Carpal tunnel syndrome
Information for patients from the Orthopaedic Hand Service
You have been diagnosed with carpal tunnel syndrome (CTS). This leaflet will explain:
what carpal tunnel syndrome is,
what the symptoms and causes are,
how a diagnosis is made,
and what the treatment options are.
If you have any questions after reading this leaflet, please speak to your relevant healthcare professional.
What is carpal tunnel syndrome?
CTS is a condition where pressure is placed on the nerves to the hand (known as the median nerve). This pressure causes feelings of:
uncomfortable pins and needles in the hand, and
in more severe cases, numbness and weakness in the hand.
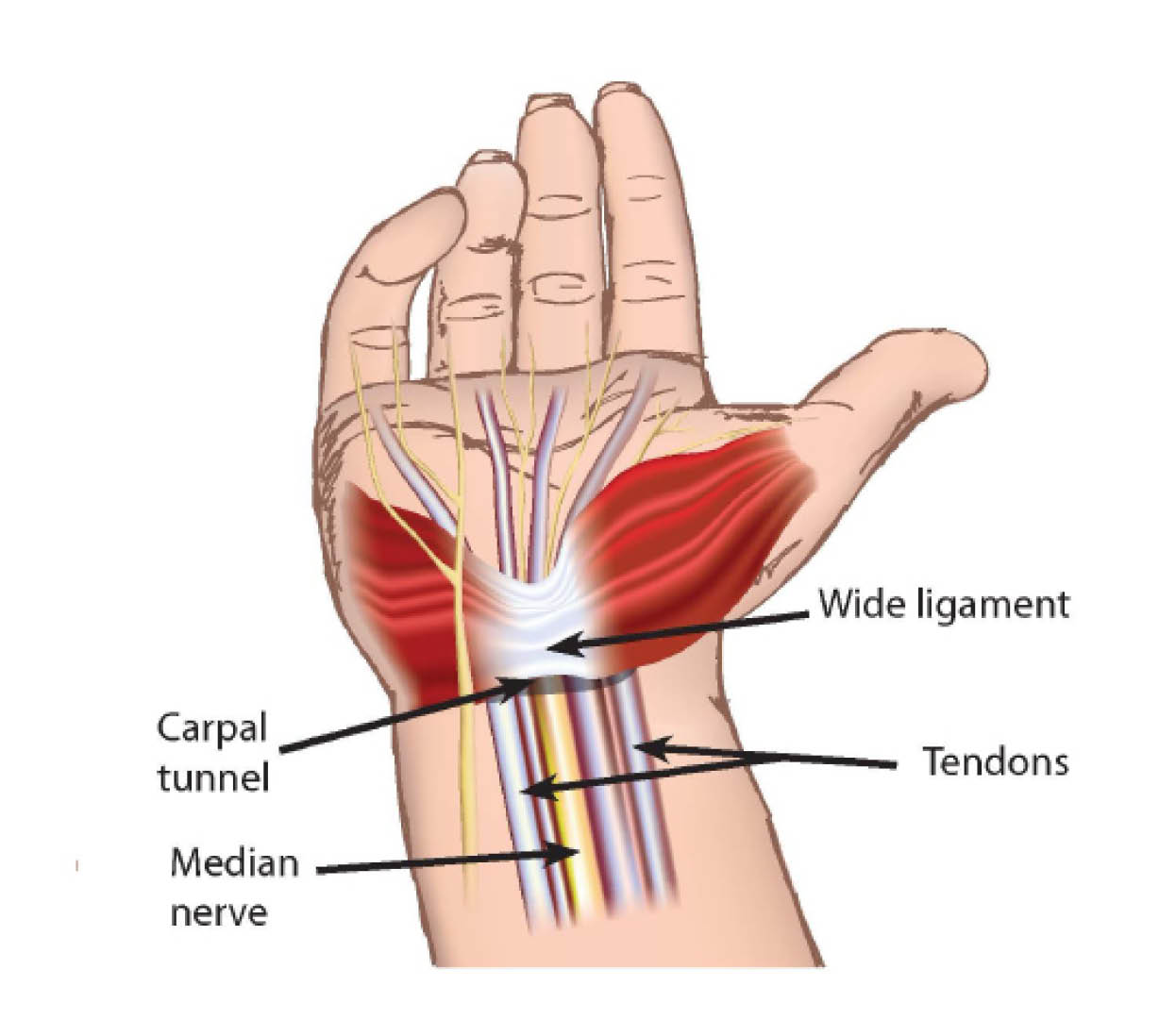
The median nerve runs from the neck, down the arm, and through a tunnel at the wrist (the carpal tunnel) and into the hand. The carpal tunnel is formed by the wrist bones in a ‘u’ shape and a wide ligament that sits across the top to the roof of the tunnel.
What causes CTS?
CTS can happen as a result of increased pressure in the carpal tunnel, which compresses the nerve in this space. In most cases CTS can happen without any identifiable cause. However there are some factors that can be linked to it, including:
diabetes
pregnancy
under active thyroid conditions
wrist fractures, and
various forms of arthritis.
Patients with CTS often say the symptoms get worse when they carry out heavy activities.
In the early stages of the condition, many people with CTS mainly have these symptoms at night. As the condition progresses, symptoms develop during the day as well and they start to happen more often.
How is CTS diagnosed?
Diagnosis of CTS is made from a combination of assessments, including the following.
Taking a your medical history, so we can see the pattern of your symptoms.
Clinical tests carried out by your GP, consultant, or therapist.
Carrying out nerve conduction studies (NCS). A NCS is where small metal wires called electrodes are placed on your skin. These electrodes release tiny electric shocks to stimulate your nerves. This can help your doctor or therapist see how bad your nerve compression is.
How can CTS be treated?
Different treatment options are available. The options available to you will depend on:
how bad your symptoms are, and
the results of the nerve conduction studies (see above).
Splint provision
You may be given a splint. The splint is usually only to wear at night, to hold your wrist in a neutral position. This allows for maximum space in the tunnel, reducing the pressure on your median nerve.
Splints are a very safe treatment. Around one in three patients find these helpful, with no other treatment needed.
Injections
A local cortisone steroid injection can be administered into the carpal tunnel, to give you some relief from your symptoms. There are some very rare complications with local injections, such as infection or nerve damage from the injection itself.
Around four in five patients will benefit from a steroid injection. In some cases the symptoms will re-occur.
Surgery
Surgery may be an option, if your CTS is quite severe and other treatments have not helped. Surgery will involve a small cut across the carpal ligament at the base of your palm. This will make more room for the nerve, easing the pressure within the tunnel. For most patients this surgery is done under local anaesthetic as a day case (you can go home on the same day as your surgery).
Most patients get very good and permanent relief from their symptoms following surgery. However, even with surgery, the nerve damage can be irreversible for some patients diagnosed with very severe CTS. Your surgeon will discuss this with you before your operation.
What happens if I choose not to have the operation?
The symptoms of pain and numbness may stay the same, increase, or even become permanent.
The muscles in your hand may become weak, causing problems with some activities.
A small number of patients may improve even without any treatment.
What are the risks with surgery?
Serious complications are uncommon. However a small number of patients can have complications, some of which resolve with time. These include:
scar tenderness and hand weakness
aching and pain especially on gripping; and
wound infections, which can happen in around one in every 100 cases.
A very small number of patients will develop a serious reaction to the surgery and develop Complex Regional Pain Syndrome (CRPS). This is a rare condition but can cause severe pain, swelling, and stiffness in the hand. It can take several months to improve or may even continue.
CRPS can often start gradually. It may not be noticeable for 4 to 6 weeks. If you have ongoing persistent pain and swelling throughout your whole hand after 6 weeks, please contact the consultant you were under for the surgery for a review, or visit your GP.
What happens before my operation?
The Pre-assessment Clinic will contact you and a nurse will discuss your operation with you. Please feel free to ask questions and raise any concerns that you may have about your operation.
You may need to have some routine tests before your operation, such as a blood test.
The nurse will ask you some questions about your general health.
Please tell the nurse what medication you are currently taking. The nurse will need to know their names and the doses. This includes non-prescription medicines, such as herbal / complimentary medicines.
Compared to non-smokers, smokers are more likely to have complications in tissue healing and infections after injuries or surgery. For free friendly support and medication to help you stop smoking, contact One You Kent.
One You Kent
Telephone: 0300 123 1220
Email
On the day of your surgery, please remove all rings from your fingers before coming to hospital.
Will I have to stay in hospital?
No, the procedure is carried out as day surgery. You will need to be in hospital for 3 to 4 hours.
What will happen when I arrive at hospital?
Please refer to your appointment letter for where to go when you arrive at the hospital. You will be greeted by a member of the ward staff and advice will be given regarding your care.
How will I feel after my operation?
You may be in a little discomfort after your surgery. This is quite normal, but it is not common to be in large amounts of pain. You can take simple painkillers such as paracetamol if you feel it necessary and you are able to take this kind of medication.
What should I do if I feel pain at home?
Contact your GP for advice if:
your pain gets much worse after you are sent home, and
if you start to feel unwell in yourself.
If this is outside GP hours, go to your nearest Emergency Department or Urgent Treatment Centre. They may need to check your wound and can then advise on what to do next.
When can I drive / go back to work?
Do not drive yourself home after your surgery. You will need to arrange for someone to drive you home. Do not return to driving until your hand feels comfortable when using it for general daily activities. This is often around 1 to 2 weeks after your surgery.
When you can return to work depends on the work you do. For example:
if your job involves light duties, you can return after 1 to 2 weeks, but
if your job involves more demanding work, you may not be able to return for around 3 to 6 weeks.
When can I return to my normal activities?
You should return to normal everyday activities as your pain allows, often around 2 to 3 weeks after your surgery.
Will I need a follow-up appointment?
Most patients are placed on a Patient Initiated Follow-Up (PIFU) after their surgery. For more information, please read the Patient Initiated Follow-Up (PIFU) (Orthopaedic Hand Service) leaflet.
The details of your appointment or who to contact in the event of a problem will be included in your post-operative discharge summary.
When will my dressing and stitches be removed?
You can remove the bulky dressing on your hand 48 to 72 hours after your surgery.
Leave the small dressing over your wound. It is very important to keep this clean and dry.
Go to your GP or Urgent Treatment Centre to have your wound checked, if:
you have any excessive pain, swelling, or tenderness around your wound, as you may have an infection.
Do not do any excessive weight bearing activities for the first 4 weeks following your surgery. Weight bearing activities include pushing up from a chair or heavy gripping.
Any dissolvable stitches will start to fall out after 10 to 14 days. Other stitches will need to be removed by your GP, practice nurse, or consultant. You will be advised of this at the time of your surgery.
How do I care for my scar?
The length of the scar will vary between patients. The number of stitches will also vary. Your surgeon will aim to make the scar look as good as possible.
Your scar may become sensitive to touch while it heals. To help with this, it is very important to massage your scar with a small amount of water-based hand cream for up to 8 weeks after surgery. This will help to soften the scar tissue and reduce its sensitivity. For more information, please read the Trust's Scar massage leaflet.
Rehabilitation after surgery
For the first 48 hours after your surgery.
Keep your hand elevated (raised) to reduce the swelling and stop stiffness in your fingers.
Do not walk with your hand dangling down by your side.
Exercises
It is important to start these exercises on the day of your surgery.
They may be uncomfortable but should not be painful.
-
 1. Make a full fist with your hand.
1. Make a full fist with your hand. -
 2. Straighten your fingers out again.
2. Straighten your fingers out again. -
 3. Touch your thumb to the tip of all your fingers
3. Touch your thumb to the tip of all your fingers -
 4. Spread your fingers out as far as possible and back again.
4. Spread your fingers out as far as possible and back again.
5.Reach as high into the air as you can.
Further information
If you have any further questions, please ask your consultant or therapist.
For more information, please go to the East Kent Hospitals' Carpal-Tunnet.net web site.