Dementia and short-term artificial feeding
Information for patients and their relatives / carers from the Dementia Team
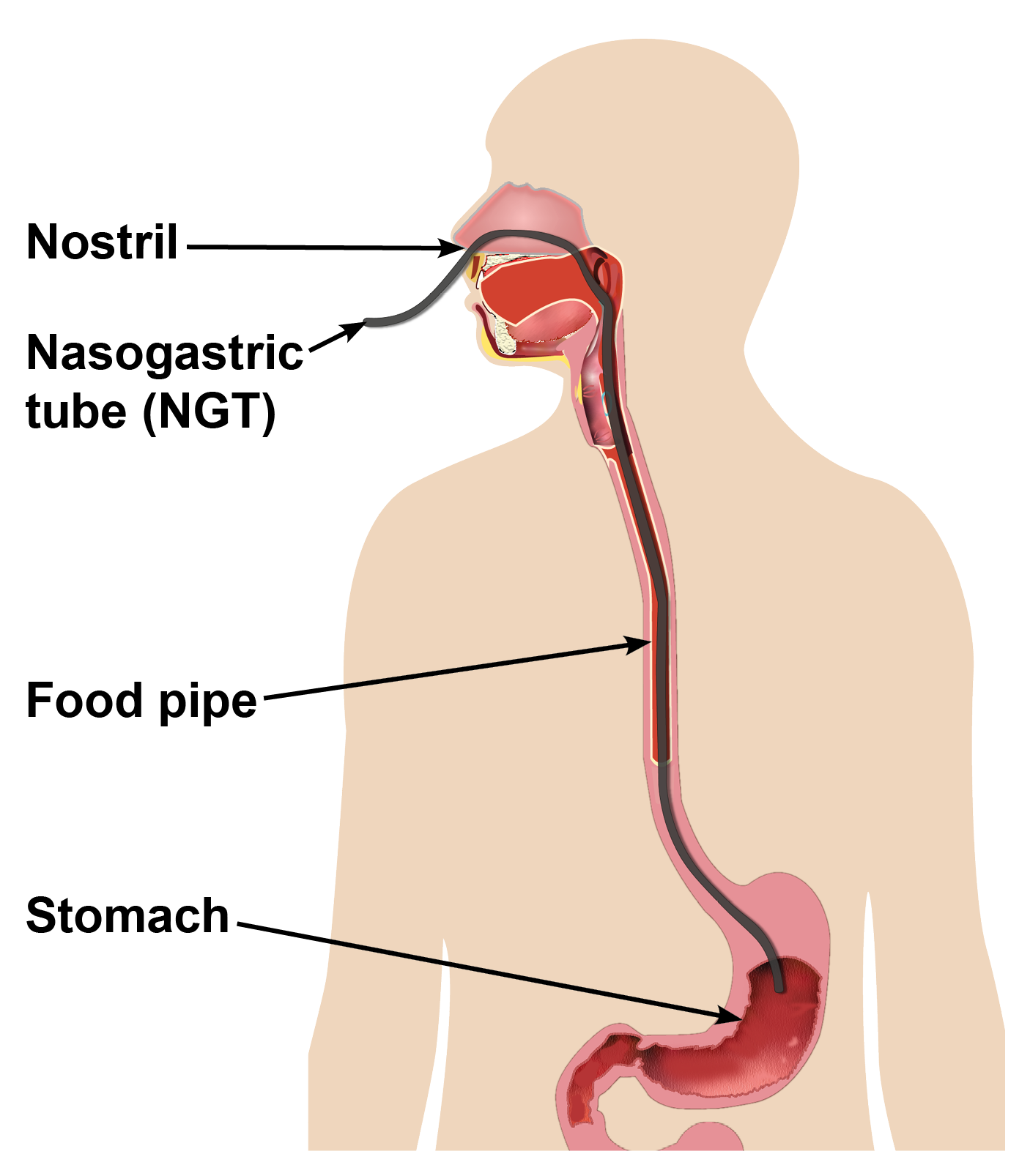
This leaflet is for people living with dementia and their relatives / carers. It explains what nasogastric tube feeding (NGT) is, and why it is important.
What is dementia?
Dementia is an umbrella term for a range of progressive conditions that can affect memory, problem-solving skills, language, and behaviour.
Difficulties with eating and drinking are common in people living with dementia, and they may not eat enough to meet their nutritional needs. If this happens nasogastric tube (NGT) feeding may be considered.
Why can people living with dementia have problems with eating and drinking?
Common reasons for changes in eating and drinking habits include:
forgetting to eat and drink
not feeling hungry or thirsty
difficulties concentrating
changes in taste / likes / dislikes
low mood
painful mouth / sores / tooth decay
infection (for example chest infection and pneumonia)
constipation (problems with bowel movements)
swallowing difficulties.
This list is not exhaustive and many of these causes, such as constipation, can be treated without the need for artificial (nasogastric) feeding (for example making changes to what you eat or taking laxatives can help some patients).
However, as dementia progresses, the person living with dementia may start eating less than before, and you may notice that they are coughing after eating or drinking, or have difficulties swallowing.
What is short-term artificial feeding?
Artificial feeding is a way of delivering nutrition directly to the body, without a person having to swallow and chew food themselves. Most commonly, this will be done through a nasogastric tube.
Artificial feeding will normally be considered if:
the person is having an acute (short-term) illness that is affecting their ability to swallow, or
the amount of food they are eating is not enough for their bodies to heal and recover from their illness.
In these cases, artificial feeding is used for a short period of time, to help the patient recover from this acute illness.
For example, a person may be admitted to hospital with a chest infection. They may become very poorly and are not eating and drinking as well as they did previously, or become too drowsy and cannot safely swallow, which has an effect on their ability to recover. NGT may be inserted for a short period of time to make sure that the person is getting enough nutrition to help them recover. However, this becomes more difficult when the person is very frail, has multiple chronic (long-term) conditions, has been living with dementia, or they have not been eating well before their acute illness.
What is a nasogastric tube (NGT)?
A nasogastric tube (NGT) is a tube that is inserted through the nostril, down the food pipe directly into the stomach. This is done by a specially trained practitioner at your family member’s bedside. Once the tube is in place, it is secured to their cheek with tape.
To check the tube is in the right position, the patient will have a pH test (or occasionally an x-ray) before the feeding or medication is first given.
What is a pH test?
During a pH test, a sample of stomach fluid is taken through the NG tube and placed on a pH strip. Stomach fluid is naturally acidic, and pH strips measure the level of acidity and confirm that an NG tube is indeed in the stomach. If staff are unable to gather a sample of stomach fluid, or the pH level is not in the right range of acidity, an x-ray is used to confirm the position of NG tube.
What are the common difficulties with NGT feeding?
Insertion of the tube can be distressing and uncomfortable for the patient. However, the practitioner will always talk you and your loved one through what is going to happen, and answer any questions you may have. They will also try to relieve any discomfort or distress your loved one may feel, by offering reassurance and a step by step explanation of what is being done, stopping if the person becomes very distressed.
The patient may forget the tube is in place or it may bother them, and they can pull it out. This can lead to the tube being reinserted a number of times.
The position of the tube is always checked using pH strips, before any food or medication is given to the patient. If the position cannot be confirmed by pH, an x-ray may be needed instead. This can sometimes lead to delays in the patient getting the food and medication that they need.
Rarely, pressure sores may develop around the nostrils. Daily checks of the area around the nostrils can help prevent this. Daily checks are carried out by the ward staff. However, should you notice a sore developing around your relative’s nose, please tell the staff nurse looking after them.
Who will give permission for NGT to be used?
Dementia can affect a person's ability to consent to NGT feeding, and very often they need a mental capacity assessment to assess whether they are able to make this decision themselves. If the person can make this decision, they can.
If a person living with dementia needs NGT feeding and they do not have capacity to consent to this, a wider discussion may be needed about the reasons for the NGT feeding, including what they would have wanted and what is in their best interest. This discussion is between different professionals looking after your relative (most often doctors, dietitians, and speech and language therapists), and you as their next of kin. However, as NGT feeding is considered to be a form of medical treatment, the responsibility and final decision lies with the consultant looking after your relative.
If it has been decided that your loved one no longer has capacity to make this decision themselves, a member of the medical team will talk to you about what happens next. The following are questions that will be discussed with you. No decisions will be made, unless they are in the best interest of your loved one.
Has the person with dementia been eating less and less before they came to hospital?
Have you ever discussed artificial feeding with the patient? Have they ever expressed any opinions or wishes before their dementia progressed?
What is your understanding and expectation from NGT feeding?
Do you have any concerns about NGT feeding? If so, please speak to a member of the team.
Is this a short-term illness, which the patient should recover from (such as an infection)?
How long will the tube be in place for?
What is going to happen if the person with dementia pulls the NGT out or are really distressed by it?
Will using NGT feeding help?
The progression of dementia often causes irreversible swallowing difficulties or reduced food and fluid intake. Studies have shown that for dementia related swallowing difficulties, there is no increased benefit of using NGT feeding, and people having NGT did not live any longer than those without it.
If your loved one lacks capacity and the decision is reached to offer NGT feeding, it will be inserted under the Deprivation of Liberty Safeguards (DOLS). This means that the procedure carried out is not something the patient had ability to consent to. DOLS is also needed if retention devices are used (see below).
What are retention devices?
Retention devices are used if the person living with dementia is likely to pull out their NGT or have pulled an NGT out before. These include mittens and a nasal bridle.

Mittens are large white gloves that are placed on the person’s hands to stop them from tugging on their NG tube. However, this also means that they cannot freely move their hands and are unable to reach for things like a drink, snack, or a blanket. Because mittens are restrictive, their use is reviewed regularly and they would only be used as long as needed.
A bridle is inserted through the nostrils, and holds the NG in place with a small clip that sits just below the nostril. Insertion of a bridle can be distressing. The bridle does not fit all nose shapes, so it cannot be used for everyone.
Mittens and bridles make it more difficult for the person to remove their NGT, but not impossible. Also, not being able to use their hands can make them more distressed. If the NGT is pulled out with a bridle in place, this can hurt and cause the patient discomfort. If an NGT had been pulled out or causes distress, the healthcare professionals involved in your loved ones care will review and discuss with you whether to carry on with NGT feeding.
Reading this leaflet as a family member, friend or carer, can be difficult. It is only natural to want your relative to have any intervention possible and it can be extremely challenging seeing them decline or distressed. Please remember, you are not alone. There are many professionals that can support you, including the ward staff, the Nutrition and Hydration Team, speech and language therapists, dietitians, and the Dementia Team.
What if the decision is made not to use NGT feeding?
If the choice to try NGT feeding is not right for the person living with dementia, or if it has been tried unsuccessfully this does not always mean that they cannot eat or drink at all or that they will be in discomfort. Often modified texture foods can make swallowing easier and safer, while food supplements can help with meeting their nutritional and vitamin needs.
Sometimes the person continues to decline eating and drinking despite all efforts. This can be a sign that they are approaching the last months, weeks, or days of their life. Should this be the case, the medical team will talk to you about palliative and comfort care.
People having end of life care (last days of their life) are offered drinks and foods for taste and pleasure. People at end of life would not feel hungry, and it is not unusual for them to decline to eat or drink. If this is the case, staff will provide regular mouth care to avoid discomfort from dry mouth and the development of mouth sores. If you would like to provide mouth care for your relative or offer food and drinks for pleasure, please speak to a member of staff.
Support for you
If you are someone who is caring for a person living with dementia, these decisions can be difficult. It is important to us that you also feel supported throughout this process. Carer’s support packs are available on the ward and we are here for you, to talk you through any concerns or worries you may have.
Useful information and support
Alzheimer’s Society website has information around eating and drinking, alongside more information about Deprivation of Liberty Safeguards.
Support line: 0333 150 3456Dementia UK website has information around eating and drinking, and about looking after yourself.
Admiral Nurses Helpline: 0800 888 6678John’s Campaign. East Kent Hospitals has signed up for John’s Campaign, to give carers and families flexible visiting times. Please speak to the ward if you would like to visit under John’s Campaign.
If you are struggling yourself, the Everyturn website has information about free counselling and talking therapies.
The With you website has advice and help for people living in Surrey and Kent, on a range of mental health problems, including stress, anxiety, and depression.