Breech presentation after 36 weeks of pregnancy
Information for women, birthing people and their families
What is a breech presentation?
During pregnancy babies are very active, twisting and turning, and changing position often. Breech presentation is common in early pregnancy. By 37 weeks most babies have usually settled into the head down position. If your baby is lying bottom, feet, or knees first in your uterus (womb) instead of head down, you will be told that your baby is breech.
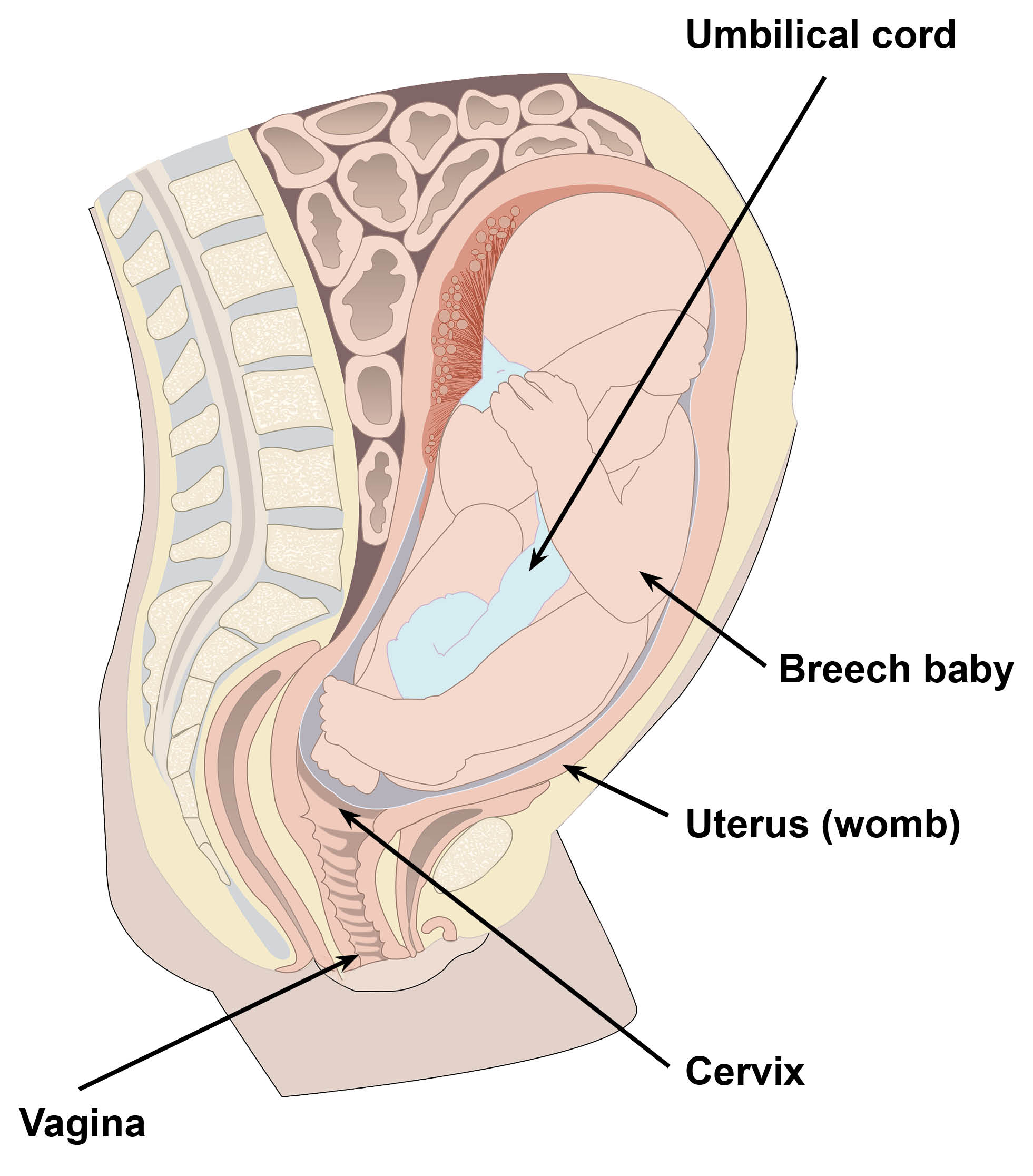
In 3 to 4 in every 100 pregnancies the baby remains in the breech position after 36 weeks. It is unusual for the baby to turn head down after this time.
If your baby is breech after 37 weeks, there are three options that should be considered.
External cephalic version (ECV) is where a skilled doctor turns your baby.
A vaginal breech birth.
A planned caesarean birth.
Decision-making needs balancing your wishes and expectations against the possible risks to you and your baby.
Why is my baby breech?
It may just be a matter of chance that your baby has not turned into the head down position. There are some reasons that make it more difficult for your baby to turn during pregnancy. These include if:
your placenta is in a low-lying position (in the bottom part of your womb)
you have placenta previa (when part of your placenta covers part, or all of the opening of your womb)
you have too much, or too little water (amniotic fluid) around your baby
you are having more than one baby; or
you have an issue with your pelvis or uterus, for example, fibroids.
What are my options if my baby is still breech at 36 weeks?
If your baby is still breech at 36 weeks of pregnancy, your doctor or midwife will start discussing the following options with you.
Trying to turn your baby in the womb into the head down position by external cephalic version (ECV)
planned vaginal breech birth; or
planned caesarean birth.
You do not have to make your decision at this time. There is still a small chance your baby may turn into the head down position after 37 weeks on its own. You can ask to speak with our consultant midwife if you have questions.
What is external cephalic version (ECV)?
An ECV is when a doctor tries to turn your baby from a bottom down into the head down position.
This involves applying gentle but firm pressure on your tummy.
You will have an injection to relax your womb.
The doctor will feel the baby’s position and carefully push the baby around into a head down position.
An ECV can be uncomfortable because of the pressure on your tummy, but it should not be painful. The procedure will only last for a few minutes. It will be carried out on the labour ward, and you will normally be able to go home on the same day.
When will I have an ECV?
An ECV is usually performed after 36 weeks of pregnancy. However, it can be performed up until the start of labour.
Is an ECV safe for me and my baby?
An ECV is generally safe. Overall, there does not appear to be an increased risk to your baby from having an ECV. When you do go into labour, your chances of needing an emergency caesarean birth, or forceps or kiwi / ventouse (suction cup) birth are slightly higher than if your baby had always been in a head down position.
Immediately after the ECV, there is a 1 in 200 chance you will need an emergency caesarean birth. This could be due to bleeding from the placenta and / or changes in your baby’s heartbeat.
We do not attempt ECV if:
you are pregnant with more than one baby
you are to be delivered by caesarean birth
you have had vaginal bleeding after 28 weeks
your waters have broken
there are any concerns about your baby’s wellbeing on ultrasound scan; or
your baby’s heart rate monitoring (CTG) is abnormal.
You can still safely have an ECV if you have already had one caesarean birth. Depending on your individual situation an ECV may be done right up until you give birth.
Will it succeed?
ECV is successful for about half of all women and birthing people (1 in 2 pregnancies). There is a small chance (5 in 100 pregnancies), that your baby will turn back to breech after a successful ECV. It is more likely to work if you have had a vaginal birth before. Your doctor will give you their opinion of the chances of your baby turning based on your individual circumstances. If your baby does not turn, your doctor will discuss your options for birth.
If your baby is successfully turned head down, you are more likely to have a vaginal birth. A successful ECV will reduce your chances of needing a caesarean birth and its associated risks.
Is there anything else I can do to help my baby turn?
There is some evidence that the use of acupuncture or moxibustion (burning a Chinese herb called mugwort) may help to turn your baby head down. These options are not offered by our Trust. If you decide to use these you should only do so when consulting a registered healthcare practitioner for advice and treatment.
Some healthcare professionals advise the use of optimal fetal positioning. This involves you getting into certain positions to increase the space in your pelvis. In theory this will give the baby space to move around. You can discuss this further with the consultant midwife. There is no scientific evidence to support that lying or sitting in a particular position can help your baby turn.
You may read about other therapies such as complementary therapies or chiropractic techniques. These are not offered at our Trust, and you are advised to take specialist advice before using any of these methods.
What will happen during an ECV?
You will be seen on the labour ward at the William Harvey Hospital (Ashford) or Queen Elizabeth Queen Mother (QEQM) Hospital (Margate).
When you arrive, your midwife will take your observations, and monitor your baby’s heart rate (CTG). They will ensure both you and your baby’s wellbeing.
You will have an injection to relax your womb. This will be given in your upper arm, thigh, or your bottom. This injection is called terbutaline, and it is safe for you and your baby. Relaxing the muscle of your womb (uterus) improves the chances of turning your baby. It may make you feel flushed and you may become aware of your heart beating a little faster than usual, but this will only last a short time.
A doctor will perform a bedside ultrasound scan. This will confirm your baby is breech, and the position of your baby.
Approximately 20 minutes after the injection of terbutaline the doctor will try to turn your baby. To do this, the doctor places their hands on your tummy. They then feel for the baby’s position and carefully push the baby around into a head down position.
After the ECV, the ultrasound scan will be repeated to check if your baby has turned.
Your baby’s heart rate will also be monitored for approximately 20 minutes to ensure your baby’s wellbeing.
If the ECV is unsuccessful on the first attempt, the doctor may discuss the option to try again on another day. This is only if you would like them to. Your doctor will tell you if they feel it is unsuitable.
After your ECV, if you have any of the following, contact Maternity Triage. Their number is at the bottom of this leaflet.
Bleeding
Abdominal pain
Contractions
Reduced fetal (baby) movements.
What should I expect afterwards?
You might feel slight discomfort after the procedure. If it is successful, however, you may feel more comfortable as your baby’s head will no longer be under your rib cage.
In the unlikely event of any vaginal bleeding, more severe pain, or a reduction in your baby’s movements, contact Maternity Triage. Their telephone number is at the end of this leaflet.
What if I am Rhesus negative?
If your blood type is Rhesus negative, and your baby is predicted to be rhesus positive, or you did not have cffDNA testing you should have already been offered an anti-D injection during your pregnancy and be aware of why this is needed. More information is available in The Rhesus factor and anti-D leaflet.
During the ECV there is a possibility that some of your baby’s blood cells could mix with yours. For this reason, it is recommended that you have an extra anti-D injection following the ECV, whether the ECV was successful or not.
What are my options for birth if my baby remains breech or I decide not to have an ECV?
If an ECV is unsuccessful or not performed, you will need to discuss your birth options with your doctor or midwife. Depending on your situation, your choices are:
a planned vaginal breech birth; or
a planned caesarean birth.
There are benefits and risks associated with both a vaginal breech birth and a caesarean birth. These should be discussed with you so that you can choose what is best for you and your baby. Both options are discussed below.
Planned vaginal breech birth
Before choosing a vaginal breech birth, it is advised that you and your baby are assessed by your doctor. We can also offer a referral to the consultant midwife to help with birth planning. Ask your midwife or doctor to refer you if you would like this.
The doctor and consultant midwife will discuss your options with you. This includes your and your baby’s suitability for a breech birth. They will discuss with you, your and your baby’s individual risks.
If you decide on a vaginal breech birth you should plan to have a hospital birth. This is so you can have an emergency caesarean birth, if needed. Four in 10 planned vaginal breech deliveries need an emergency caesarean birth (Royal College of Obstetricians and Gynaecologists, RCOG). All maternity staff are trained and updated yearly on how to support vaginal breech births.
Induction of labour is generally not recommended for a breech birth. While vaginal breech birth carries the least risk for you, it does carry a small increased risk for your baby around the time of birth. A vaginal breech birth may also cause short-term complications for your baby. However, these complications do not seem to have any long-term effects. Your doctor or consultant midwife will answer any questions you may have.
A vaginal breech birth may not be advised if:
your baby is a footling or kneeling breech (one or both of the baby’s feet or knees are below its bottom)
your baby is larger or smaller than average (your doctor will discuss this with you)
your baby is in a certain position, for example, if its head is very tilted back (hyper extended)
you have a low-lying placenta or placenta previa
you have pre-eclampsia or any other pregnancy problems.
What can I expect in labour with a breech baby?
With a breech baby you have the same choices for pain relief as with a baby who is in the head down position. If you choose to have an epidural, there is an increased chance of a caesarean birth. However, whatever you choose, a calm atmosphere with continuous support should be provided. If you have a vaginal breech birth, your baby’s heart rate will usually be monitored continuously. This has been shown to improve your baby’s chance of a good outcome.
A midwife and doctor will be present at the birth. For some births the doctor or midwife may need to perform some manoeuvres to help the baby with birth. When you meet with your doctor or consultant midwife they will discuss these with you.
If there are concerns about your baby’s heart rate or if your labour is not progressing, you may need an emergency caesarean birth during labour. A paediatrician (a doctor who specialises in the care of babies, children, and teenagers) will attend the birth to check your baby is doing well.
Planned caesarean birth
The Royal College of Obstetricians and Gynaecologists (RCOG) recommend a planned caesarean birth takes place at 39 weeks. More information is available in the RCOG's Considering a caesarean birth leaflet.
Having a caesarean birth can increase your chances of problems in future pregnancies. These may include:
placental problems
difficulty with repeat caesarean birth surgery, and
a small increase in stillbirth in future pregnancies.
Contact Maternity Triage if you think you are in labour and you are having a planned caesarean birth. At the hospital your midwife will take your observations and monitor your baby. If you appear to be in labour your doctor or midwife may ask to perform a vaginal examination. This will allow them to assess the progress of your labour. If your baby is close to being born, it may be safer for you to have a vaginal breech birth. Your doctor will discuss all of your options with you.
What happens after the birth?
Most breech babies do not have any concerns following birth. Due to their position in your womb, breech babies do have an increased risk of hip problems. Your baby may keep their legs in the air for the first few days, which is normal and will settle. Your baby will have their hips checked during your stay in the hospital. Your baby will also be offered a follow-up hip ultrasound scan, this appointment is usually sent to you within 6 weeks. You can always contact Maternity Triage should you have any concerns.
What if I have any questions?
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Consider ‘Ask 3 Questions’
To begin with, try to make sure you get the answers to 3 key questions, if you are asked to make a choice about your healthcare.
What are my options?
What are the pros and cons of each option for me?
How do I get support to help me make a decision that is right for me?
Who can I contact if I have concerns?
Contact Maternity Triage on 01227 206737 for help and advice.
Ask your midwife or doctor for a referral to the consultant midwife.