Bronchoscopy
Information for patients from the Trust's Endoscopy Units
This leaflet is for patients who are having a bronchoscopy. It explains what is involved, and any significant risks there may be.
As a University Hospital, students and trainees supervised by qualified staff may be involved in your care. If you do not wish students to be present, please tell the bronchoscopist or nurse-in-charge.
The time on your appointment letter is your booking in time. Please tell anyone that comes with you to your appointment that this is not your procedure time. If you do not come to your appointment without telling the Endoscopy Unit in advance, you may be removed from the waiting list.
The test itself takes around 30 minutes. It may take longer if we need to carry out additional procedures. If there is an emergency or very complex cases, these take priority and may delay your procedure.
What is a bronchoscopy?
A bronchoscopy is where a bronchoscopist looks into your main airways. These are the central, larger tubes that carry air into your lungs.
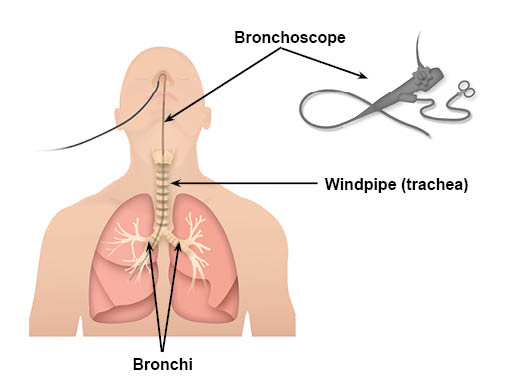
A fibre-optic bronchoscope is used to look into your airways. This is a thin, flexible telescope (shown in the diagram). It is about as thick as a pencil.
The bronchoscope is passed through your nose or mouth, down the back of your throat, into your windpipe (trachea), and down into your bronchi. The fibre-optics allow light to shine round bends in the bronchoscope. This allows the bronchoscopist to see your airways on a screen.
Why am I having a bronchoscopy?
Common reasons for having a bronchoscopy are:
To try and find the cause of a ‘shadow’ or 'opacity' found on a chest x-ray / CT scan.
To investigate a persistent cough.
To find a cause for coughing-up blood, a suspected infection, or lung cancer.
The bronchoscopist can look at any area of concern in the main airways. They can also take a biopsy (small sample) to look at under the microscope.
You may have other tests, but a bronchoscopy is one of the main diagnostic tests for diagnosis of respiratory complaints.
What do I do before coming into hospital?
On the day of your examination, do not eat or drink for four hours before your appointment.
You should take your normal medication, with a sip of clear water, except any medication that thins your blood or medication for diabetes. You should bring these into hospital with you. You will be told before your bronchoscopy when you can start taking your blood-thinning medication again.
Please feel free to bring a book or something to occupy you, as well as a dressing gown and slippers.
Please arrange for someone to drop you off and pick you up from the Endoscopy Unit. Someone should also stay with you overnight, as the sedation may not have fully worn off.
Please contact the Endoscopy Unit as soon as possible if:
you have diabetes
might be pregnant
are taking blood-thinning medication, or
have a pacemaker.
We also need to know if you have had a heart attack, clots in your lungs, or stroke within six weeks of your appointment.
If you have any questions, please contact the Endoscopy Unit.
It is important to bring any angina sprays or asthma inhalers with you.
Please do not bring valuables into hospital.
What will happen when arrive at hospital?
Please report to the Endoscopy Unit reception.
An endoscopy nurse will check your details, blood pressure, and pulse. If you are taking any medication or you are allergic to anything (medications, plasters, latex), please tell the nurse.
You will be asked to remove any jewellery, glasses, contact lenses, tongue studs, and false teeth before your examination.
The bronchoscopist will explain the procedure. They will outline the risks and the benefits of the procedure. You will then sign a consent form.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time
You will need to change into a hospital gown.
A small needle will be used to place a plastic tube into a vein in your arm, to give you medication. This tube is called a cannula.
A nurse will stay with you throughout your examination.
What does the examination involve?
The bronchoscopist will numb the inside of your nose and the back of your throat, using a local anaesthetic spray. This may taste a bit unpleasant and cause you to cough.
You will have a sedative to help you to relax. This is given through your cannula. The sedative can make you drowsy. It is not a general anaesthetic and does not ‘put you to sleep’. It should be enough to relieve any anxiety or distress. Sometimes it can also make you forget the procedure itself.
Your essential observations will be monitored throughout your bronchoscopy, to ensure your safety. Your arm will be connected to a monitor to check your blood pressure, and a pulse oximeter will be put on a finger. This does not hurt. The oximeter checks your pulse and blood oxygen content, telling us if you need extra oxygen during your bronchoscopy. You will have a soft plastic tube placed just inside your nose to give you oxygen.
The bronchoscopist will insert the tip of the bronchoscope into a nostril. They will guide it round the back of your throat into your trachea (windpipe). It is sometimes passed via the mouth rather than your the nose, if you have narrow nasal passages. The bronchoscope transmits pictures through a camera attachment on to a TV monitor, for the bronchoscopist to look at. The bronchoscopist looks at the images and checks the lining of the trachea and main bronchi (the main airways). The bronchoscope may make you cough. It does not hurt, and should not affect your breathing.
The bronchoscopist may take samples (biopsies or brushings) of parts of the inside lining of your airways or the peripheral substance of the lung. This is painless. The biopsy samples are sent to the laboratory for testing.
Sometimes a small amount of sterile fluid is passed into the lung and sucked back out again. This is called bronchial washing. This fluid can also be sent to the laboratory to look for organisms or abnormal cells.
The bronchoscope is then gently removed.
How long will it take?
The bronchoscopy itself usually takes about 30 minutes. However, you should allow at least four hours for your appointment. This allows you time to prepare and gives the sedative time to work. It also includes the bronchoscopy itself, and the time needed to recover.
What will happen after my procedure?
You will return to the recovery area to rest.
Your pulse and blood pressure will be monitored until you have recovered.
Your nose and throat may be sore after the local anaesthetic wears off, but this will pass.
You will feel sleepy for a while. This will improve over the next few hours, and you will be fully recovered within 24 hours.
You may cough-up some blood-stained sputum or have a small nose bleed, but this should not worry you.
You will be kept nil-by-mouth until your nurse says it is safe to eat and drink. You will be offered a drink and something to eat, usually about two hours after your procedure.
You may be seen by the bronchoscopist before your discharge home.
If you have had samples taken, the results will take approximately seven working days to come back.
What should I do when I go home?
You must have a friend or relative with transport collect you from the unit. They must stay with you for 24 hours, while you rest until you are fully recovered.
You must not drive, drink alcohol or use any sleeping aids, operate machinery (including an electric kettle), make important decisions, or sign important documents for 24 hours following your procedure.
You may have a cough for a few days after your procedure. This should clear on its own, and should not be of concern.
When can I return to work?
The sedation stays in your system for approximately 24 hours. You should not operate machinery or drive during this time. You may feel well the day after your examination, but the sedation may affect your ability to work. We advise you to take the day after your examination off work, to allow you to rest and recover.
Are there any risks?
Common side effects include:
Cough
Sore throat
Hoarse voice
Under-sedation (where you are able to remember the procedure)
Some blood streaking / clumping in the sputum.
Serious or life-threatening complications
These are rare, affecting less than one in 5,000 patients. They include the following:
Bleeding.
Fever or infection, introduced through your upper airway during the bronchoscopy.
Collapse of the lung (pneumothorax) or escape of air into the centre of the chest (pneumo-mediastinum). These usually resolve on their own in time. Sometimes they may need observation in hospital or insertion of a drain into the chest under local anaesthetic.
Irregularities of the heart (arrhythmias).
Sedation may cause suppression of breathing. If this happens you may need temporary support with breathing (ventilation).
Death is an extremely rare complication of bronchoscopy.
You will have the chance to ask any questions and discuss these risks before your bronchoscopy.
What do I do if I feel unwell at home?
If you you have any the symptoms listed below within 24 hours of having your procedure, contact the Endoscopy Unit or go to an Emergency Department. Tell them that you have had a bronchoscopy. Take a copy of your report with you.
Symptoms
You feel unwell
You feel hot and cold
Your heart is racing
You have any chest pain
You are coughing-up a lot of blood.
If there is anything you are unsure about, please speak to your nurse before you leave the hospital.
Any further questions?
Please phone the Endoscopy Unit. The units are open Monday to Sunday 8am to 6pm.
Kent and Canterbury Hospital, Canterbury
Telephone: 01227 783058Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 234370William Harvey Hospital, Ashford
Telephone: 01233 616274
If you have any questions between 6pm and 8am Monday to Sunday then contact the Emergency Department on:
Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235030William Harvey Hospital, Ashford
Telephone: 01233 616207
A short film outlining what patients can expect when coming to hospital for an endoscopy is available on the East Kent Hospitals web site.
Our units are regularly inspected and audited; please ask if you want any information about our performance standards. You can also visit the Care Opinion web site.