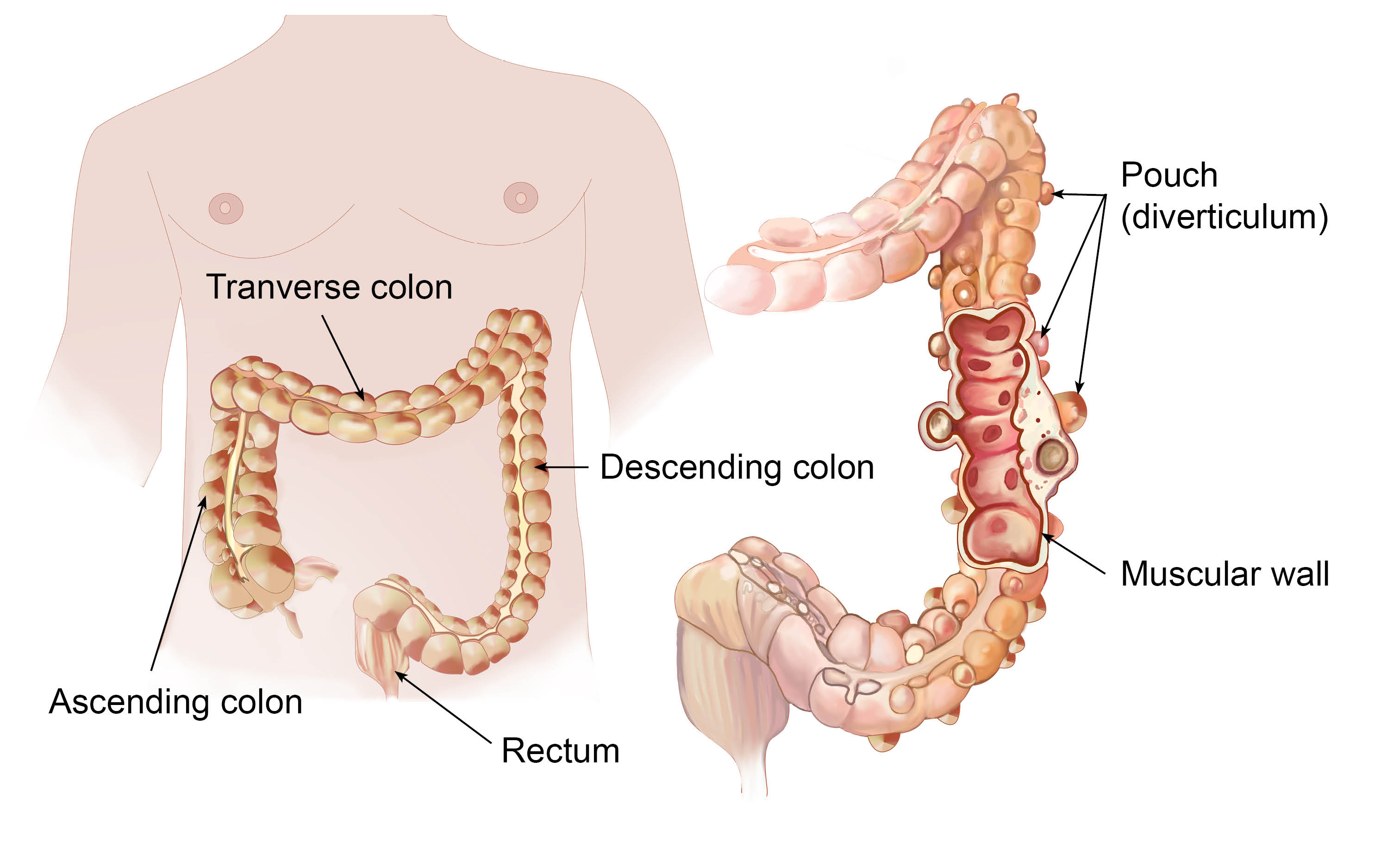
When the pouches become infected or inflamed, the condition is called diverticulitis. This occurs in 10 to 25 in every 100 people with diverticulosis. Diverticulosis and diverticulitis are also known as diverticular disease.
Diverticular disease is extremely common in the developed world. Between 30% and 50% of this population will be affected during their lifetime.
What causes diverticular disease?
If your stools become small and hard instead of soft and bulky, your colon has to squeeze hard to push the stool forward. These contractions create high pressure in the muscular wall of your colon. If this continues over the years, then these pouches develop at the weak areas in the wall of your colon. This is one of the reasons why diverticula are more likely to develop in the left side of the colon.
There is no exact cause of diverticular disease. However, the following could increase your risk of developing the disease:
increasing age
obesity / high BMI (body mass index), and
people on low fibre diets.
Fibre is the part of fruits, vegetables, and grains that the body cannot digest. Some fibre dissolves easily in water (soluble fibre). It takes on a soft, jelly-like texture in the intestines. Some fibre passes almost unchanged through the intestines (insoluble fibre). Both kinds of fibre help make stools soft and easy to pass. Fibre also prevents constipation.
What are the symptoms?
Diverticulosis
Most people with diverticulosis do not have any discomfort or symptoms. However, possible symptoms may include mild cramps, bloating, and constipation. These symptoms do not always mean you have diverticulosis. Other diseases such as irritable bowel syndrome (IBS) and stomach ulcers cause similar problems. You should visit your doctor if you have these symptoms.
Diverticulitis
The most common symptom of diverticulitis is abdominal pain. The most common sign is tenderness around the left side of the lower abdomen. If infection is the cause, you may have the following symptoms as well:
fever
nausea (feeling sick)
vomiting
chills
cramping, and
constipation.
How bad your symptoms are depends on the extent of the infection and complications.
What are the complications?
Diverticulitis can lead to bleeding, infections, perforations (small holes), tears, or blockages. These complications need treatment to stop them getting worse and causing serious illness.
Bleeding
Bleeding from diverticula is a rare complication. When diverticula bleed, you may find blood in the toilet or in your stool. Bleeding can be severe, but it may stop by itself and not need treatment. If you have bleeding from your rectum, you should see your doctor. You may need surgery if the bleeding does not stop.
Abscess, perforation, and peritonitis
The infection causing diverticulitis often clears up after taking antibiotics for a few days. If your condition gets worse, an abscess may have formed in your colon. An abscess is an infected area with pus, that may cause swelling and destroy tissue. Sometimes the infected diverticula may develop small holes called perforations. These perforations allow pus to leak out of the colon into your abdominal area. If the abscess is small and remains in your colon, it may clear up after treatment with antibiotics. If not, your doctor may need to drain it.
To drain the abscess, your doctor uses a needle and a small tube called a catheter. They insert the needle through your skin under a local anaesthetic (you will be awake but the area being treated is numb) and drains the fluid through the catheter. This procedure is called percutaneous catheter drainage. You may need surgery to clear the abscess and / or remove part of your colon.
A large abscess can become a serious problem, if the infection leaks out and contaminates areas outside your colon. Infections that spread into the abdominal cavity are called peritonitis. Peritonitis needs immediate surgery to clean the abdominal cavity and to remove the damaged part of your colon. Without surgery, peritonitis can be fatal.
Fistula
A fistula is an abnormal connection of tissue between two organs, or between an organ and the skin. When damaged tissues come into contact with one another during infection, they sometimes stick together. If they heal that way, a fistula forms. When diverticulitis related infections spread outside the colon, the colon tissue may stick to other nearby tissues. The organs usually involved are the bladder, small intestine, and skin.
The most common type of fistula happens between the bladder and the colon. It affects men more than women. This type of fistula can result in a severe, long-lasting infection of the urinary tract. Surgery to remove the fistula and the affected part of your colon can correct this problem.
Intestinal obstruction
The scarring caused by infection may cause part or total blockage of your colon. When this happens, your colon is unable to move bowel contents normally. When the obstruction totally blocks your colon, you will need emergency surgery. Partial blockage is not an emergency, so the surgery to correct it can be planned.
How does your doctor diagnose diverticular disease?
To diagnose diverticular disease, your doctor will:
Ask about your medical history. They may ask you about your bowel habits, symptoms, pain, diet, and medications.
Perform a physical examination, usually with a digital rectal examination. To perform this test, your doctor inserts a gloved, lubricated finger into your rectum. This allows them to check for any tenderness, blockages, or blood.
Your doctor may perform one or more tests. They may check your stools for signs of bleeding and test your blood for signs of infection.
As most people do not have symptoms. Diverticulosis is often found through tests ordered for another condition.
Your doctor will order further tests which may include the following.
A colonoscopy or flexible sigmoidoscopy. During a colonoscopy, a tube with a camera is passed into your colon through your back passage. This allows the endoscopist to see the inner lining of your whole colon. A sigmoidoscopy is a similar procedure that views mostly the left side of your colon. Medication can be given to make the procedure comfortable. You are given medication before your procedure to make sure your bowels are completely empty.
A CT colonoscopy is an x-ray-based test. You are given medication before your procedure to make sure your bowels are completely empty.
What is the treatment for diverticula disease?
A high-fibre diet and occasionally, mild painkillers will help relieve symptoms in most cases. Sometimes an attack of diverticulitis is serious enough to need a hospital stay and surgery.
Diverticulosis
Increasing the amount of fibre in your diet may reduce symptoms of diverticulosis. It may also prevent complications, such as diverticulitis. Fibre keeps stools soft and lowers pressure inside the colon. This allows bowel content to move through easily. You should eat / drink 20 to 35 grams of fibre daily. The table below shows the amount of fibre in some foods that you can add to your diet.
Your doctor may also recommend taking a fibre product such as Fybogel once a day. These products are mixed with water. They provide about 2 to 3.5 grams per tablespoon, mixed with 8 ounces of water. Fybogel and Psyllium seed products are available in pharmacies.
Until recently, many doctors suggested avoiding foods with small seeds. They believed that the seeds could lodge in the diverticula and cause inflammation. It is now generally accepted that only foods that may irritate or get caught in the diverticula cause problems. Avoid the following foods:
nuts
popcorn hulls,
and sunflower, pumpkin, caraway, and sesame seeds.
The seeds in tomatoes, courgettes, cucumbers, strawberries, and raspberries, as well as poppy seeds, are considered harmless. People differ in the amounts and types of foods they can eat. Make decisions about your diet on what works best for you. Keeping a diary may help identify individual items in your diet.
If cramps, bloating, and constipation are problems, your doctor may prescribe a short course of pain medication. However, many medications can cause constipation.
You should take regular exercise, lose weight if you are overweight or obese, and stop smoking. Studies do not show that these changes will definitely help all patients. But changes to a person’s lifestyle will bring benefits to general health and wellbeing.
Amount of fibre in some foods
| Breakfast cereals | Typical portion (weight) | Fibre / portion |
|---|---|---|
| All-Bran | 1 medium sized bowl (40g) | 9.8 grams |
| Shredded Wheat | 2 pieces (44g) | 4.3 grams |
| Bran Flakes | 1 medium sized bowl (30g) | 3.9 grams |
| Weetabix | 2 pieces (37.5g) | 3.6 grams |
| Museli (no added sugar) | 1 medium sized bowl (45g) | 3.4 grams |
| Muesli (Swiss style) | 1 medium sized bowl (45g) | 2.9 grams |
| Fruit 'n' Fibre | 1 medium sized bowl (40g) | 2.8 grams |
| Porridge (milk or water) | 1 medium sized bowl (250g) | 2.3 grams |
| Cornflakes | 1 medium sized bowl (30g) | 0.3 grams |
| Bread / rice / pasta | Typical portion (weight) | Fibre / portion |
|---|---|---|
| Crispbreads (rye) | 4 crispbreads (36g) | 4.2 grams |
| Pitta bread (wholemeal) | 1 piece (75g) | 3.9 grams |
| Pasta (plain, fresh cooked) | 1 medium portion (200g) | 3.8 grams |
| Wholemeal bread | 2 slices (70g) | 3.5 grams |
| Naan bread | 1 piece (160g) | 3.2 grams |
| Brown bread | 2 slices (70g) | 2.5 grams |
| Granary bread | 2 slices (70g) | 2.3 grams |
| Brown rice (boiled) | 1 medium portion (200g) | 1.6 grams |
| White bread | 2 slices (70g) | 1.3 grams |
| White rice (boiled) | 1 medium portion (200g) | 0.2 grams |
| Vegetable | Typical portion (weight) | Fibre / portion |
|---|---|---|
| Baked beans | Half a can (200g) | 7.4 grams |
| Red kidney beans | 3 tablespoons (80g) | 5.4 grams |
| Peas (boiled) | 3 heaped tablespoons (80g) | 3.6 grams |
| French beans (boiled) | 4 heaped tablespoons (80g) | 3.3 grams |
| Brussel sprouts (boiled) | 8 sprouts (80g) | 2.5 grams |
| Potatoes (old, boiled) | 1 medium size (200g) | 2.4 grams |
| Spring greens (boiled) | 4 heaped tablespoons (80g) | 2.1 grams |
| Carrots (boiled / sliced) | 3 heaped tablespoons (80g) | 2.0 grams |
| Broccoli (boiled) | 2 spears (80g) | 1.8 grams |
| Spinach (boiled) | 2 heaped tablespoons (80g) | 1.7 grams |
| Salad vegetables | Typical portion (weight) | Fibre / portion |
|---|---|---|
| Pepper (green or red) | Half (80g) | 1.3 grams |
| Onions (raw) | 1 medium (80g) | 1.1 grams |
| Olives (in brine) | 1 heaped tablespoon (30g) | 0.9 grams |
| Tomato (raw) | 1 medium / 7 cherry (80g) | 0.8 grams |
| Lettuce (sliced) | 1 bowl (80g) | 0.7 grams |
| Fruit | Typical portion (weight) | Fibre / portion |
|---|---|---|
| Avocado pear | 1 medium (145g) | 4.9 grams |
| Pear (with skin) | 1 medium (170g) | 3.7 grams |
| Orange | 1 medium (160g) | 2.7 grams |
| Apple (with skin) | 1 medium (112g) | 2.0 grams |
| Raspberries | 2 handfuls (80g) | 2.0 grams |
| Banana | 1 medium (150g) | 1.7 grams |
| Tomato juice | 1 small glass (200ml) | 1.2 grams |
| Strawberries | 7 strawberries (80g) | 0.9 grams |
| Grapes | 1 handful (80g) | 0.6 grams |
| Orange juice | 1 small glass (200ml) | 0.2 grams |
| Dried fruit / nuts | Typical portion (weight) | Fibre / portion |
|---|---|---|
| Apricots (semi-dried) | 3 whole (80g) | 5.0 grams |
| Prunes (semi-dried) | 3 whole (80g) | 4.6 grams |
| Almonds | 20 nuts (33g) | 2.4 grams |
| Peanuts (plain) | 1 tablespoon (25g) | 1.6 grams |
| Mixed nuts | 1 tablespoon (25g) | 1.5 grams |
| Brazil nuts | 10 nuts (33g) | 1.4 grams |
| Raisins / sultanas | 1 tablespoon (25g) | 0.5 grams |
| Other foods | Typical portion (weight) | Fibre / portion |
|---|---|---|
| Quorn (pieces) | 1 serving (100g) | 4.8 grams |
| Chicken curry (takeaway) | 1 portion meat / sauce (150g) | 3.0 grams |
| Vegetable pasty | 1 medium sized (150g) | 3.0 grams |
| Bran (wheat) | 1 tablespoon (7g) | 2.5 grams |
| Potato crisps (low fat) | 1 bag (35g) | 2.1 grams |
| Pakora / bhajia (vegetable) | 1 portion (50g) | 1.8 grams |
| Pizza (cheese and tomato) | 1 slice, deep pan (80g) | 1.8 grams |
Diverticulitis
Treatment for diverticulitis focuses on:
clearing up the infection and inflammation
resting your colon, and
preventing or minimising complications.
If treated early, an attack of diverticulitis without complications may respond to antibiotics within a few days.
To help your colon rest, your doctor may recommend bed rest and a liquid diet, along with pain relief.
When is surgery necessary?
Your doctor may advise surgery, if:
your attacks are severe or happen often, or
you develop a fistula or intestinal obstruction.
This involves your surgeon removing the affected part of your colon and joining the remaining sections. This is called colon resection. It aims to keep attacks from coming back and prevents complications.
If antibiotics do not correct an attack, you may need emergency surgery. Reasons for emergency surgery include:
a large abscess
perforation
peritonitis, or
continued bleeding.
Emergency surgery usually involves two operations. The first surgery will clear the infected abdominal cavity and remove part of your colon. Infection and sometimes obstruction, make it unsafe to re-join your colon during the first operation. Instead, your surgeon creates a temporary hole, or stoma, in your abdomen. They connect the end of your colon to the hole, with a procedure called colostomy. This will allow you to eat normally and have normal bowel movements. The stool goes into a bag attached to the opening in your abdomen. In the second operation, your surgeon re-joins the ends of your colon.
Further information
The British Dietetic Association (BDA) has information on healthy eating on their website.
If you have any questions or concerns, please speak to the healthcare professional responsible for your care.