Colonoscopy
Information for patients from the Trust's Endoscopy Units
This information is for patients who are having an examination of their large bowel known as a colonoscopy. It explains what is involved and any significant risks that there may be.
If you do not attend your appointment without telling the Endoscopy Unit in advance you may be removed from the waiting list.
Students and trainees supervised by qualified staff may be involved in your care. If you do not want students and trainees to be present, please tell the endoscopist or nurse in charge. The time stated is your booking in time, so please tell those coming to hospital with you that this is not your procedure time.
The test itself takes 20 to 40 minutes, and may take longer if any polyps (projections of tissue rather like warts) are removed. Normally you will be able to go home about 45 to 60 minutes later. Occasionally, if there are emergency or very complex cases, the start of your procedure may be delayed and you may be in the hospital for up to four hours.
What is a colonoscopy?
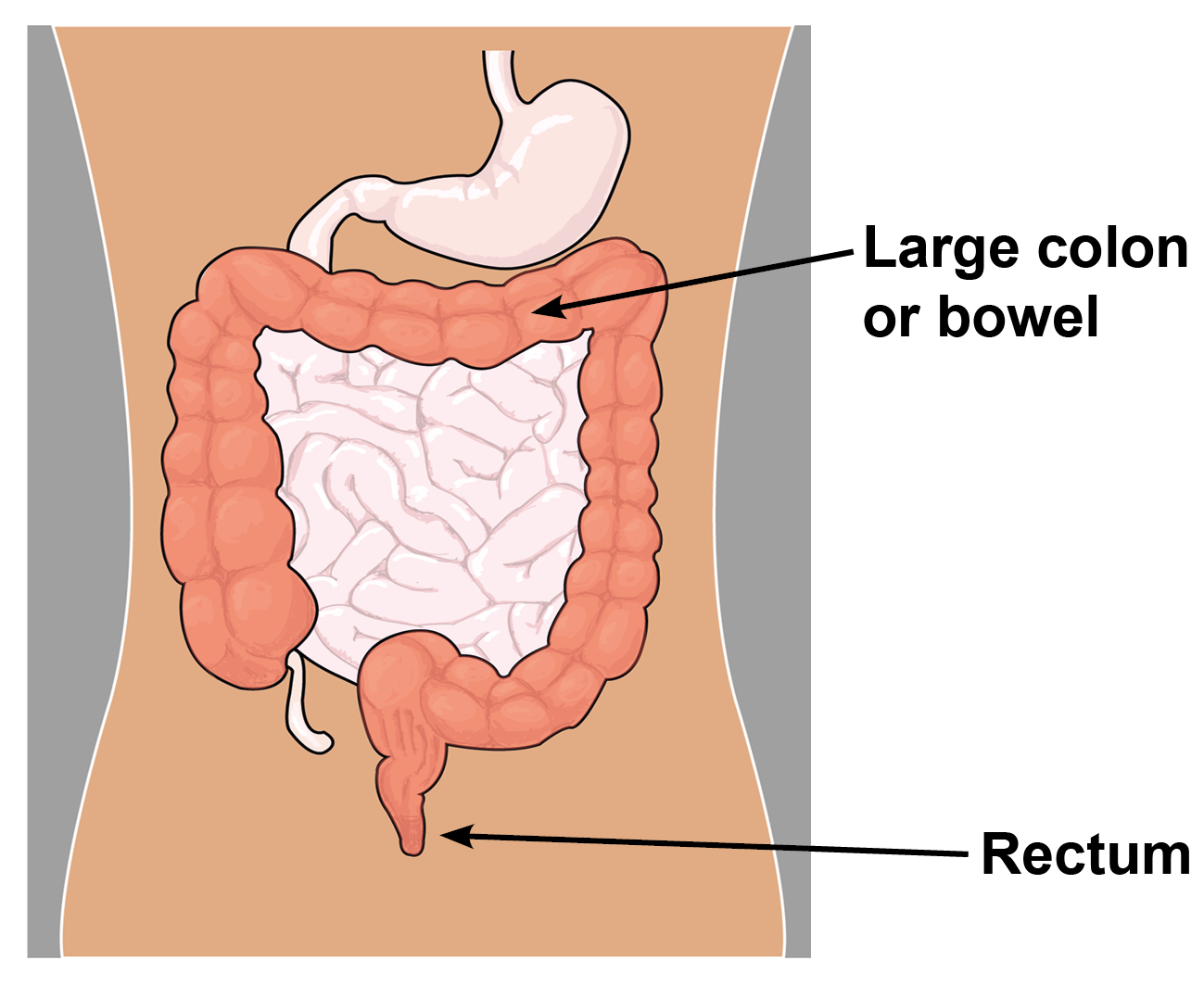
A colonoscopy is an examination which allows the endoscopist to look directly at the lining of the large colon or bowel using a colonoscope. This is a flexible tube about the thickness of a woman’s index finger.
Sometimes a sample of the lining of the bowel (a biopsy) is taken for laboratory examination. If polyps are found, they can be removed during the examination.
How do I prepare for my examination?
For your examination to be successful and to allow a clear view of your colon, your bowel must be as empty as possible.
It is important to follow the advice given about bowel preparation.
As part of your preparation you will be given a laxative. Please refer to the Instructions for Bowel Preparation leaflet enclosed.
If your bowel is not empty enough the whole procedure may have to be cancelled and repeated on another day. This is due to the high possibility of the endoscopist missing important signs. (It is believed that those patients who have a bowel cancer diagnosed within two years of a previous colonic examination, have probably had it missed at the time of their original examination - this is called Post Colonoscopy Colorectal Cancer Syndrome PCCCS).If you have diabetes or haemophilia, please phone the Endoscopy Unit your procedure is booked for specific advice.
If you are taking Warfarin, Clopidogrel, Dabigatran, Rivaroxaban, Apixaban, Edoxaban, or other blood thinning medications, please tell us at least one week before your test.
If you have a pacemaker or ICD, please tell us at least one week before your test.
You may continue to take other medications as normal, except iron tablets or stool bulking agents (such as Fybogel, Regulan, Proctofibe), which should be stopped one week before your test.
Please bring a list of any medications you are currently taking. If you have any queries about your medication, please phone the Endoscopy Unit.
It is especially important to remember to bring any asthma inhalers or angina sprays with you.
If you have been diagnosed with sleep apnoea and use a CPAP machine, please bring this with you to your appointment and tell the nurse on arrival.
Do not bring any valuables to the unit. Please note that East Kent Hospitals accepts no responsibility for the loss or damage to personal property, unless the property has been handed in to Trust staff for safe-keeping.
Please remove your nail polish and all types of false nails before coming to hospital for your procedure.
Please bring your dressing gown, slippers, and something to read during your stay. Patients feel a spare set of underwear is useful.
What happens when I arrive at the hospital?
Please report to the reception of the Endoscopy Unit.
A nurse will check your details, blood pressure, and pulse. If you are allergic to anything (medication, plasters, latex), please tell the nurse.
You will be asked to remove any jewellery.
Please tell the nurse if you have a pacemaker, replacement joints, pins, or plates.
Please do not hesitate to ask any questions you may have.
You will have the test you will be having explained to you during your admission. You will then be asked to sign a consent form. Remember you can withdraw your consent for treatment at any time.
You will need to change into a hospital gown, your dressing gown, and slippers.
A nurse will stay with you throughout your examination.
What does the examination involve?
A small needle will be placed into a vein and a sedative and / or painkiller injected before your examination; this will make you feel relaxed but rarely makes you fall asleep. (This needle will be left lightly strapped to your hand / arm until you are recovered from your procedure).
For some patients we offer the use of Entonox for this procedure or no medication at all. Entonox is the pain relief gas that women are given while giving birth. It works by taking in a deep breath using a mouth piece.
A small device for recording your pulse and breathing will be attached to your finger. You will be given oxygen.
A cuff will be placed on your arm to monitor your blood pressure (please tell the nurse if there is a reason why a certain arm cannot be used).
A rectal examination will be performed by the endoscopist before your procedure.
While you are lying comfortably on your left side the endoscopist will gently insert the colonoscope into your back passage (rectum) and pass it around your large colon (bowel).
You may be asked to change positions to lie on your back and / or right side (in some cases on your tummy) during the procedure. This is to help the endoscopist navigate the instrument on difficult bends in your colon.
Air will be passed in to your bowel to expand it so the bowel lining can be seen more clearly. This may give you some discomfort (sometimes mild pain), but it will not last long.
You may need to pass wind during your procedure; this is normal and the endoscopist is used to it. Please do not be embarrassed.
A biopsy (a small sample of the lining of your bowel) may be taken during your examination to be sent to the laboratory for more tests. You cannot feel this. (A video recording and / or photographs may be taken for your records).
Any polyps may be removed during the examination, but you will not feel this either. Polyps are small growths in the lining of the bowel; they are not cancerous but could turn into a cancer in years to come if not removed. Polyps are removed at colonoscopy by cutting them out. This is done by placing a small loop of wire through which a low current of electricity is passed, causing the stem to be burnt through.
Afterwards the colonoscope is removed easily.
What happens after my examination?
You will return to the recovery area to rest.
Once recovered you may eat and drink as normal.
You may still have a little wind; this is natural.
The nurse will tell you the result of the examination before you go home. Any biopsy result will take longer.
After sedation, you may feel a little light headed for the rest of the day and possibly the next day as well.
A letter will be sent to your GP.
Going home
If you have had sedation:
You must have a friend or relative with transport to collect you from the Endoscopy Unit and stay with you at home for at least 24 hours until you are fully recovered.
You must not drive, drink alcohol, operate machinery (including an electric kettle), or sign important documents for 24 hours following the sedative.
You may notice that your bowels do not return to normal for a few days following your procedure.
If you have had Entonox you cannot drive for 30 minutes after the last dose of medication.
If you did not have sedation the above restrictions do not apply to you.
Are there any significant risks?
This test is very safe, but there are some risks linked to this procedure.
A reaction to the sedative. The sedative can affect your breathing making it more slow and shallow.
When a biopsy is taken or a polyp is removed, rarely there may be a little bleeding (the risk is approximately one for every 100 to 200 examinations where a polyp is removed). If this does not stop within 24 hours or is excessive, please contact the Endoscopy Unit or Emergency Department.
Perforation, which is a little tear in the wall of the colon, this is also rare (risk is approximately one for every 1000 examinations). This would need a short stay in hospital and treatment with antibiotics. Very occasionally it may need surgical repair.
A feeling of bloating due to the air we need to insert so we can clearly see where we are. Please talk to your endoscopist before your examination if you have any worries about these risks.
Are there alternatives to a colonoscopy?
Yes, there is a CT pneumocolon and a barium enema. They both need the same kind of bowel preparation as a colonoscopy but they do not allow the removal of polyps or the taking of biopsies. This means that you would probably need a colonoscopy anyway.
Any further questions?
Please phone the Endoscopy Unit. The units are open Monday to Sunday 8am to 6pm.
Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783058Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234370William Harvey Hospital, Ashford
Telephone: 01233 616274
If you have any questions between 6pm and 8am Monday to Sunday then contact the Emergency Department on:
Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235030William Harvey Hospital, Ashford
Telephone: 01233 616207
Our units are regularly inspected and audited. Please ask if you want any information about our performance standards. You can also visit the Care Opinion web site.
A short film outlining what patients can expect when coming to hospital for an endoscopy is available on the East Kent Hospitals' YouTube channel.