Corneal graft transplant
Information for patients from Ophthalmology
This leaflet is not meant to replace the information discussed between you and your doctor, but can act as a starting point for such a discussion or as a useful reminder of the key points.
You have been told by your eye surgeon that you need a corneal graft (transplant). This leaflet explains what happens next, and aims to answer any questions that you may have. We hope it will help you to reach a decision on whether you wish to have the operation.
What is the cornea?
-1721383839.jpg)
The cornea is the clear tissue covering the front of the eye.
It is the main focusing element of the eye. If your cornea becomes cloudy from disease, injury, or infection you will find it harder and harder to see.
Why do I need a corneal graft?
Sometimes through injury, infection, or some inherited condition (such as keratoconus) your cornea may lose its natural transparency or normal shape, leading to blurred vision. In many cases glasses or contact lenses may help you to see more clearly, but there are times when these do not work and the cornea needs to be replaced with a graft / transplant.
What is a corneal graft?
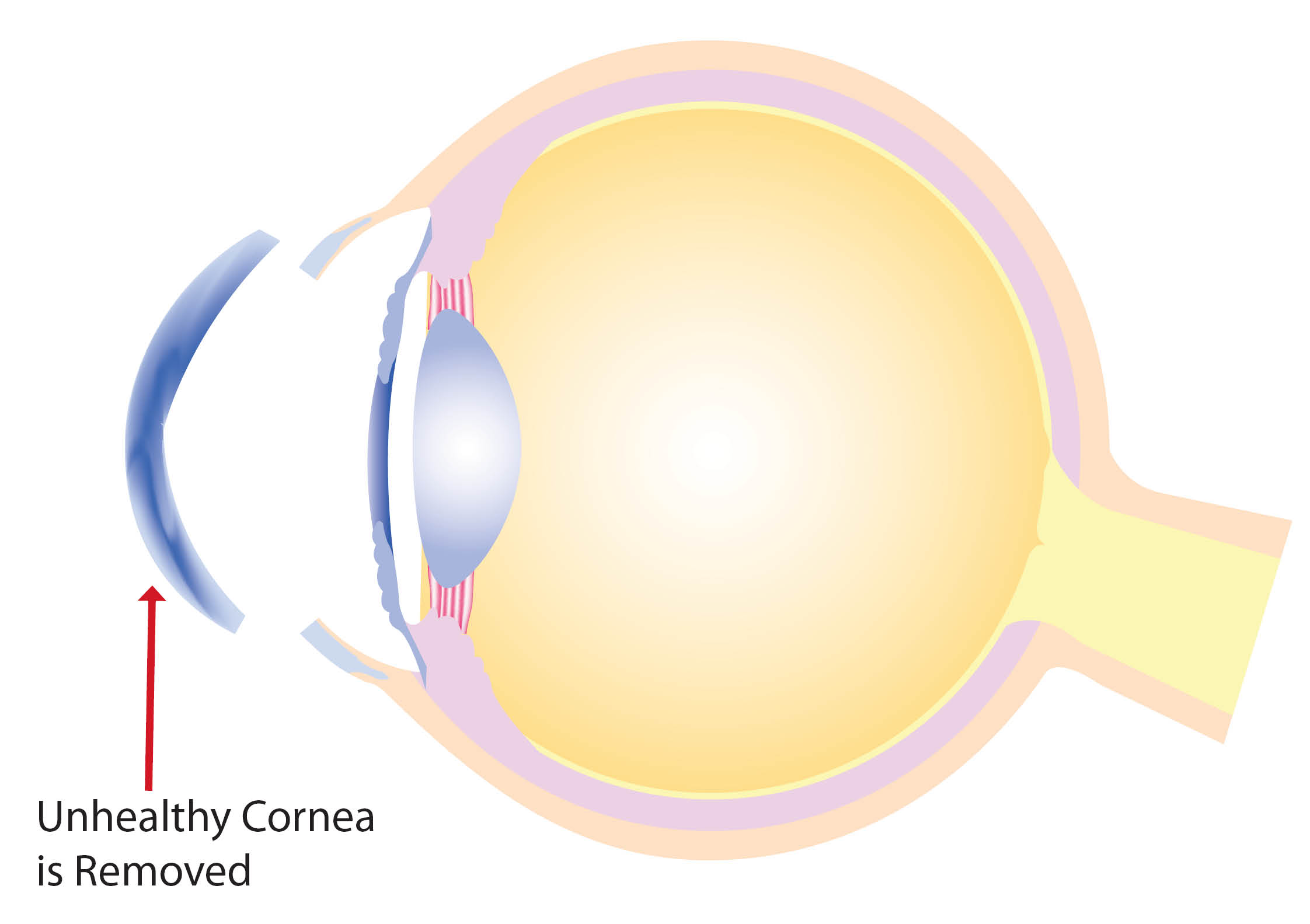
A corneal graft is a surgical procedure which replaces a disc shaped part of the cornea (typically about seven to eight millimetres in diameter) with a similarly shaped piece of donor cornea.
There are three types of corneal graft surgery.
Deep anterior lamellar corneal graft. If only the surface layers of the cornea are unhealthy, these layers are removed and replaced by a graft.
Corneal endothelial graft. If it is the inside layer of the cornea that is unhealthy, only this is removed and replaced by a graft.
Penetrating corneal graft. If the whole thickness of the cornea is unhealthy, the patient’s whole cornea is removed and replaced with a graft.
Who decides which surgery I will have?
You will discuss this with your surgeon, and they will advise you as to which is the most appropriate surgery for you.
What do I need to do before I come in for surgery?
Continue with all your current medication, unless told otherwise.
You may wear your glasses or contact lenses until your admission to hospital.
You should follow the instructions about eating and drinking that you have been given.
The fitter you are at the time of surgery the quicker you may recover.
It is important that you follow any instructions that you are given both before and after surgery, as this will help your recovery.
What happens when I arrive at hospital?
Please refer to your appointment letter for where to report to when you arrive at the hospital. You will be greeted there by a member of the ward staff and introduced to your named nurse. They will discuss with you the care you will have while you are in hospital.
You will be seen by the surgeon before your operation and asked to sign a consent form. Please make sure that you ask any questions before you sign this form, so you completely understand your operation. Please remember that you can withdraw your consent for treatment at any time.
Will I have general anaesthetic?
If you are having a general anaesthetic (you are asleep for the procedure) you will also meet with the anaesthetist before your surgery. Please raise any questions or concerns you may have about the anaesthetic with the anaesthetist.
How long will I be in hospital?
This operation is usually carried out as a day case, so you will go home the same day as your surgery.
How is the graft held in place?
If the surface or all of your cornea is replaced, the graft is sewn into place with microsurgical instruments. The sutures (stitches) will remain in place for several months after your surgery. The time and rate at which the sutures are removed varies from person to person, but may take up to two years. This will depend on your recovery and vision.
If only the inside layer of your cornea is replaced, the graft is put into your eye through a small incision (cut) and is held in place by an air bubble that will dissolve after two to three days. The incision is closed with sutures which can be removed after one month (in clinic by the ophthalmologist). You will be asked to lie flat for several hours after your surgery to help the air bubble keep the graft in place.
What happens after my surgery?
For deep anterior lamellar grafts and penetrating corneal grafts the sutures will need to stay in place for several months. You should not feel these sutures as they are very thin. Treatment with drops is needed and continues for several months (how long you use the drops will depend on your recovery and vision). You will be shown how to use the eye drops before leaving hospital.
Close follow-up is very important and you will need to come to clinic (usually at Kent and Canterbury Hospital where we have the correct equipment to map your cornea and assess your recovery) on a frequent and regular basis. To begin with, this may be weekly and then monthly. Your first appointment will usually be a week after your operation and will be arranged before you leave the hospital after your surgery.
The recovery of your vision after a corneal graft happens gradually after several months. The final result is only obtained once all the sutures have been removed; this is done in the Outpatient Clinic and it may take over a year before all the sutures are removed. The sutures are usually removed over several appointments, perhaps only one or two at a time depending on your vision and recovery.
For corneal endothelial grafts, recovery of vision is usually faster (approximately three months) and sutures can be removed in hospital after one month. Your first appointment for suture removal will be made before leaving hospital. Treatment with drops is also needed (see above) and continues for several months, again this depends on your vision and recovery.
To get the best visual results after any corneal graft surgery, glasses or contact lenses may be needed.
How will I feel after my surgery?
Your eye may be uncomfortable for a few days after your operation; this should be controlled with over the counter painkillers, such as paracetamol. You will be prescribed stronger painkillers if your doctor thinks it necessary.
You will not be able to drive home or use a mobility scooter after your procedure;
this is because of the drops. Please bring someone with you on the day of your surgery, or make suitable transport arrangements, so you can get home after your surgery. You may start driving the day after your surgery, when your vision has returned to normal.
Are there any risks?
There are complications that can arise during or after corneal grafting. These include general complications that may happen whenever the eye is operated on, such as infection or sudden haemorrhage (bleeding) within the eye. Either of these can result in blindness but the risk of these happening is very low.
For deep anterior lamellar and for penetrating grafts, complications include:
problems related to sutures, which can break and lead to infection or rejection of the graft
astigmatism (a defect in the eye which prevents proper focussing) which happens frequently after such surgery; you may need glasses, contact lenses, or further surgery to correct this
primary graft failure is rare; this is where the graft never clears after being transplanted into the eye and results in poor vision.
For corneal endothelial grafts, suture related problems and astigmatism are less of a problem. The main complication is failure of the graft to stick to the patients own cornea, as the graft is not stitched into place but held by an air bubble that dissolves on its own. This would need a further bubble of air to be put into the eye with the patient again lying flat for a few hours. Because these endothelial grafts are very delicate if there are problems in getting the graft into the eye at the time of surgery, primary graft failure is a bigger risk than with the other grafts.
What are the chances of my graft rejecting?
Unfortunately your body can reject the graft at any time (even years) after surgery. The risk of rejection varies depending on the underlying disease that needed corneal grafting in the first place, but it can happen in all corneal grafts.
If the rejection is not treated quickly it may result in failure of the graft. Although graft rejection appears to happen most often after penetrating (full thickness) corneal graft surgery, it may happen with all three forms of corneal graft. Therefore it is essential that a patient with a corneal graft be prepared to contact the Eye Casualty Department at William Harvey Hospital Ashford on 01233 633331 and ask for the on-call ophthalmology doctor as soon as their eye becomes red, sensitive to bright light, blurred, or painful. Any of these signs may be related to early rejection of the graft, which needs to be treated as an emergency if the graft is to survive (usually with steroid drops, but occasionally with tablets).
If for any reason you feel that you will not be able to quickly contact the Eye Casualty Department it may be preferable for you not to go ahead with the surgery. Please discuss this with your surgeon.
Where does the donor cornea come from?
Donor corneas come from a patient who has died and whose family have consented to tissue being donated.
Are the donor corneas safe?
All donor corneas are processed by the UK Transplant Service Eye Bank, where they are screened for transmitted diseases and are assessed regarding suitability for use as graft material. All donor corneas are screened for HIV, syphilis, and the hepatitis B and C virus, and will have been quality checked to make sure that they are safe to transplant.
Will I know where the donor cornea came from?
No. The gift of sight is made anonymously. Specific information about the donor family is not available to the recipient. However, should you wish to convey your thanks to the donor family these will always be passed on.
How often is corneal transplantation surgery carried out?
Corneal grafting was pioneered in the UK in the 1930s. Technical advances over the last 30 years have made this one of the most frequently performed human transplant procedures. There are over 2000 sight saving corneal transplants carried out each year.
How successful is corneal transplantation?
Over 96% of all corneal transplant operations (more than 96 out of 100 operations) successfully restore the corneal recipients sight.
Is there an alternative to using donor corneas?
There is no substitute for human tissue. The transplantation process depends upon the gift of corneal donation from one person to another.
What will happen if I choose not to have the corneal graft?
If you choose not to go ahead with the corneal transplant then you will need to discuss with your consultant how this will effect your condition.
What should I consider before I make my decision?
It is important that you understand that:
the return of good vision after surgery takes a long time
many and frequent visits to the clinic will be needed in the early stages after your surgery
further surgery may be needed to deal with the astigmatism in the graft
rejection of the graft may happen at any time after surgery, which would need urgent attention.
If you think any of the above points may cause a problem, you must discuss this with your eye surgeon before having your corneal graft.
What should I do if I am worried about my eye?
Please remember that most patients have a very good result from their surgery. If you develop any problems following your operation, please do not hesitate to call us using one of the numbers below.
Kent and Canterbury Hospital, Canterbury
Waiting List Coordinator
Telephone: 01227 866444Ophthalmology Suite
Telephone: 01227 866493
Queen Elizabeth the Queen Mother Hospital, Margate
Waiting List Coordinator
Telephone: 01843 234364Day Surgery
Telephone: 01843 234458
William Harvey Hospital, Ashford
Waiting List Coordinator
Telephone: 01233 616757Channel Day Surgery
Telephone: 01233 616263