Cyclodiode laser treatment
Information for patients from Ophthalmology
Cyclodiode laser treatment is used to manage glaucoma, by lowering intraocular pressure. The following explains:
What cyclodiode laser treatment is.
Why the treatment has been recommended.
What you can do before your treatment, to help with your recovery.
What the alternatives are.
What happens during and after your treatment.
Who to contact if you have any questions.
We hope this leaflet answers some of the questions you may have. If you have any further questions or concerns, please contact the Urgent Eye Service using the details at the end of this leaflet.
What is cyclodiode laser treatment?
Cyclodiode laser treatment uses laser energy to reduce the production of aqueous humour. Aqueous humour is the fluid inside the eye. This is done by destroying part of the ciliary body, the part of the eye which produces aqueous fluid. The treatment can reduce the amount of fluid produced and therefore reduce pressure inside the eye.
During treatment, a laser probe is placed on the surface of the eye. Pulses of laser are passed through the eye, to reach the ciliary body. This disrupts the fluid production, and reduces the amount of fluid being produced.
Why has this procedure been recommended?
Cyclodiode laser is usually recommended when other treatments to control eye pressure are not suitable or have not worked. Other treatments may include eye drops or surgery.
It is commonly used for patients with glaucoma, when high intraocular pressure:
poses a risk to sight; or
is causing you significant eye pain.
The treatment does not cure the underlying condition. However, it often significantly reduces pressure in the eye and helps preserve existing vision. Some patients need repeated laser treatment or further procedures to maintain these benefits.
Will I have to stay in hospital?
Cyclodiode laser is usually performed as a day case, in an outpatient clinic. This means you will be able to go home the same day, without needing to stay in hospital overnight.
Do not drive yourself home after your procedure. Arrange for someone to collect you from hospital and take you home.
Are there any alternatives?
Alternative treatments of high eye pressure include:
topical eye drops
oral medications; and
surgery, such as trabeculectomy or tube surgery.
You will discuss these treatments with your surgeon before any decisions are made.
What happens if I choose not to have treatment?
If you choose not to have any treatment, your eye pressure may continue to rise. This can lead to progressive and irreversible damage to the optic nerve, which can result in permanent loss of vision.
Is there anything I can do before treatment to improve my recovery?
Make sure your blood pressure and any other medical conditions are under control.
If you smoke, try to stop. Compared to non-smokers, smokers are more likely to have complications in tissue healing and infections after injuries or surgery. For free friendly support and medication to help you stop smoking, contact One You Kent.
One You Kent
Telephone: 0300 123 1220
Email
Follow the advice given to you by the hospital.
What will happen when I arrive at hospital?
Please refer to your appointment letter or email for where to go when you arrive at the hospital.
A member of the clinical team will welcome you and discuss the procedure with you. They will ask you to sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of:
medical treatment
test; or
examination.
Consent is usually given when you sign the consent form before your treatment. We may ask you to give your consent verbally (spoken rather than written consent).
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. Please speak to staff if:
staff have not given you this information; or
they have but you still have questions.
You must be capable of giving consent. This means you understand the information given to you, and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
Who will perform the procedure?
An ophthalmologist (eye doctor), with experience in laser treatment, will perform the procedure.
Will I have anaesthetic?
Yes. The treatment is usually performed under local anaesthetic (the treated area is numb but you are awake). The anaesthetist usually uses a blunt needle to fill the tissues around the eye with anaesthetic drops. While the anaesthetic is given, most patients only experience mild pressure or a light touching sensation. This quickly passes. Once the anaesthetic takes affect, the laser procedure is painless.
Please lie still during the treatment.
Can I eat and drink before my procedure?
Most patients can eat and drink as normal before their procedure. If this is not the case for you, the reason will be explained at your pre-assessment appointment.
Will additional procedures be necessary?
In some cases, further laser treatment or alternative procedures may be needed if:
the eye pressure does not reduce enough; or
the eye pressure increases again in the future.
If this is needed, your surgeon will discuss this with you at your follow-up appointment.
Are there any risks to having the procedure?
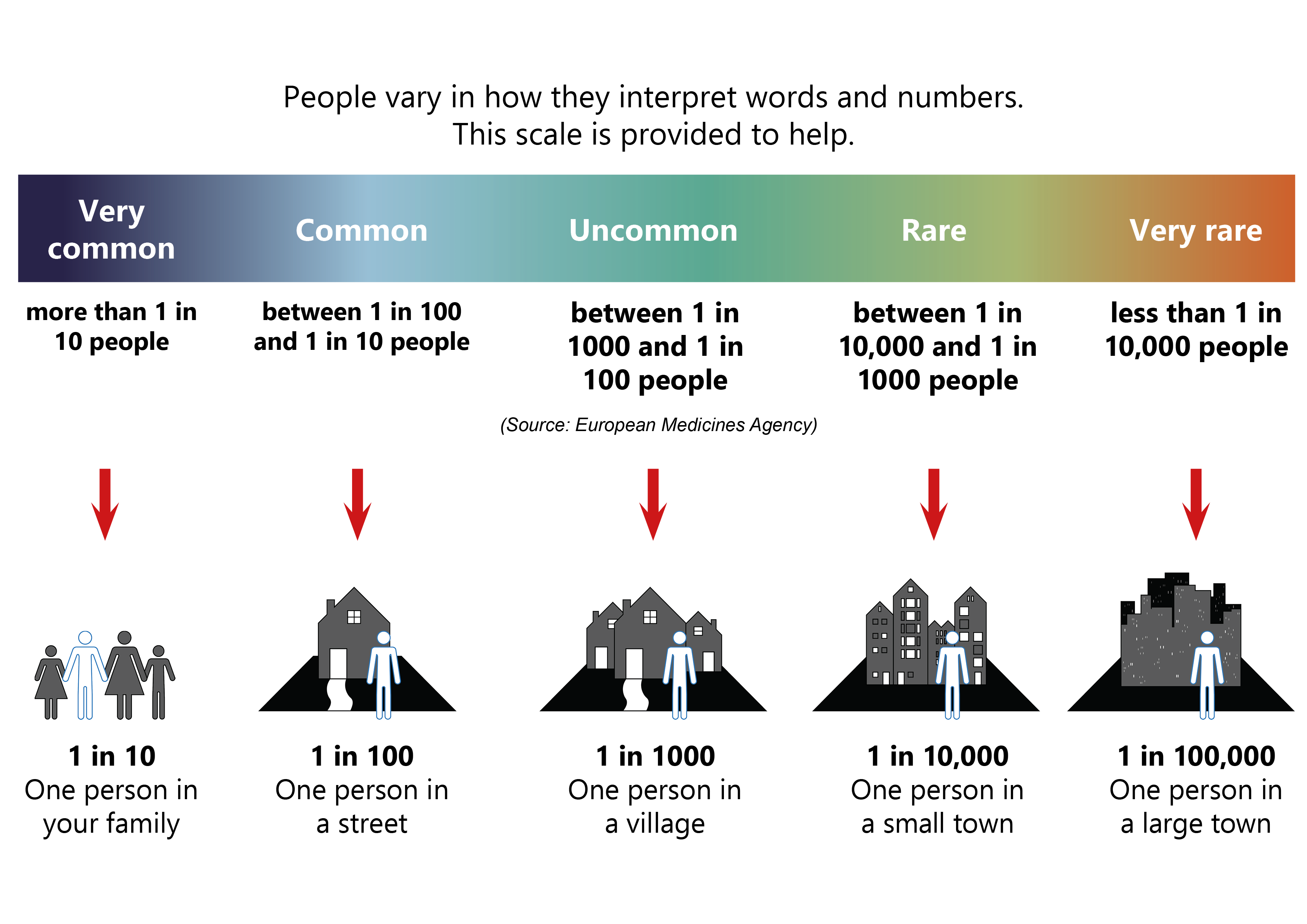
Like all procedures, cyclodiode laser treatment carries some risks.
The following risks are often temporary.
Bloodshot eye (common). This should settle on its own after a few days.
Discomfort or inflammation in the eye (common). Please use the eye drops given or paracetamol for pain. This should settle within a few days.
Reduced vision for up to 6 weeks (uncommon).
Damage to surrounding structures, such as cornea, conjunctiva, sclera, iris, lens, and retina (very rare).
Bleeding and infection (very rare).
The following can be permanent.
Loss of sight (very rare).
Sometimes the treatment fails or you need further treatment. You will discuss this with your surgeon.
If you have any questions or concerns about these risks, please speak to your surgeon.
Are there side effects of any drugs used?
The local anaesthetic and any eye drops prescribed after surgery may cause redness and irritation. Allergic reactions are rare. If your eyes become red or inflamed when using the drops, please contact the Urgent Eye Service for advice.
Please read the information provided with any prescribed medication. Tell staff if you have any known allergies.
How will I feel after the procedure?
You may feel some eye discomfort or pain, which usually settles within a few days. Common painkillers (such as paracetamol or ibuprofen) may help.
Do not rub your eyes. Follow all instructions regarding eye drops or other medications.
Continue using your usual eye drops after your procedure. We will tell you if and when they can be reduced or even stopped.
Do not drive on the day of your procedure. Only drive again once you can see clearly, and your eyesight is no longer blurred. Arrange for someone to take you home after your appointment.
Most patients need 1 to 2 days off work.
You can resume normal activities once your eye feels comfortable and your vision is stable. Normal activities include sport, gardening, and housework.
Will I need a follow-up appointment?
Yes. At your follow-up appointment your surgeon will check whether the treatment worked. They will also discuss with you any complications you have experienced. You will be told the date of your follow-up appointment before you leave hospital.
When will I know if the treatment has worked?
You may not notice any improvements straight away. Sometimes if can take a few weeks to notice a difference. The outcome of the procedure will be assessed at your follow-up appointments. This is usually done through eye pressure measurements and examination.
What should I do if I feel unwell at home?
If you experience any of the following, contact the Urgent Eye Service immediately.
Severe eye pain, not helped by paracetamol or ibuprofen.
Significant swelling or discharge from the eye.
Sudden / severe loss of vision.
Further information
[Websites last accessed 24th September 2025]
Contact details
Urgent Eye Service, Ophthalmology Department
Telephone: 01233 616232
Email
Opening hours: Monday to Friday, 9am to 5pmFor out-of-hours queries, call the main switchboard at William Harvey Hospital. They will direct you to the on-call ophthalmology doctor.
William Harvey Hospital, Ashford switchboard
Telephone: 01233 633331
Ask 3 Questions
There may be choices to make about your healthcare. Before making any decisions, make sure you get the answers to these three questions:
What are my choices?
What is good and bad about each choice?
How do I get support to help me make a decision that is right for me?
Your healthcare team needs you to tell them what is important to you. It’s all about shared decision making.
What do you think of this leaflet?
We welcome feedback, whether positive or negative, as it helps us to improve our care and services.
If you would like to give us feedback about this leaflet, please fill in our short online survey. Either scan the QR code below, or use the web link. We do not record your personal information, unless you provide contact details and would like to talk to us some more.
If you would rather talk to someone instead of filling in a survey, please call the Patient Voice Team.
Patient Voice Team
Telephone: 01227 868605
Email