Dental advice for patients having radiotherapy and chemotherapy for head and neck cancer
Information for patients from the Oral and Maxillofacial Department
The management of your head and neck cancer can involve:
an operation, and / or
radiotherapy / chemotherapy.
The aim of these treatments is to cure or shrink your cancer. Unfortunately, the side effects of these treatments can have long-term effects on your face and mouth. This leaflet will explain what side effects you may have in the short- and long-term.
If you have any questions, please contact us Monday to Friday 8am to 5pm:
Restorative Dentistry reception desk
Telephone: 01233 616045Restorative Dentistry Secretary
Telephone: 01227 866317
Why have I been referred to the Restorative Dental team?
Before you start your cancer treatment, you must have a dental assessment at the hospital. The assessment will be with a consultant in restorative dentistry or a member of their team. This is because the treatment you are going to have causes:
soreness and dryness of the mouth due to reduced saliva, and
an increased risk of tooth decay, gum disease, and infections.
It is very important that your mouth is as healthy as possible before you start chemotherapy / radiotherapy.
We may also need to arrange for you to have:
some teeth removed before your cancer treatment, and / or
some fillings for you either before or after your cancer treatment, depending on how urgent it is.
When will I have my dental assessment?
Sometimes you will have your dental assessment after your chemotherapy has begun. This will prevent any delays with your cancer treatment.
The Dental team will arrange your dental assessment around your chemotherapy schedule. This will allow you time to recover before any dental work begins.
What will happen at my dental assessment appointment?
The team will take a large x-ray of your upper and lower jaws, to check your teeth and bones. Your oncologist will ask for this before you come to your dental assessment appointment. They will want to make sure that we have all the information we need before we see you.
Before your chemotherapy / radiotherapy, you will have a dental assessment with a consultant in restorative dentistry or a member of their team.
As part of this dental assessment, your consultant may recommend the removal (extraction) of some of your teeth. This may be because your teeth:
have infections
are badly broken down
may cause problems in the future, as they are next to the radiotherapy fields, or
your teeth are near the cancer.
Extraction may also help your surgeons to remove the tumour.
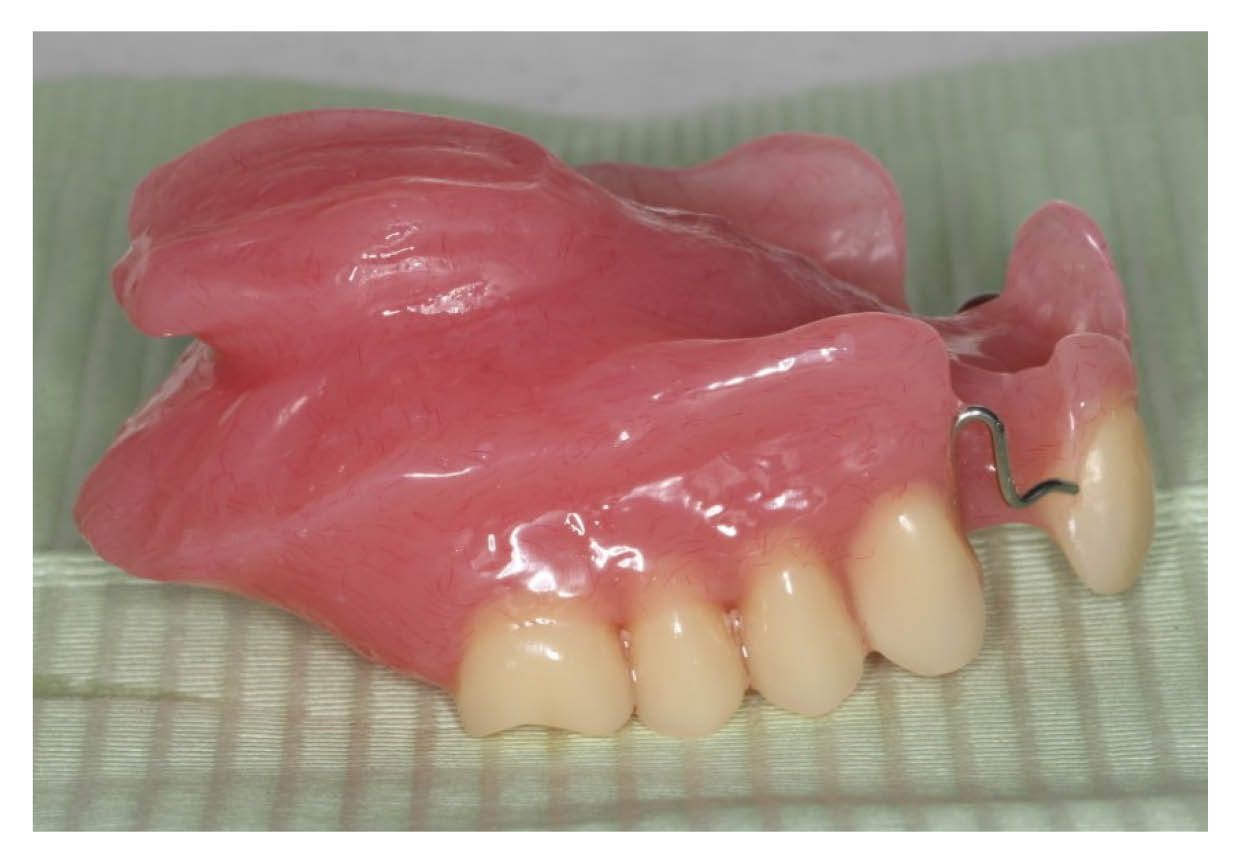
We may provide you with immediate replacement dentures, but this will depend on which teeth are removed.
If your cancer surgery involves your upper jaw, you may have an ‘obturator’ made. The obturator closes any opening between the roof of your mouth and your nasal cavity. The obturator will stay in place after your operation and during your radiotherapy treatment. It is replaced with a new prosthesis after the area has healed. More details on how an obturator can help you can be found in the next section.
Radiotherapy treatment causes damage to the blood supply of the upper and lower jaw bones. If you need to have a tooth removed after radiotherapy, you risk having a serious bone infection of the jaw called osteoradionecrosis. Osteoradionecrosis is a condition where the bone dies and becomes infected. To try and stop this, at your assessment we will check if you have any teeth that are at risk of being lost in the future. If you do, we will arrange to have these teeth extracted before your cancer treatment begins. This will avoid the risk of you developing this bone infection later in life.
The Oral Surgery team will carry out any dental extractions for you as soon as possible. We may also need to do some fillings for you, either before or after your cancer treatment depending on how urgent it is. Your consultant will discuss this with you at your assessment.
What is an obturator?
If your surgery results in a hole being created in your palate (roof of your mouth), an obturator plate may be used.
An obturator is a removable prosthesis (artificial device). It closes the hole in your palate left by your cancer operation. If the hole in your palate is left open, it:
will affect your speech, and
can cause food to escape from your mouth up into your nose while you eat and drink.
The obturator will improve your speech, air flow, and how you eat. It will also reduce the chances of you regurgitating your food. Regurgitating is bringing your food back up into your mouth.
The team will regularly review your obturator. It will need to be remade every so often, due to changes in the shape of your mouth after your cancer operation.
If you need to have an obturator fitted, your doctor will discuss this with you in more detail.
How can I protect my teeth during my chemotherapy / radiotherapy treatment?
We will prescribe you high concentration fluoridated toothpaste called Duraphat 5000ppm. Use this toothpaste twice a day. You must get repeat prescriptions for this toothpaste from your GP or local dentist (free of charge) for the rest of your life. This toothpaste protects your teeth from tooth decay.
We understand that you may not be able to use this toothpaste during your chemotherapy / radiotherapy treatment, due to a burning feeling in your mouth. Please start using the toothpaste as soon as you are able to after your chemotherapy / radiotherapy has finished.
Use this toothpaste instead of any other toothpaste. You are more likely to get tooth decay now and this toothpaste can protect your teeth.
We also recommend that you use a pea-sized amount of GC Tooth Mousse. You smear this over your teeth with your finger; leaving it without rinsing for 5 minutes. After rinsing, brush your teeth for 2 minutes with Duraphat toothpaste. Spit the toothpaste out; do not rinse with water afterwards as this will wash away the toothpaste.
This mousse is very important, as it tops up the minerals in your saliva that are lost as a result of radiotherapy. You can buy the mousse from our department or online. Please speak to a member of staff for details.
We may also recommend you use an alcohol-free fluoride mouthwash, to help protect your teeth from tooth decay. Use this mouthwash once a day, 60 minutes after brushing your teeth with Duraphat toothpaste.
-
 Duraphat 5000ppm
Duraphat 5000ppm -
 GC Tooth Mousse
GC Tooth Mousse -
 Alcohol-free fluoride mouthwash
Alcohol-free fluoride mouthwash
It is very important to have good oral hygiene during your cancer treatment. We recommend you visit our Dental Hygiene Therapist to discuss how you brush your teeth.
What side effects can I expect during my radiotherapy / chemotherapy?
Expect some or all the following side effects during your radiotherapy / chemotherapy treatment.
Your mouth can become red, sore, and painful. This usually starts in the first 2 to 4 weeks, and settles 2 to 3 weeks after you complete your radiotherapy treatment.
During this time, it may become very difficult for you to swallow.
You may develop regular mouth ulcers and a burning feeling in your mouth.
If you have any pain or soreness in your mouth during your treatment, please speak with your clinical nurse specialist or Oncology team.
During your cancer treatment, you may not be able to brush your teeth due to the discomfort and pain. Do not worry if this is the case.
How can I manage the side effects?

Some mouthwashes may help with the soreness and ulcers in your mouth during radiotherapy / chemotherapy. These include Benzydamide (Difflam) mouthwash. Your Oncology team can prescribe this for you.
If you are unable to brush your teeth, you can use Chlorhexidine mouthwash as a disinfectant. Use this for 1 to 2 minutes, up to 2 to 4 times a day. Be aware that this may stain your teeth. Please stop using Chlorhexidine mouthwash once you can brush your teeth again, as it is no longer needed.
You can also use soft pink sponges to gently clean the inside of your mouth. But only do this while you are unable to brush your teeth during radiotherapy / chemotherapy.
Sucking on ice chips can help with mouth soreness and burning sensations in your mouth during treatment.
Do not drink alcohol or smoke. These can make your mouth feel worse.
Saliva substitutes can help lubricate your mouth. For more details, please speak to your pharmacist or a member of staff.
Lidocaine gel (local anaesthetic gel) can also provide short-term pain relief. For more details, please speak to your pharmacist or a member of staff.
I am having difficulty eating solid food, what can I do?
The soreness in your mouth can make eating very difficult. Whilst having radiotherapy, it is important that you keep up your strength. Eat plenty of carbohydrate foods to support you through your cancer treatment. Carbohydrate foods include pasta, potato, and rice-based dishes.
Your Oncology team and dietician may recommend you have a PEG tube to help you feed while your mouth is very uncomfortable. A PEG tube is a flexible feeding tube placed through your abdominal wall and into your stomach.
Or, they may advise you to have high energy drinks. These drinks are very important to keep your energy up during your cancer treatment. However, they are very high in sugar and can cause rapid dental decay of your teeth, causing them to break down. After drinking them rinse your mouth with water, as the sugar can cause damage to your teeth. You must make sure you have strength. Once you feel better and are able to eat and drink better, stop drinking high energy drinks and return to a balanced diet.
If possible, eat frequent soft meals.
Do not eat hot and spicy foods.
Do not eat acidic fruits, such as oranges, grapefruit, lemons, and pineapple.
Drink plenty of sugar-free fluids. Do not drink fruit juices.
What side effects may I have after my surgery and / or chemotherapy / radiotherapy?
Change in my appearance
If you had an operation to remove your cancer, and depending on the size of your cancer and where it is, you may have:
scarring on your face
a loss of facial symmetry after your cancer is removed, and
deviation of your jaw towards one side.
These issues vary from patient to patient.
Loss of taste
This is usually temporary, as the radiation treatment damages your taste buds. Most patients report the loss of taste with certain food groups such as spicy foods, salt flavours, and sweets.
Problems opening your mouth fully
Radiotherapy causes damage to the muscles around your cheeks. This causes them to scar and lose their elasticity. This is a common side effect of radiotherapy. It can make brushing your teeth, eating certain foods, and opening your mouth very difficult.
To help manage this, do not bite into hard foods.
After your radiotherapy, we will give you wooden spatulas to place between your teeth. These spatulas are used to do some daily jaw exercises. This will limit the extent of the problem and relieve some of the tightness in your jaw. Unfortunately it cannot reverse the effects of the reduced opening.
-
 Example of how wide you may be able to open your mouth before treatment
Example of how wide you may be able to open your mouth before treatment -
 Example of how wide you may be able to open your mouth after treatment
Example of how wide you may be able to open your mouth after treatment -
 Exercise your jaw by placing wooden spatulas between your teeth
Exercise your jaw by placing wooden spatulas between your teeth
Dry mouth
Saliva is important in clearing away food from your mouth. It also neutralises the acids from the food you eat.
Your salivary glands can get damaged from radiotherapy treatment. Most patients report that their mouth feels like sand, which makes it difficult to swallow or enjoy the taste of food. The dryness may improve after several months. However, it may never fully recover to the level you had before your cancer treatment.
When your saliva reduces, you become more likely to develop:
tooth decay
gum disease, and
infections in your mouth.
How to manage dry mouth
Carry a water bottle with you at all times. Take frequent sips of water throughout the day and night.
Use Vaseline on your lips frequently.
Suck on ice chips during your radiotherapy / chemotherapy treatment.
We can prescribe you products that act as saliva substitutes, to help moisten your mouth. If you have any teeth, please make sure this saliva substitute has a neutral pH, such as Saliva Orthana. You will only be prescribed alternative products, such as Glandosane, if you have no remaining teeth.

Caphosol® mouthwash can be used to help with dry mouth. It contains calcium and phosphate to replenish what is lost in your saliva.
Difficulty with dentures
Wearing your dentures can be very difficult during your radiotherapy treatment. This is due to your lack of saliva, which causes your dentures to not fit as well as before. It is also due to the inflammation (swelling) in your mouth, which can make wearing your dentures sore.
Advice to help with your dentures
Take them out at night or if they are causing ulcers or discomfort for you during the day.
If your dentures are loose, consider using a denture fixative.
Clean your dentures carefully after every meal.
To avoid infections, use a denture cleansing agent once a week.
If possible take your obturator out at night. Be aware, this will make it difficult to put your obturator back into your mouth first thing in the morning.
Sensitivity
Your mouth can become very sensitive to different food groups during radiotherapy / chemotherapy. These food groups include sweets, or cold or spicy foods.
Your mouth will also be very sensitive to toothpaste. Brushing your teeth may feel very uncomfortable. It is important to keep your mouth as clean as possible, but do not worry if you are unable to brush your teeth during this time.
How to manage sensitivity
During your radiotherapy, use Chlorhexidine mouthwash and some sponge brushes to gently wipe the inside surfaces of your mouth and all your teeth. If you find the mouthwash stings your gums, dilute it with water.
Be aware that the continued use of this mouthwash will stain your teeth.
If toothpaste irritates your mouth, brush with a solution of 1 teaspoon of salt added to 1 cup of warm water. Do this until you are able to start using toothpaste again.
Start using GC Tooth Mousse and high concentration fluoride toothpaste prescribed to you:
after you complete your radiotherapy / chemotherapy, and
your mouth is no longer sore.
You may also wish to use sensitive toothpaste.
How should I look after my mouth after my radiotherapy / chemotherapy is finished?

Do not smoke and drink alcohol. Smoking increases your risk of developing gum disease and causes tooth loss.
Good oral hygiene will prevent tooth decay and gum disease. Brush your teeth twice a day. Use a medium tufted toothbrush with a small / medium sized head, that can get to all the surfaces of your teeth and gums. A single tufted brush can also help to access your teeth for brushing.
Brush your teeth 30 to 60 minutes after each meal, snack, and sugary drink. Do not rinse your mouth after brushing, just spit out the remaining toothpaste.
If you have active or previous gum disease, we will show you how to use different sized interdental brushes. It is very important that you use these brushes twice a day every day. They will help you:
maintain good oral health, and
minimise the risk of your gum disease progressing, and needing any teeth taken out in the future.
Use high concentration fluoride toothpaste twice a day.
We will prescribe you with Duraphat 5000ppm toothpaste to begin with. You must see your GP or local dentist to get this toothpaste on repeat prescription for the rest of your life. Your teeth are at a greater risk of dental decay following radiotherapy. This toothpaste will help to protect you against tooth decay.
Please make sure no one else at home uses this toothpaste. It can be harmful if not prescribed specifically for you to use.
Use GC Tooth Mousse first, smeared over your teeth and left in place for 5 minutes. After 5 minutes, brush your teeth with the Duraphat 5000ppm toothpaste.
Visit your local dentist every 3 months to make sure your mouth is healthy. You will have a dental review appointment at the hospital 4 months after you complete your radiotherapy.
We will provide any difficult dental treatment you may need. However, we need you to see your local dentist every 3 to 6 months to carry out routine check-ups and dental treatment. You are at high risk of developing dental disease after radiotherapy. Please make sure that you are registered with a local dentist and that you see them regularly. Tooth decay can progress very quickly after you have had cancer treatment.
Do not have high sugar snacks and drinks between your meals. Follow the advice of your Oncology team and dietician. Fruit juices and fruits have sugar that can cause tooth decay and acid erosion to your teeth. Try to have sugary foods and drinks at meal times only.
Will I have a follow-up appointment with the Restorative Dental team?
Yes. After you complete your radiotherapy / chemotherapy, the team will review you again. We will help to rehabilitate your mouth as best as possible, and tell your GP and dentist about the treatment you have had.
Summary of products to help your mouth during and after chemotherapy / radiotherapy
GC Tooth Mousse replenishes the calcium phosphate ions lost in your saliva after radiotherapy. Smear the mousse on all your teeth for 5 minutes, then brush your teeth with Duraphat 5000ppm toothpaste. This mousse can only be bought by a dental professional, it is not available in shops or online. It is available to buy from the Maxillofacial Department at William Harvey Hospital.
Your GP or dentist will prescribe you Duraphat 5000ppm toothpaste free on a NHS for the rest of your life. It protects your teeth from tooth decay once your saliva is reduced after radiotherapy. Use twice daily. After brushing, spit out, do not rinse with water.
You can buy fluoride mouthwash over-the-counter. It is also available to buy from the Maxillofacial Department at William Harvey Hospital. It provides extra fluoride protection for your teeth against tooth decay. Use the mouthwash at least 30 minutes after brushing your teeth with Duraphat 5000ppm toothpaste.
Difflam mouthwash helps relieve pain due to ulcers or a burning sensation in your mouth. The Oncology team will give you this mouthwash before you start your treatment.
Chlorhexidine mouthwash is an antiseptic mouthwash. It is useful when you are unable to brush your teeth due to pain / soreness in your mouth. You may wish to dilute this mouthwash with warm water and rinse your mouth twice a day.
Do not worry if you are unable to clean your mouth during this time. You can use this mouthwash until you are able to brush your teeth again. The Oncology team will give you this mouthwash before you start your chemotherapy / radiotherapy.
Saliva substitutes help with mouth dryness. Mouth dryness is common during and after radiotherapy, due to the damage to your salivary glands. The amount of saliva you produce may improve but it can take several months or years. It may never return to your previous levels. You can try these saliva substitutes on an NHS prescription, but most people find frequent sips of water the best remedy.
Contact details
If you have any questions, please contact us Monday to Friday 8am to 5pm:
Restorative Dentistry reception desk
Telephone: 01233 616045Restorative Dentistry Secretary
Telephone: 01227 866317
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email