Cardiac intervention
Information for patients from the East Kent Cardiac Catheter Suites (EKCCS)
You are coming into hospital for an angioplasty and stent procedure (PCI). This leaflet will explain:
why you need an angioplasty
what happens during the procedure, and
what happens afterwards.
Further information is available from your local heart support group. Also the British Heart Foundation has a series of booklets, which are available from your cardiac rehabilitation nurse or in the Cardiac Catheter Suite.
Why do I need an angioplasty?
Your heart muscle is supplied with oxygen by blood being pumped into your coronary arteries. If these arteries narrow, your heart becomes starved of oxygen. This causes pain in your chest, called angina.
Angina usually occurs when the heart muscles’ need for oxygen increases. This can happen when you are exercising or during stressful situations. However, for some people, angina occurs even when they are resting. This suggests that their arteries may be more severely affected.
Many people who have angina are treated with tablets and / or GTN spray. However, some people continue to have symptoms despite taking several different types of drugs. They may be unable to carry out normal daily activities because of their chest pain.
Angioplasty is one option for treating this condition.
What is an angioplasty?
During the procedure your narrowed arteries are opened, so that blood can flow more easily to your heart muscle.
The procedure is called a percutaneous coronary intervention (PCI). It is performed in a cardiac catheter lab, using x-ray screening.
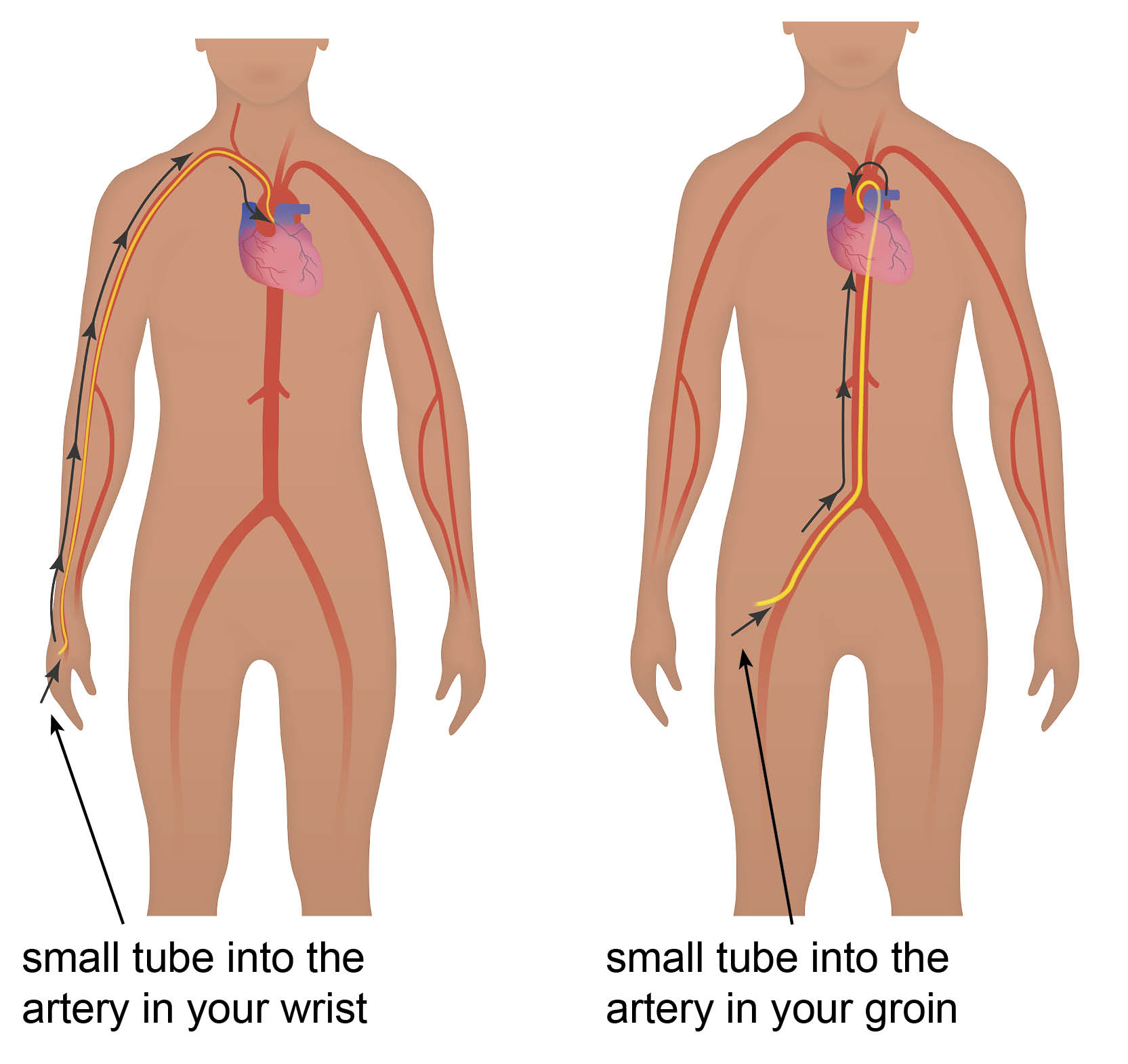
A fine plastic tube (called a sheath) is passed into the artery via a small puncture hole in the groin or a small cut in the wrist. This will be done under local anaesthetic (the area is numbed but you are awake).
The wrist is the most common site used for this procedure.
Another fine tube (called a guiding catheter) is passed through this sheath. The guiding catheter is passed along to the heart and positioned at the opening of the coronary artery.
A fine guide wire is passed down the artery through the area of narrowing.
A small balloon is inflated. This will compress the fatty plaques up against the wall of the coronary artery, widening your artery.
The balloon may need to be inflated several times. Your doctor may also need to use several catheters and balloons to widen your narrowed artery.
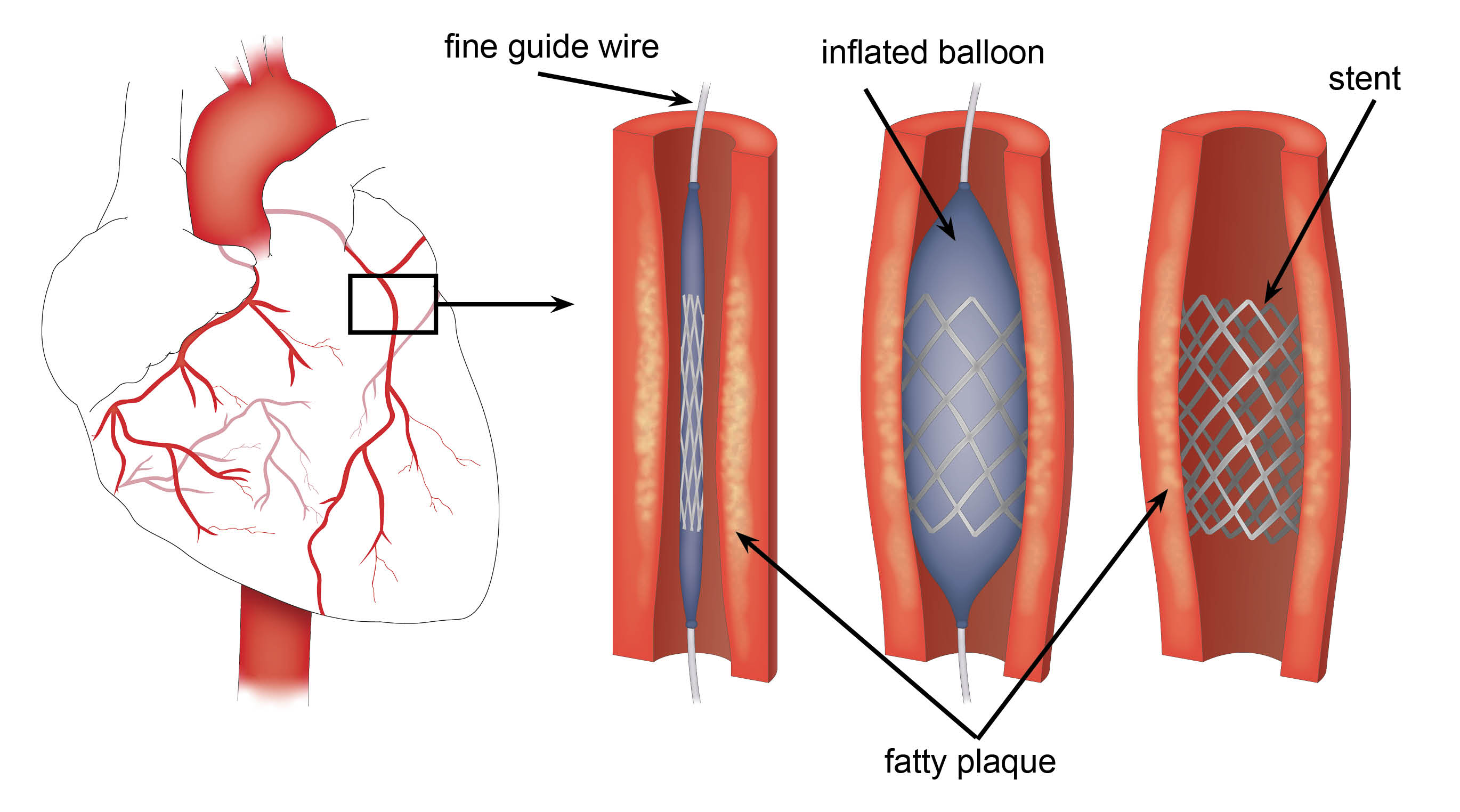
A coronary stent may be used during the angioplasty to support the artery wall.
Once your doctor is happy with the result, the catheter and balloons are removed. The sheath in your wrist or groin will be left in, until your doctor is satisfied that it can be removed.
What is a coronary stent?
This is a small metal mesh tube which is inserted into an artery, at the site of a narrowing. It forms an internal scaffolding, or support, to the artery. The stent is mounted on a balloon and positioned by inflating the balloon. This expands the stent and pushes it up the artery wall. When the balloon is deflated the stent remains in place.
In the four weeks following insertion of the stent, a thin film of cells will grow over the framework. This will line the wall of the artery like a skin. Until this has occurred, there is a risk of blood sticking to the stent, forming a clot. To reduce the chances of this happening, you will be prescribed aspirin and clopidogrel.
Some stents also contain a drug to reduce the number of times clot formation happens.
What should I do before I arrive for my procedure?
Take all your usual medicines and bring them with you to hospital. There may be some that your doctor will not want you to take, but you will be told of these in your appointment letter.
If you are diabetic, please contact the Cardiac Catheter Suite before your appointment. The contact details are at the end of this leaflet.
Remove any nail varnish.
Arrange for someone to drop you off and pick you up after your procedure. If there is no one available, please let us know as soon as possible.
Unfortunately you cannot bring anyone onto the unit with you.
Bring an overnight bag and toiletries. You will change into a hospital gown for your procedure, so please also bring slippers and a dressing gown.
Wear comfortable underwear without tight elastic.
Leave any valuables at home.
Eat and drink as normal.
What will happen when I arrive on the ward?
Soon after you arrive, a nurse will get some details from you and take a blood sample. A small intravenous tube called a cannula is placed in your arm or hand. This is in case you need any medication during your procedure.
What happens during my procedure?
During your procedure the x-ray equipment will, at times, be brought very close to you. Sometimes it may be necessary to rest your arms above your head and turn your head to the left and right.
Whilst the balloon is being inflated you may feel discomfort in your chest (angina). If this happens, please tell the doctor and nurses straight away. This is due to the balloon causing a temporary blockage to the blood flow through the artery. This is normal.
How long does the procedure take?
The procedure can take 30 minutes to 3 hours. It will depend on the complexity and number of narrowings in your coronary arteries.
What happens when I return to the ward?
When you return to the ward area you will placed on an ECG monitor, which will remain on for several hours.
You will be able to drink as soon as you are back in the ward area. You can eat again once you can sit up.
The nurses will check your puncture site regularly.
After your procedure, the sheath is usually removed from your wrist. A pressure band is left in place for several hours.
If we go via your groin, you will need to lay flat to prevent any damage to the artery in your leg. When appropriate, the nurse will sit you up. You can get out of bed later that day.
Methods for preventing bleeding on removal of the sheath:
The doctor or nurse may press on the puncture site for 10 minutes or until the bleeding has stopped. You may then need to lay flat for a few hours, unless you had your procedure performed in your wrist.
Another method is the femostop. This puts firm pressure on the puncture site for a period of time. Some patients may find this uncomfortable.
Or we will use a product called an angioseal. This is a collagen plug that blocks the puncture hole in the artery.
Your doctor will decide which method is best for you. Please discuss this and any other questions you may have, when you sign your consent form before your procedure.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
How do I look after my wound?
Leave the puncture site exposed, to help it to heal.
Some bruising or discolouration may occur at the site. This is not serious and may get worse before it gets better. If the sheath was in your groin, bruising may extend down your leg. It will fade over the next few weeks, as you start to walk around. Take paracetamol for any minor discomfort.
If you notice any signs of infection at the puncture site, please contact your GP. This includes heat, oozing, redness, swelling, or increased soreness.
You can shower when you get home, but avoid rubbing your wound site for a week.
Do not put creams or soap directly onto your wound during this time.
When can I return home?
These procedures are usually done as day cases. If there were any complications or your discharge is delayed, you may need to stay in hospital overnight.
You must not drive yourself home. You must not drive for a week after your procedure.
Remember that everyone is different and you will recover at your own rate.
Will I need a follow-up appointment?
Yes. You will have a follow-up appointment with your local cardiologist. The hospital will send the details of this appointment to your home address. It is helpful to write down any questions which you may have before this appointment.
A cardiac rehabilitation nurse may also follow you up at home.
Will I go home with medication?
If needed, we will give you a supply of medicines to take home. Your nurse will explain them to you.
If you had a stent inserted, we may prescribe you a tablet called clopidogrel (Plavix). This medication will help prevent blockages building up in your new stent. Please check with your nurse to find out how long you need to take this medication for. If you were already taking clopidogrel you may need to continue taking it for the long-term.
When can I resume my normal activities?
You may resume light household chores the day after you are discharged from hospital.
Avoid strenuous activities, such as vacuuming or moving furniture, for at least a week. Continue to avoid sudden exertion.
The DVLA recommend that you do not drive for one week after an angioplasty. You do not need to tell the DVLA that you have had the procedure unless you hold a PSV or HGV licence. However, you may need to tell your vehicle insurance company.
In the long-term it is safe to fly. You will be able to pass through airport security gates with no problem. Many airlines prefer you to wait two to three weeks after your procedure. It is best to check with your airline.
If your work is light, for example a desk job, you may return to work as early as two days after your discharge from hospital, but only if you have recovered sufficiently. If you do manual work you should not return for one week.
If you have had your procedure following a heart attack, speak to your doctor or cardiac rehabilitation nurse about when to return to work.
Activity and exercise are good for your heart. If you usually exercise regularly, you should build up to your normal level gradually in the first two weeks following your angioplasty. If you are not normally active then now may be a good time to start. Your cardiac rehabilitation programme will include exercise.
You and your partner may be worried about having sex again. The physical effort used when having sex is no more than you would use in regular physical activity. It is normally safe to have sex again as soon as you feel ready. It is not uncommon for cardiac patients to experience sexual problems. If you have any concerns, please speak to your doctor or nurse.
Will I experience chest pain after discharge from hospital?
Most people never get chest pain again.
Some people can have artery spasms for up to two weeks after a stent insertion. This can be like previous angina pain. Your doctor or nurse may give you tablets for this when you leave hospital.
Some people may get further angina, which may be harder to control. If this is the case, make an early appointment with your GP.
If you have sudden, severe chest pain lasting longer than 15 minutes, which is not helped by GTN spray, tablets, or rest, you should telephone 999 immediately for an ambulance. Do not drive. You can use up to three doses of GTN five minutes apart to relieve angina. Do not exceed this dose. Tell the ambulance crew that you have had a stent inserted at the William Harvey Hospital, and that you need immediate transport to hospital.
What are the benefits of the procedure?
This procedure is simpler and the recovery a lot shorter, than if you have a coronary artery bypass surgery (CABG). A CABG involves opening up your chest wall.
The aim is to improve your quality of life by removing or reducing the number of angina attacks.
Are there risks to the procedure?
Most patients have no problems with this procedure, but we need to outline some possible risks. Your doctor will discuss these with you before you sign your consent form.
A small clot in your artery may dislodge and cause a stroke.
You may have an allergic reaction to the dye injection (contrast). Symptoms include a rash, itching, or inflammation.
You may have damage to your heart artery. This will need emergency bypass grafting, and mean transferring you to St Thomas’ or King’s College Hospital, London. More information on this is below.
Damage to the artery in your groin can cause swelling, known as a false aneurysm.
Your heart artery may block and your doctor is unable to open it. This could bring on a heart attack.
Though rare, it is important for you and your relatives to know that death is possible.
The risks of needing emergency cardiac surgery as a result of cardiac angioplasty (PCI) are approximately one in 500. Whilst EKCCS provides an out-of-hours on-call service, we are not able to provide cardiac surgery within this Trust. In the unlikely event of you needing emergency cardiac surgery, we will transfer you to St Thomas’ or King’s College Hospital in London. They provide us with a comprehensive surgical back up service.
EKCCS is assessed and approved by the British Cardiac Interventional Society (BCIS) to perform cardiac angioplasty. If you feel, for any reason, that you do not wish to have your PCI at EKCCS, this would in no way compromise your treatment or medical care. The choice remains entirely with you.
Please remember that the majority of procedures are performed without any major complications. But it is important that you realise that this is not a risk free procedure.
Further information
If you have any further questions, please contact either:
one our cardiac nurse specialists,
your doctor when you sign your consent form, or
the Cardiac Catheter Suite, William Harvey Hospital Ashford on 01233 616830.