Bladder care during labour and following birth
Information for women, birthing people, and their families
This aim of this leaflet is to explain and discuss the importance of bladder care and fluid balance. It will cover what will happen during labour, delivery, and immediately after birth.
We hope this leaflet helps to answer some of the questions you may have. If you have any further questions or concerns, please speak to your midwife or doctor.
It is important that you stay well hydrated in labour. Becoming dehydrated can cause your labour to slow or stop. We will observe how much you have drunk to make sure you do not have too little or too much fluid. All women / birthing people will be started on a fluid balance chart. Your midwife may ask you or your birth support person to write down what you have drunk and write it on the chart.
Why do I need to be on a fluid balance chart?
A fluid balance chart allows us to check how much fluid you are having and how much urine you are passing (weeing). Your fluid intake will include drinks and any medicines / drips that you may be having.
The aim is to balance your input (what you drink) and your output (urine / what you wee). Having too much fluid can cause fluid overload. This can be dangerous and cause damage to your kidneys.
Examples of the measurements of drinks available in the hospital
| Type of drink | Amount (ml = millilitres) |
|---|---|
| mug or cup of tea / coffee | 200mls |
| china cup of tea / coffee | 100mls |
| glass of water | 150mls |
| soup | 150mls |
| ice cream | 50 mls |
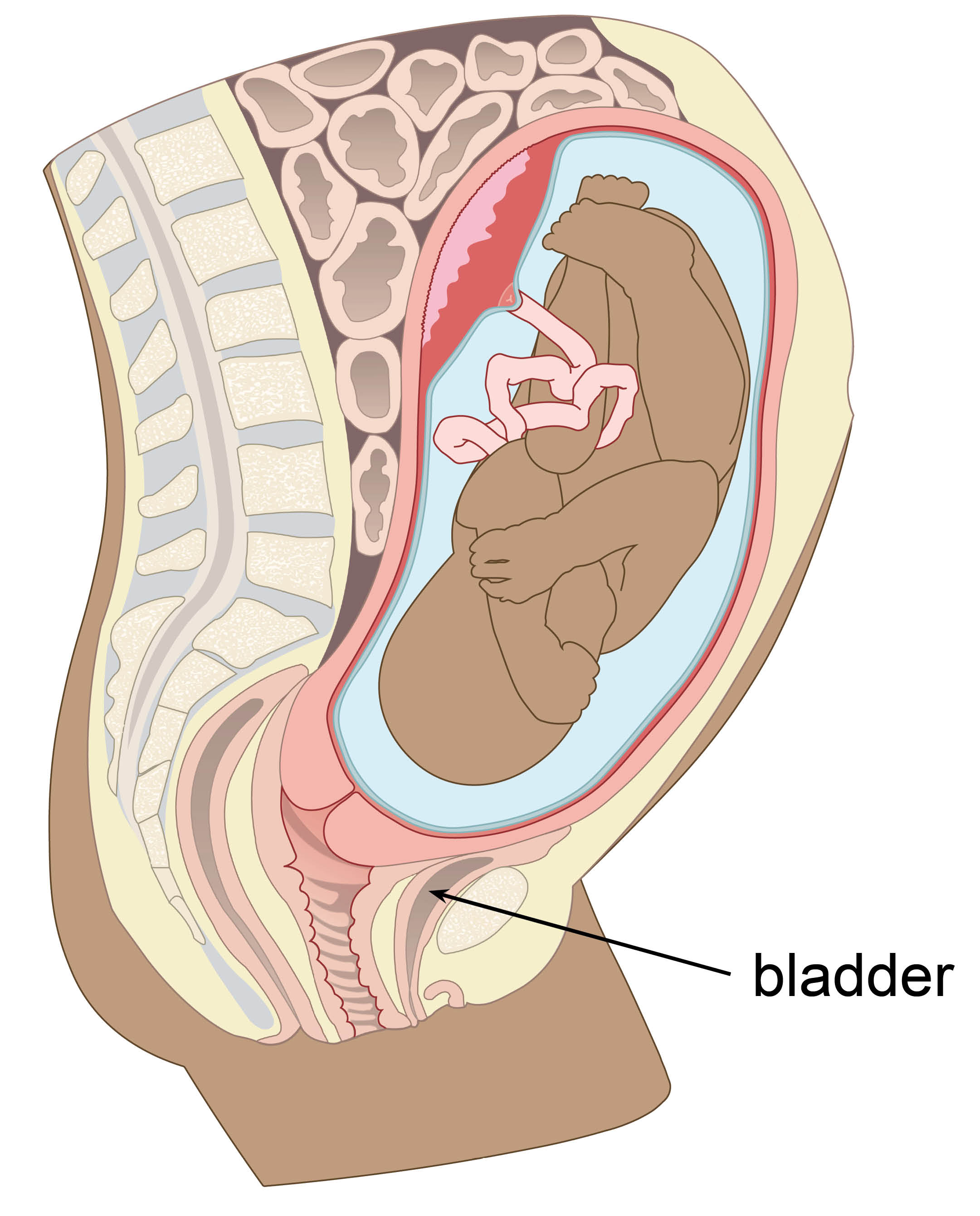
Your midwife will encourage you to empty your bladder regularly. This will allow your baby’s head to descend (move down) into your pelvis. This will help to reduce your risks of bladder trauma.
I am having a home birth. Do I still need a fluid balance?
Yes, it is still important for us to know how much fluid you are drinking, and that you are passing urine (weeing) well. At your home we will not be able to measure your urine. Instead your midwife will ask you if you feel you passed your ‘normal’ amount of urine.
You will be encouraged to empty your bladder regularly. This will enable your baby’s head to descend (move down) into your pelvis. This will help to reduce the risk of trauma to your bladder.
What if I am unable to pass urine (wee)?
If you are unable to wee every 2 to 3 hours while in labour, your midwife may discuss the following options with you.
Encouraging you to drink more if you are not drinking enough.
If you are unable to wee, your midwife may discuss an in / out catheter with you. A catheter is a small plastic tube that is passed into your bladder. An in / out catheter means your bladder will be emptied, and then the catheter is removed. Ideally you will not be catheterised more than twice, this is to reduce your risk of infection.
Your midwife or doctor may recommend that a urinary catheter is inserted. One that will remain in place until the delivery of your baby. This will depend on your individual circumstances. This could include if more than 1 in / out catheter is needed during labour.
What other reasons might I need a catheter?
Your midwife or doctor may discuss the need to have a catheter for the following reasons.
To empty your bladder using an in / out catheter before an operative vaginal delivery. This includes:
forceps
kiwi / ventouse (suction cup) delivery; or
an episiotomy, to speed up the delivery of your baby.
If you are having a caesarean birth or spinal anaesthetic for any reason.
If you are unable to pass urine (wee) after an epidural.
If you have any questions, please speak to your midwife.
Bladder care for a caesarean birth
When you have a spinal anaesthetic, you may not have the same sensation to wee, or you may not be mobile enough to do so.
Planned caesarean birth
If you are planning to have an elective caesarean birth, you will need to have a catheter inserted. This will normally be inserted when you are in theatre and you have been given pain relief. Catheter insertion can sometimes be a little uncomfortable, it is not usually painful.
Unplanned caesarean birth
If you need to have a caesarean birth that is not planned, you will need to have a catheter inserted. Depending on your individual circumstances this may be inserted:
When you are in theatre and have been given pain relief.
In the delivery room before you are transferred to theatre. This may happen in an emergency; but, you will be offered gas and air if needed.
How long will I need a catheter for?

Your catheter will normally be removed 12 to 24 hours (at least 12 hours) after delivery or spinal anaesthetic.
What happens after a vaginal birth?
If you had a vaginal birth without a catheter we still need to measure your urine output. You will be asked to tell your midwife when you have passed urine. Your midwife or another member of hospital staff will measure this for you. In hospital you will wee into cardboard container, which sits inside the toilet seat. This is so it can be weighed.
If you had a vaginal birth and had a catheter you will start a trial without catheter (TWOC). You will need to wee within 4 hours of removing the catheter. See below for more information on TWOC.
What if I had a caesarean birth or an operative vaginal delivery?
Some women / birthing people like to have pain relief before their catheter is removed. This is because once it is removed, you will need to start moving and walking. For more information, please see the Pain relief after caesarean birth leaflet.
You will then start a trial without catheter (TWOC). You will need to wee within 4 hours of removing the catheter. See below for more information on TWOC.
What if I am having problems passing urine?
You should try to be as relaxed as possible while trying to pass urine (wee). We understand you may feel worried about pain, especially if:
you had stitches; or
a caesarean birth.
Some women / birthing people find it helpful to turn the taps on in the bathroom / toilet. The sound of trickling water often helps. You can talk to your midwife if you have any worries or concerns.
Tell your midwife immediately if you have any problems passing urine. For example:
Frequency (regular trips to the toilet) and passing small amounts of urine.
Incomplete voiding (feeling like your bladder is not completely empty after weeing).
Bladder pain (lower tummy pain).
Hesitancy (difficulty in starting to wee).
Feeling you have a full bladder and are not able to empty it.
Incontinence / trickling of urine.
The amount of urine your bladder holds can increase in pregnancy. You can usually expect to wee larger amounts after the birth.
What is a trial without catheter (TWOC)?
TWOC is a method used to make sure that you are able to empty your bladder properly. It is performed after having a urinary catheter removed.
You will need to pass urine (wee) in the first 4 hours of your TWOC. It is important that you are able to empty your bladder well, this helps to stop:
urinary tract infections
your bladder becoming too full; or
being unable to pass urine (wee). This is called urinary retention.
A TWOC starts once your catheter has been removed. An indwelling catheter will stay in place, and remains in for at least 12 hours. An in / out catheter is inserted and removed straight away.
You will need to wee twice to complete your TWOC. Your midwife will ask you to let them, or another member of the maternity team, know every time you have been to the toilet.
You will be asked to wee into a cardboard container that fits inside the toilet, this is so it can be weighed. This tells us how much urine you have passed. Do not leave your urine collection in the toilet without giving it to a member of staff.
Your midwife will let you know if you have not passed enough urine (wee), or if you need do more measurements. They will also look at how much you are drinking, you may need to drink more.
You will need a bladder scan if you are unable to wee in the first 4 hours after your catheter has been removed.
What is a bladder scan?

A bladder scan is a non-invasive scan of your bladder.
Your midwife will place lubricating gel on your tummy, this can sometimes be a little cold.
A probe, like the one used during an ultrasound, is placed on your tummy. It is placed just above your pubic bone, over your bladder.
Your midwife will scan your bladder. This scan will tell us how much urine (wee) is inside your bladder.
The scan is not painful, but sometimes your midwife may need to use gentle pressure. This can be a little uncomfortable if your bladder is very full.
If your bladder contains more than 500mls, or you are uncomfortable. Your midwife may suggest using an in / out catheter to empty your bladder. You will then re-start your TWOC.
If your bladder contains less than 500mls, and you are comfortable. Your midwife or doctor will re-assess you in 2 hours. This will be no later than 6 hours after delivery or removal of your catheter. You will be encouraged to drink to please your thirst during this time.
What if I need extra bladder scans?
If you have an extra bladder scan, the results will lead to the following actions:
Less than 150mls in your bladder - TWOC passed.
150 to 250mls in your bladder – scan repeated in 2 hours time, or after you wee next. Whichever is sooner.
Less than 500mls but more than 250mls in your bladder – you will need an in / out catheter, and will then restart TWOC.
More than 500mls in your bladder – you will need a catheter inserted, this will stay in for 24 hours. After 24hours it will be removed, and you will restart your TWOC.
More than 1000mls in your bladder – you will need a catheter inserted. You will be sent home with the catheter for 7 days. For re-admission in 7 days to re-try TWOC.
What if I am still unable to wee and my TWOC is unsuccessful?
If this happens you will be sent home with an indwelling catheter for 7 days. This allows your bladder to rest.
On the 7th day you will be asked to call Maternity triage at 8am.
They will tell you the time to come to hospital to have your catheter removed. Their number is at the bottom of this leaflet.
Due to patient safety, on rare occasions you may have the removal of your catheter delayed. This will be discussed with you and will depend on your individual circumstances.
If you have any worries, questions, or feel unwell please call Maternity triage. Their number is at the bottom of this leaflet.
What happens when I go home?
After having a baby, it is important to look after your needs as well. Remember to drink to please your thirst. You should drink between 1.5 to 2 litres of water a day.
You might notice some changes with how you wee after having a baby. For example:
Feeling like you have less control over the flow / speed when you wee.
Suddenly feeling a strong and urgent need to wee.
You may leak a little wee before making it to the bathroom.
You may leak a little bit of wee when you sneeze, cough, or exercise.
If you have pain or are unable to wee, speak to your midwife or call Maternity triage for advice. Their number is at the bottom of this leaflet.
Pelvic floor exercises
It is important to start pelvic floor exercises as soon as you can. This helps to make your pelvic muscles stronger and helps with your healing. Only start these exercises when you feel comfortable.
Pelvic floor muscles help you control when you wee and poo, and can prevent leaking. You should wait until you feel comfortable before starting if you:
had a caesarean birth
had an operative vaginal delivery
forceps
kiwi or ventouse (suction cup); or
an episiotomy. A small cut between your vagina and anus (bottom).
had a third- or fourth-degree perineal tear.
Your pelvic floor muscles might feel weak at first. Exercising them makes them stronger. It is important to start slowly, and do more as you feel better. Do not give up. Pelvic floor exercises are helpful throughout your life.
Urinary incontinence is common during the late stages of pregnancy and after birth. Urinary incontinence is the unintentional leaking of wee.
Pelvic floor exercises usually fix the symptoms, but it can take a bit of time. Speak with your midwife or GP if you have bladder control issues. It can feel embarrassing to need extra help. Remember, that many other women / birthing people are experiencing the same thing.
Your midwife can refer you to physiotherapy, if they feel this will help you. For more information, see our Postnatal recovery: advice and exercise leaflet.
Will I get a urinary tract infection (UTI) after having a catheter?
You are at an increased risk of developing a UTI if you had a catheter during your delivery or after birth. Every care would have been taken when inserting the catheter. An a-septic (as clean as possible) technique is used when inserting the catheter. The risk of UTI and bladder retention (being unable to wee) increases each time a catheter is inserted.
It is possible to develop a UTI or have urine retention without having a catheter. This is because labour and birth can cause damage to your bladder. This is usually only a short-term issue, and resolves with resting your bladder.
What are the symptoms of a UTI?
It is important to be aware of the symptoms of a UTI. Some signs and symptoms can include:
pain or a burning sensation when weeing (dysuria)
needing to wee more often than usual
needing to wee more often than usual during the night (nocturia)
needing to wee suddenly or more urgently than usual
wee that looks cloudy
blood in your wee
lower tummy pain or pain in your back, just under the ribs
a high temperature, or feeling hot and shivery
a very low temperature, below 360°C
vomiting (being sick)
confusion
pain during sex
your wee may also be dark or smell strong. If this is your only symptom, it might be because you have not been drinking enough water.
If you have any of these symptoms, please tell your midwife or GP. If you feel unwell, contact Maternity triage for help and advice. Their contact details are at the bottom of this leaflet.
What is the treatment for a UTI?
If you have a UTI, you will need antibiotics. Your doctor will prescribe an antibiotic that is safe and works well for you and your baby. You will likely take the antibiotics for at least 3 to 7 days. These will usually be tablets.
Rarely, or if the infection is severe, you may need to have IV antibiotics. These are given in hospital, through a cannula. A cannula is a small plastic tube that goes into your vein.
It is safe to take antibiotics and breastfeed your baby.
How do I care for a catheter if I am sent home with one?
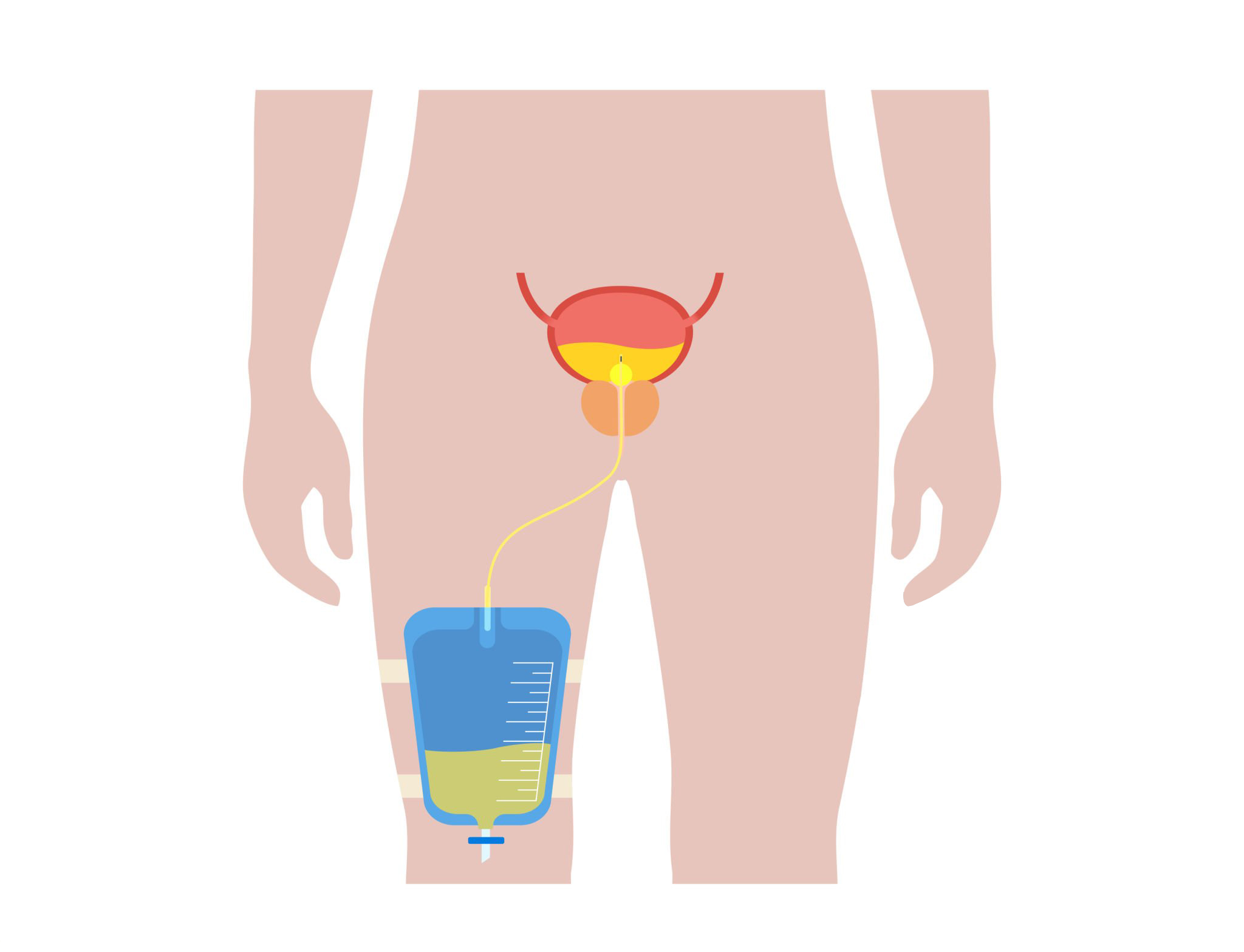
A catheter needs very little care.
Make sure that it is not allowed to hang and pull.
You can shower or bath as normal.
Empty the bag regularly. Do not allow the bag to become full, or it may leak or break.
For more information, please read the Going home with a urinary catheter leaflet.
Useful contacts
Contact our Maternity telephone triage service on 01227 206737 for help and advice.
Contact Birth Afterthoughts service if you have any unanswered question about your experience. You can call or email, and ask to arrange an appointment with ‘Birth Afterthoughts’.
Call Maternity Liaison 9am to 3:15pm on 01227 864152
Useful links
East Kent Hospitals. Postnatal recovery: advice and exercise patient information leaflet.
East Kent Hospitals. Going home with a catheter patient information leaflet.
East Kent Hospitals. Pain relief after caesarean section patient information leaflet.
References
East Kent Hospitals University NHS Foundation Trust. Bladder Care Guidelines for Labour and Post-Partum Period. April 2024.
