Diagnosis and treatment of venous thrombo-embolism (VTE) in pregnancy and after birth
Information for women, birthing people, and their families
This leaflet is for you, if your doctor suspects you may have a blood clot in your leg or your lungs. It explains the investigations, and treatment for blood clots whilst you are pregnant, or have recently given birth. This condition is known as venous thrombo-embolism or VTE.
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are both known as a venous thrombo-embolism (VTE)
What is a deep vein thrombosis (DVT)?
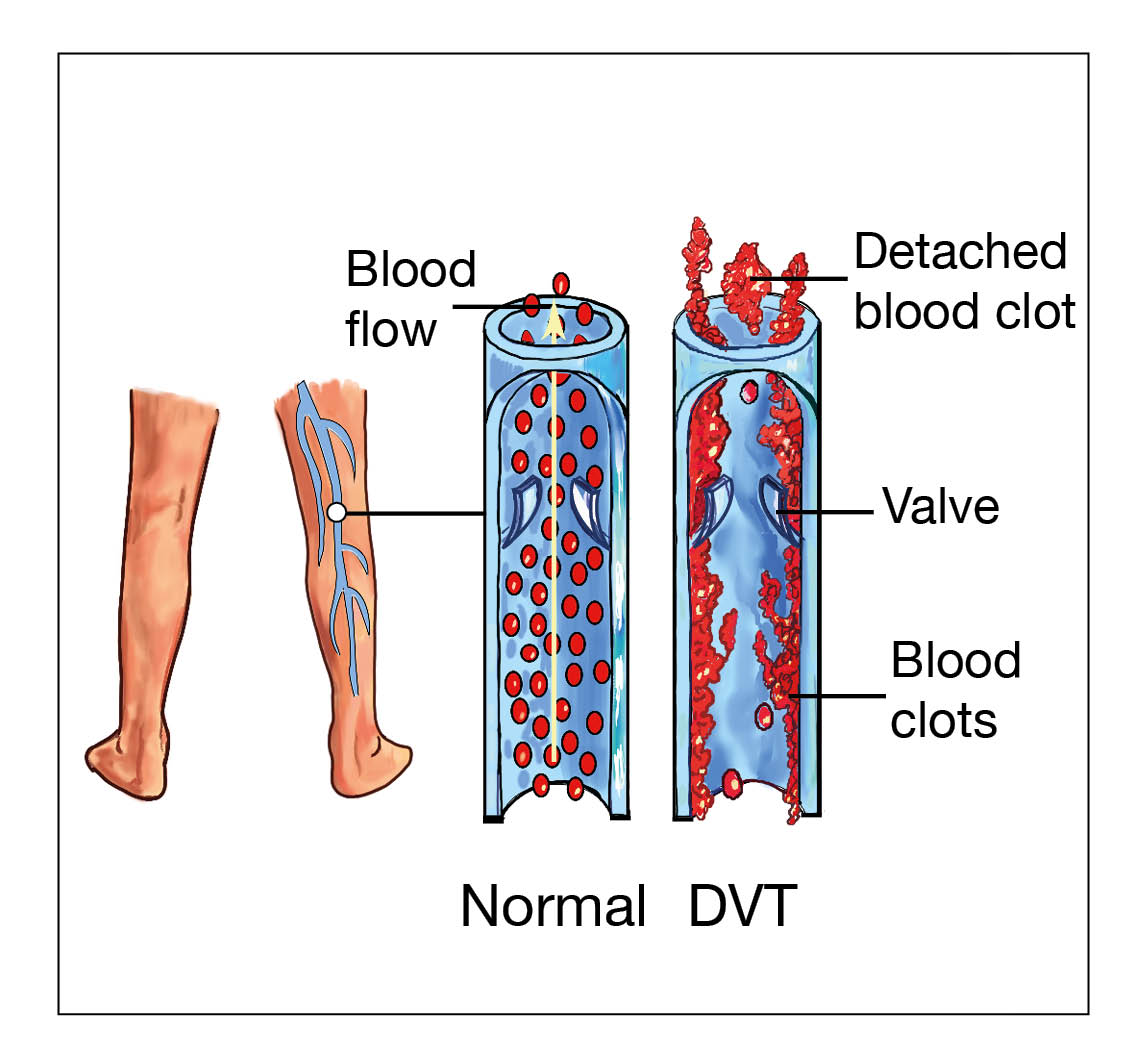
A DVT is a blood clot in a deep vein. Deep veins are large blood vessels which return blood to the heart. These veins lie deep within the body and cannot be seen. A DVT usually involves the deep veins of the legs, thigh, or pelvis, but can occur elsewhere in the body. Calf veins (found in the back part of your lower leg, between your knee and ankle) are the most common site for a DVT.
Symptoms can vary according to the size and location of the clot. They may include:
Swelling of your limb / leg (this can be sudden).
Pain or tenderness in your limb / leg, often in the calf. This can increase when standing or walking.
Change in skin colour. For example red or purple of light skin tones, and darker brown on darker skin tones.
Unexplained feeling of warmth in your limb / leg.
Swollen veins that are hard or sore to touch.
How is a DVT diagnosed?
Doppler ultrasound scan. This uses an ultrasound machine to look for the clot in the veins.
Other scans. Sometimes a blood clot can form higher up in the veins in your tummy (that lead to the leg veins). In that situation, we will need other scans, such as MRI (magnetic resonance imaging). This is safe to carry out in pregnancy, if needed, and is only rarely required.
What are the risks of not identifying a DVT?
A DVT can also cause long-term swelling and discoloured legs. They call it post thrombotic syndrome. Part of the clot could break off and travel to your lungs. This is a pulmonary embolism (PE).
What is a pulmonary embolism (PE)
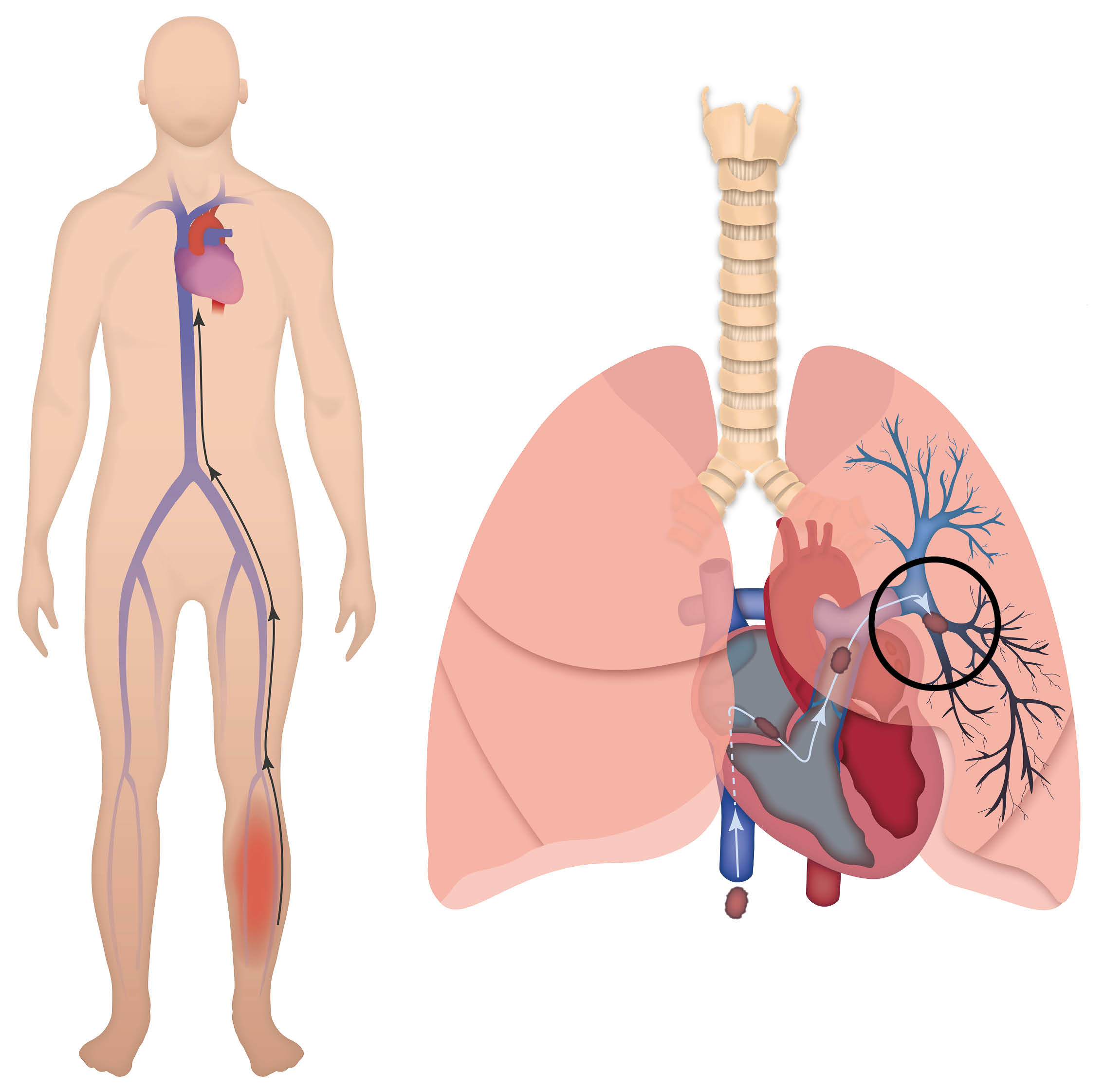
A pulmonary embolism (PE) is a blood clot, which is lodged in one or more of the arteries in the lung. A PE usually originates from a DVT. A PE can be life-threatening if left untreated.
Symptoms can include some or all of the following:
Shortness of breath, either at rest or on exertion (this may be sudden and unexplained). This is due to the blood clot restricting the blood flow through the lungs. In some cases, oxygen may be needed to help with this.
An increased heart rate. This is due to the heart having to work harder to make sure enough oxygen is transported around the body.
Tightness in your chest or chest pain. This may be constant or only when breathing deeply. This is due to inflammation in the lungs or lining of the lungs.
Coughing. Occasionally, coughing-up blood or blood-stained sputum.
Feeling very unwell or collapsing.
May also be accompanied by symptoms of a DVT.
How is a PE diagnosed?
If you have symptoms of a PE, we will advise and arrange for you to have an electrocardiogram (ECG) and a chest X-ray.
If you have symptoms of DVT (see What is a DVT? above), we will usually carry out an ultrasound scan (Doppler) of your legs. You will not need any further scans if the Doppler confirms a DVT. Treating your DVT will also treat any PE you may have, as the treatment for both conditions is the same.
There are two types of scans used to diagnose a PE. These are a ventilation / perfusion (VQ) scan or computerised tomography pulmonary angiography (CTPA). Before you have either of these, you will need a chest X-ray.
Chest X-ray
The X-ray uses a tiny dose of radiation to create an image of your chest and lungs. This rules out other conditions, such as pneumonia, which can cause very similar symptoms to a PE. In that case, you may not need the V/Q scan or CTPA, so it is an important test to do first.
The tiny dose of radiation used in a chest X-ray is not considered at all harmful for you or your baby.
Ventilation / perfusion (V/Q) scan
During this scan you will have a small narrow tube, called a cannula, put into a vein in your arm. The scan has two stages:
First part: Breathing in a low dose of a radioactive substance through a small plastic mask.
Second part: An injection of a low dose of a radioactive substance through the cannula in your arm.
A special camera picks up radiation from both and then creates images of the blood supply to your lungs. Sometimes only the second half is done. The scan would then be described as a Q scan (perfusion only).
In pregnancy, the second part can use half the normal radiation dose. Research shows it is as good at diagnosing PEs as using the full dose. This is called a 'half-dose' scan.
Computerised Tomography Pulmonary Angiography (CTPA)
This is a specialised scan of your lungs by a scanner that uses X-rays to create images. You will have an injection of dye into a cannula (a small narrow tube) in a vein in your arm. The dye makes the blood vessels of your lungs easy to see on the scan images, so that clots can be seen.
Dye used in CTPA is different to a VQ scan and is not radioactive. The radiation comes from the X-ray machine used to take the pictures.
What are the risks to me and my baby from having a V/Q scan or a CTPA?
V/Q scans and CTPA scans both involve 'ionising radiation'. lonising radiation can sometimes cause cell damage which, could turn cancerous.
Risks to you. A CT scan gives a higher dose of radiation to your breasts than a VQ scan and the lifetime risk of breast cancer may be increased. Some studies suggest increase by 13.6% above your background risk.
Risks to your baby. Your baby will be exposed to lower levels of radiation than you will. The level of radiation during a V/Q scan is a little higher than your baby would receive from a CTPA scan. But it is still so low that the risk to your baby is considered to be minimal.
Risk from a V/Q scan is approximately 1 case of childhood cancer from 280,000 scans. Risk from a CTPA scan is approximately 1 case of childhood cancer from one million scans.
Do I need to take any other precautions for these tests?
VQ scan
No special preparation is needed before the test. You can eat, drink, and take medication as normal. The radioactive dye will still be in your body for a few hours after the scan. During this time, you might give off a small amount of radiation. It may also be in your body fluids, such as your urine. Because of this:
Pregnant staff members should not care for you in the first 12 hours after your test.
Avoid long periods of close contact with your baby. Do not cuddle your baby for longer than 30 minutes. You should follow this advice for the first 12 hours after your scan.
You should not breastfeed your baby for 12 hours following your scan. You should express any breastmilk you produce during this time and discard it. If you are able to, express at least one feed before your scan and store it to give to your baby after your scan.
Use the toilet, rather than a bedpan or bottle, and flush the toilet twice, in the first 12 hours after the scan.
Family members, including children, can visit you as normal.
CTPA
You do not need to take any extra precautions before or after a CTPA.
When is a V/Q scan not appropriate?
Doctors will not recommend a VQ scan:
if you have a chest condition (such as asthma)
if you smoke, as this can affect the results, or
you have had a chest X-ray that shows an abnormality.
The V/Q scan cannot be carried out in an emergency. If a scan is needed to make a diagnosis in an emergency, a CTPA would be advised.
Why do I need to have either a V/Q or CTPA scan?
If a PE is left untreated, there is a risk of death. There are also longer-term consequences, including heart failure. This occurs when excessive strain is put on your heart. There are no good alternatives to using these scans. Doctors cannot confirm the diagnosis during pregnancy with blood tests or examinations alone.
A diagnosis of DVT or PE has important implications for future pregnancies. You may need to inject yourself daily with preventative injections. Your midwife or doctor will discuss this with you further if you have any questions or worries.
You should avoid the combined oral contraceptive pill and hormone replacement therapy. These can increase the chance of a blood clot happening again.
Why can I not just have the treatment without having a scan?
The blood-thinning injections can cause an increased risk of bleeding. It is not a treatment that could be given for any length of time as ‘just in case’ with treatment doses.
It is also important to exclude any other medical condition that may have similar symptoms to PE / DVT. Blood-thinning injections might not treat those conditions.
Overall, it is a risk-benefit ratio / balance. The risks associated with scans are lower than the risks of continuing treatment without a confirmed diagnosis.
If I can have a V/Q scan whilst I’m pregnant, why are pregnant staff members not allowed to care for me after my scan?
The radiation dose to you from a single scan is very small. The risk to a pregnant member of staff caring for you is even smaller. The reason we protect pregnant staff is because they may come into contact with your bodily fluids. Also, while you are only getting one radiation dose our midwives see many women whilst they are working and the risk grows with the number of women seen.
What happens when the diagnosis is confirmed?
You will be started on the treatment doses of blood-thinning injections.
You will be referred to a specialist antenatal clinic. You will have the chance to ask questions and discuss your treatment options. Together a management plan will be made for the rest of your pregnancy, your delivery, and after birth.
You will also be referred to the Thrombosis Clinic at Kent and Canterbury Hospital. You will be seen by a specialist who will review and provide a treatment plan, which will include treatment length. If you do not receive an appointment for this, please contact you midwife.
How will the DVT / PE be treated?
The treatment of the blood clot involves having blood-thinning injections of enoxaparin. Enoxaparin is a low molecular weight heparin (LMWH). Your treatment may start before your scans are performed or before confirming diagnosis. The dose and duration of treatment will depend on your weight and clinical diagnosis.
In case of a DVT, you may also be prescribed a special stocking to wear on your affected leg. This helps to maintain blood flow in the veins in your leg, which in turn helps to reduce any pain and swelling.
What does enoxaparin treatment involve?
Enoxaparin is given as an injection under the skin (subcutaneous) at the same time every day. Dosage depends on your weight and on your individual risks.
You (or a family member) will be shown how and where on your body to give the injections. See Injecting yourself with enoxaparin below. We understand that you may be worried about this. If you are worried or frightened about this, please talk to your midwife or healthcare professional.
Clinicians will provide you with the needles and syringes (already made-up) and a sharps bin. You will be given advice on how to store and dispose of these.
Some blood-thinning treatments contain animal products. Enoxaparin has content that has been derived from pigs. If you are concerned about this, please speak to your midwife or your healthcare professional.
Will being on enoxaparin affect how I give birth?
No. Taking enoxaparin during pregnancy should not affect how you deliver your baby.
Are there any risks to my baby and me from enoxaparin?
Enoxaparin, is a low-molecular-weight heparin. It does not cross the placenta, so it cannot harm your baby.
There may be some bruising where you inject, but this will usually fade in a few days.
The medicine may sting a little when you inject it, but this only lasts a few seconds.
One or two patients in every 100 (1 to 2%) will have an allergic reaction. If you notice a rash after injecting, you should tell your doctor so that they can change the type of medicine.
You should also contact us if you have any bleeding. Phone our telephone Maternity Triage service if you have any concerns. Their number is in your lilac notes and at the bottom of this leaflet.
How long will I need to take enoxaparin for?
Treatment is usually recommended for the rest of your pregnancy and for at least six weeks after the birth. The minimum treatment time is three months and you may need to continue it for longer.
What should I do when labour starts while I am taking enoxaparin?
If you think you are going into labour, please do not take any more injections. Phone Maternity Triage and tell them that you are on enoxaparin treatment for a VTE. They will tell you what to do. Their telephone number is on the front of your lilac notes and at the bottom of this leaflet.
Can I have an epidural whilst taking enoxaparin?
There is a 24 hour ‘window’ between when you take your last dose of enoxaparin, and when an epidural can be given. You will be offered alternative pain relief if you are within this time frame. Your midwife will discuss these options with you. If the plan is to induce labour, you should stop your injections 24 hours before your planned date.
What happens if I have a caesarean birth?
For a planned caesarean birth. Your last enoxaparin injection should be 24 hours before the delivery.
For an emergency caesarean birth. If your last enoxaparin injection was within 24 hours, you will not be able to have an epidural or spinal injection. Instead, you will need a general anaesthetic for your operation. The anaesthetist will discuss this with you. Your blood thinning medication will be restarted within four hours of your operation.
What happens after birth?
Treatment should be continued for at least six weeks after birth. You are likely to need treatment for longer if your DVT or PE was diagnosed late in your pregnancy or after birth. There is a choice of treatment after birth. Your doctor will discuss your options with you.
At your postnatal appointment the doctor will:
Ask about your family history of blood clots. Discuss tests for a condition that makes thrombosis more likely (thrombophilia). These tests should be done after you have stopped treatment. Ideally, they should be done before any future pregnancies.
Discuss your options for contraception. You will be advised not to take any oestrogen containing contraception.
Discuss future pregnancies. Enoxaparin treatment will be recommended during and after your next pregnancy.
Can I breastfeed?
Yes. Both enoxaparin and warfarin are safe to take when breastfeeding. Oral anticoagulants, such as apixaban and rivaroxaban, are not recommended in pregnancy or breastfeeding.
Enoxaparin
Before injecting yourself with enoxaparin
Check the expiry date. Do not use if date has passed.
Check the syringe is not damaged and the liquid inside is clear.
An air bubble in the syringe is normal. Do not press the plunger to remove it.
Injecting yourself with enoxaparin
Wash your hands with soap and water.
Pull off the grey needle cap. Do not bend the needle. Do not let the needle touch anything (this keeps it clean).
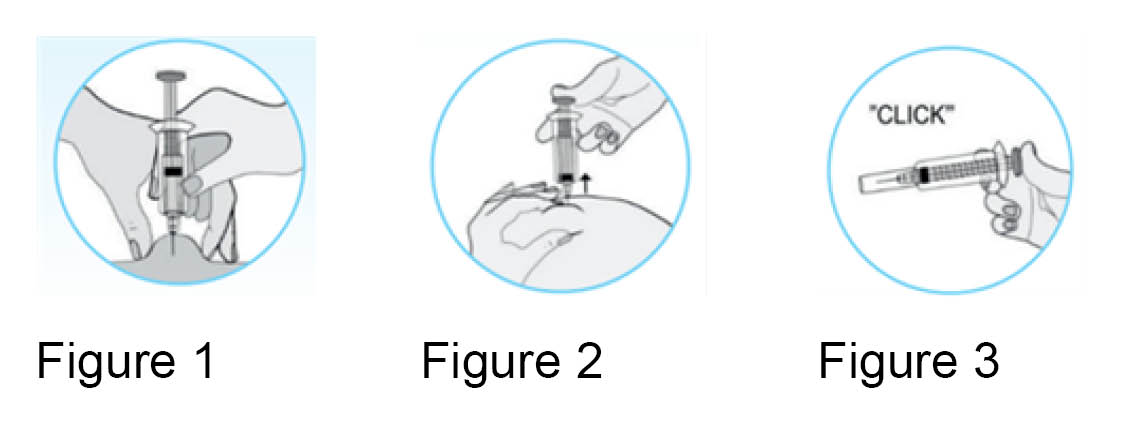
Hold the syringe in your dominant hand (the hand you write with). Pinch your skin with your other hand. Choose an area about 5cm away from your belly button (and no higher) and away from any scars. Alternate the side you inject each time. See Figure 1.
Insert the full length of needle straight (at angle of 90 degrees) into the area of skin.
Make sure to keep the skin pinched throughout the injection (see Figure 2).
Press down firmly on the plunger. Injecting the medication slowly until the syringe is empty.
Keep the plunger pressed down and carefully remove the needle. When the needle is out you can let go of the area of skin. Do not rub the skin afterwards, this causes bruising.
Push down on the plunger until it clicks. This releases the protective needle cover (see Figure 3).
Place the needle and syringe into the sharps bin. Keep this out of the reach of children.
When the sharps bin is full, you will need to go online to arrange collection. You can arrange collection through the Kent County Council web site. Scroll down to 'Clinical waste collection', and select your local council. Do not put the syringe in your household rubbish.
The preferred site for injection is your tummy. However, if you feel uncomfortable injecting your tummy you can inject into your thigh. Remember to alternate your injection site each time.
What should I do for future pregnancies?
If you have had a confirmed VTE, get advice from your doctor before becoming pregnant. If you become pregnant first, see your doctor as soon as possible. It is important to make a plan to reduce your risk of having another VTE.
Who can I contact if I have concerns?
For help and advice, contact our Maternity telephone triage service on 01227 206737.
Further information
You can find further information on how to reduce your risk of a DVT and PE in hospital at Thrombosis UK.
Download the Thrombosis UK app, ‘Let's talk clots’ from the App Store or Google Play. They have an extensive section on VTE in pregnancy and after childbirth.
This link takes you to a video showing you how to inject enoxaparin yourself.
References

Royal College of Obstetricians and Gynaecologists (RCOG). Diagnosis and treatment of venous thrombosis in pregnancy and after birth. August 2015.
NICE. Venous thromboembolic diseases: diagnosis, management and thrombophilia testing. NICE guidelines. NICE guidelines (NG158). Last updated 02 August 2023.
Community Pharmacy Hampshire & Isle of Wight. How to inject with Inhixa (enoxaparin). July 2019.