Deep vein thrombosis (DVT)
Information for patients
What is deep vein thrombosis?
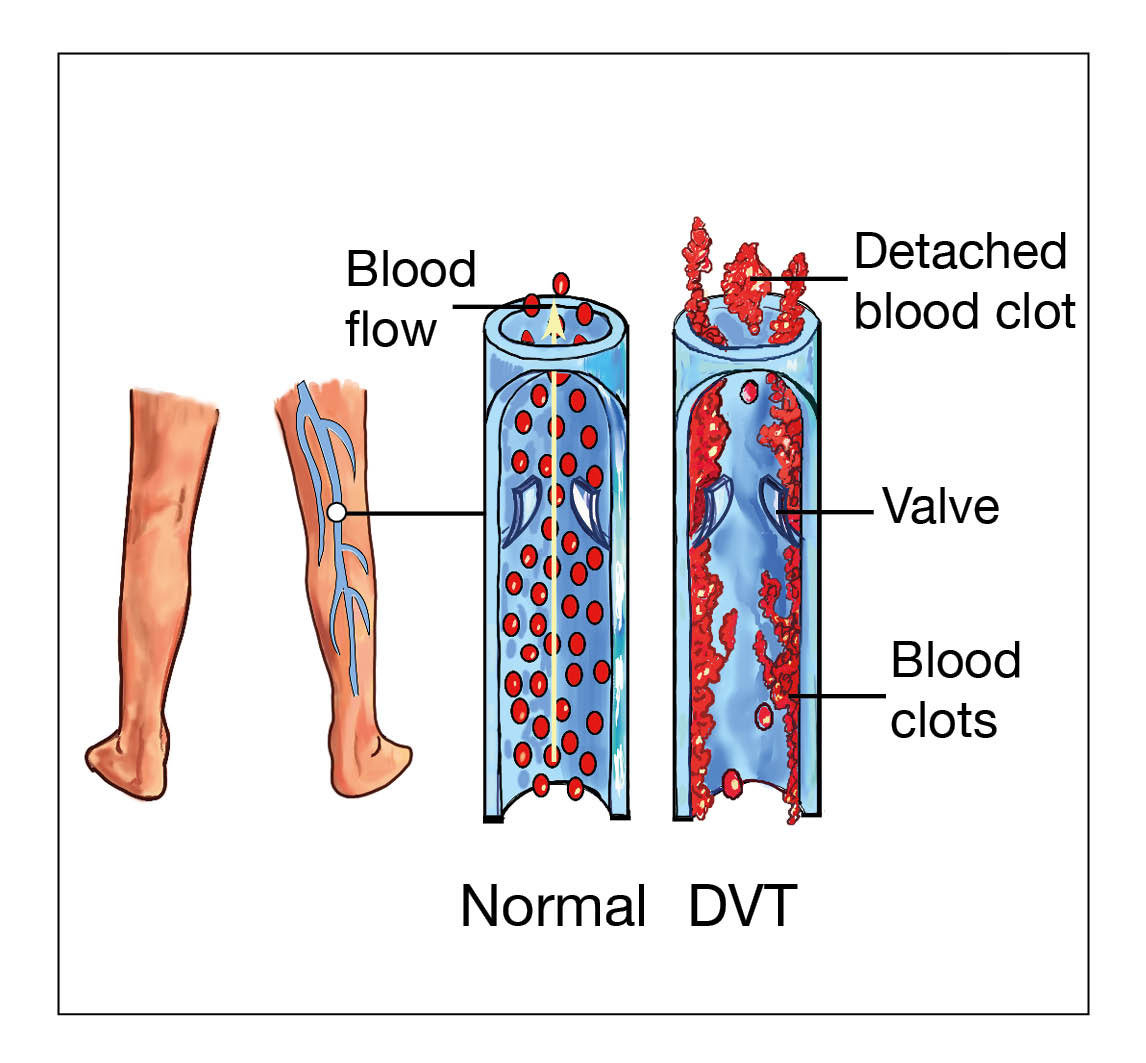
A deep vein thrombosis (DVT) is a blood clot which forms in a deep vein, usually in the leg, but can occur elsewhere in the body.
Deep veins are large blood vessels which return blood to the heart. These veins lay deep within the body and cannot be seen.
What are the symptoms of a DVT?
These will vary according to the size and position of the clot. Not everybody has all of these symptoms but usually you will have some pain, swelling, and discolouration of the area and sometimes it can be hot and sore to touch. Further advice on how to manage these symptoms can be found further on in this leaflet.
What tests will I have in hospital?
Blood tests. You will have blood taken from a vein in your arm, this may be a routine blood test or to monitor you whilst taking medication to treat your DVT.
Doppler ultrasound gives the radiologist a picture of the veins and the sound of the blood flowing in them, showing whether or not a clot is there. This takes about 15 minutes.
Chest x-ray. Occasionally part of the clot can dislodge and travel in the blood stream to the lungs (this is known as a pulmonary embolism). Although the chest x-ray does not diagnose this, it can help the doctor to decide if there is any other condition present (such as infection) and if any other test is needed (usually a scan).
What is the treatment of a DVT?
Your body will naturally break down the blood clot, but in order to do this safely you will need to take anticoagulant medication. Anticoagulant medication works to prevent the clot from getting bigger or moving, or from new clots forming.
Anticoagulation may be given as Warfarin tablets, heparin injections, a combination of the two, or more often oral anticoagulant tablets called direct acting anticoagulants (DOAC). All these medications have trade names as well as the generic names used in this leaflet.
Apixaban is an oral anticoagulant. If taken from when a blood clot is first diagnosed, it is taken at a higher loading dose for one week, and then continues on a fixed dose twice daily thereafter. After the first one week loading period, the treatment dose usually does not change and there is no need for blood tests to monitor its effect.
Your kidney and liver blood tests will need to be checked before and every three to six months during treatment with this drug, as this is how your body processes the drug.
Rivaroxaban is an oral anticoagulant. If taken from when a blood clot is diagnosed, it is taken twice daily for three weeks and then once daily thereafter. After the first three weeks, the dose usually does not change and there is no need for blood tests to monitor its effect.
Your kidney and liver blood tests will need to be checked before and every three to six months during treatment with this drug, as this is how your body processes the drug.
Heparin injections are given according to your weight and kidney function. Heparin is usually given once daily (occasionally twice daily) in to the skin of your abdomen. It is often given as a low molecular weight heparin such as Enoxaparin, Fondaparunux, Dalteparin, or Tinzaparin. You may be taught how to administer it yourself or a nurse may do this for you. You may have to take a heparin injection until fully diagnosed or until a treatment like Warfarin is fully effective.
Warfarin tablets are an oral anticoagulant and come in three different colours and doses:
1mg: brown tablets
3mg: blue tablets
5mg: pink tablets.
When taking Warfarin, you will have regular blood tests to monitor your INR (International Normalised Ratio). This is a measure of how long it takes for your blood to clot.
The dose of Warfarin will differ according to your INR. Your specialist will tell you what to take, and when, according to your blood test.
You should only be on one anticoagulant, although a few days overlap is necessary if you are changing to Warfarin or Acenocoumarol.
Other oral anticoagulants are Dabigatran, Edoxaban, and Acenocoumarol. You will only be advised to use these if they have advantages for you compared to the ones mentioned above.
Some patients with a DVT might need other treatments, such as anti-embolic stockings (AES). Some medications, such as some oral contraceptive pills, may increase the risk of a DVT and might have to be changed.
What are the side effects of anticoagulants?
All anticoagulants increase your risk of bleeding. Be extra careful when cutting nails, shaving, or using sharp implements. If you do have any bleeding, apply extra pressure on the affected area and ask for medical help if it does not stop. You are also at increased risk of bruising.
Some people complain of feeling cold when taking anticoagulants.
Heparin can potentially cause your platelets (a clotting component in the blood) to drop in the first few weeks of taking it. Your blood will be tested regularly when you first start taking heparin to check for this.
There are some medications, such as aspirin, clopidogrel, dipyridamole, and ticagrelor which often should not be taken with anticoagulants or be taken with dosage adjustment; your specialist will advise you on this. Some herbal medications and food types also interact with certain anticoagulants; your specialist will advise you on this.
It is important that you make sure the person starting you on an anticoagulant knows all the medications you are taking. You should tell any doctor, dentist, or nurse that you are taking an anticoagulant when you attend with an injury or for a procedure, or if they are prescribing you a new medication.
What will happen if I do not want to take anticoagulants?
You are strongly advised to take the anticoagulants.
If untreated, a DVT can break off and the clot can travel to your lungs where it causes a pulmonary embolism (PE), which can be fatal. Most people who have a DVT and take anticoagulants usually recover without complications.
Do I need to stay in hospital?
Not usually. If you are relatively well with your DVT, you are most likely to be treated as an outpatient.
How long will I be on anticoagulants?
You will need anticoagulant medication for at least six weeks, often up to three months, but sometimes longer. We do not routinely rescan your leg during or after treatment with anticoagulants.
If you are on Rivaroxaban, Apixaban, or heparin injections, you will usually be referred to the anticoagulant outpatients early on in your treatment. The specialist staff at the anticoagulant clinic will confirm the length of your treatment and arrange follow-up as needed. You will be contacted for an appointment within six weeks of your first diagnosis. Please make sure the hospital has your correct contact details, including any changes to your address or phone number.
If taking Warfarin, you will usually be referred to the anticoagulant clinic as an outpatient. The anticoagulant clinic staff will continue to monitor your INR and Warfarin. Once your INR is ‘stable’ (remains at an acceptable level), you will be referred to an anticoagulant clinic closer to your home.
What can I do to help my recovery?
Try and stay mobile and walk normally as much as you can.
Try not to walk on tip toe, as this may cause you to develop a stiff knee joint and which will cause more problems later on. If you are having any problems, please let us know.
If you have pain and swelling for more than two weeks after starting treatment, wearing anti-embolic stockings may help. Your GP may be asked to assess and prescribe British Grade 3 / European Grade 2 (25 to 35 mmHg) below the knee stockings, to be worn during the day for two years (not at night).
Listen to your body. If you do anything that makes you feel breathless or increases pain, stop.
Until the DVT starts to improve, you may feel some discomfort. Take the painkillers which have been prescribed for you. Avoid over-the-counter pills unless discussed with your specialist.
Stay mobile as your pain allows. But when sitting, keep your legs elevated (raised), ideally above the level of your hips, unless told otherwise by your specialist. This will help with blood flow and reduces the level of leg swelling.
Look after yourself. Eat a healthy diet and drink plenty of fluid. Your mobility may be restricted to start with due to pain and breathlessness; this will increase your risk of constipation.
When attending your appointment, please bring a list of your medications with you. You may also be asked to discuss your medical history. It is important that this information is shared with the doctor or nurse who is seeing you so we can safely treat and manage your diagnosis. All information is kept private and confidential.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email