Appendicitis and surgery
Information for patients having a day case surgery for appendicitis (planned and emergency)
You have been diagnosed with appendicitis. This leaflet will explain:
what your treatment options are
what happens during surgery; and
how you may feel afterwards.
We hope it will help to answer some of the questions you may have. If you have any further questions or concerns, please speak to a member of your healthcare team.
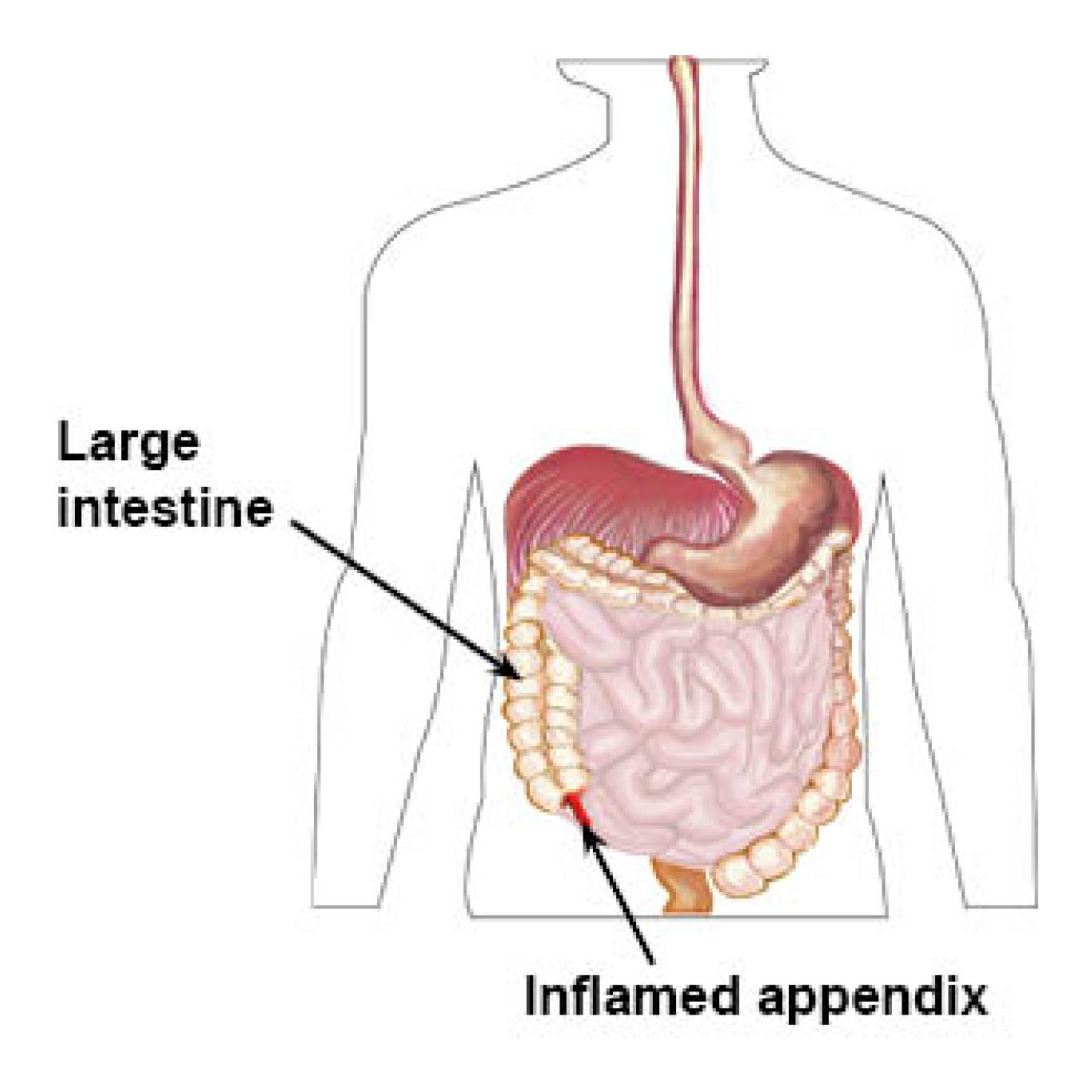
What is the appendix?
The appendix is a small thin structure approximately 5 to 10cms long. It is connected to the large intestine on your right-hand side.
Having you appendix removed will cause you no long-term harm, as you can happily live without one.
What are my treatment options?
The usual treatment for appendicitis is surgery. However, if it is uncomplicated and this option is appropriate for you, it is possible to treat appendicitis with antibiotics. Your surgeon will discuss your options with you before you make any decisions.
What is an appendicectomy?
The surgery is called an appendicectomy and involves removing your inflamed appendix. This is done either with laparoscopic (keyhole) surgery or open surgery.
Your surgeon will explain both options to you, before you and your surgeon decide which is the best for you.
Will I have a general anaesthetic?
Yes, you will have a general anaesthetic for this procedure (you will be asleep during surgery).
What happens next?
Once you have discussed your options with your surgeon, they will ask you to sign a consent form. You can ask your surgeon any questions before you agree to the procedure.
You will also be seen by an anaesthetist before your operation. Please ask them any questions about the anaesthetic and pain relief.
Why do I need to sign a consent form?
All patients must give permission before they receive any type of medical treatment, test, or examination. Consent is usually given when you sign the consent form before your treatment, but we may ask you to give it verbally.
You must give your consent voluntarily.
The hospital must give you all the information you need to make a decision about your treatment. This is so you can give us informed consent. If you have not been given this information, or you have but you still have questions, please speak to a member of staff.
You must be capable of giving consent. This means that you understand the information given to you and can make an informed decision.
When we ask you to give consent, please use this time to ask any questions you may still have. For more information, please go to the NHS Consent for Treatment web page. Remember, you can withdraw your consent for treatment at any time.
How long will I be in hospital for?
An appendicectomy is usually performed as a day case procedure. A day case procedure is where you come into hospital for your surgery and go home later the same day. You do not stay in the hospital overnight.
If you do need to stay in hospital overnight, your surgeon will discuss this with you after your surgery.
What is laparoscopic (keyhole) appendectomy?
Laparoscopic surgery means keyhole surgery. It allows a surgeon to use small cuts and a camera for procedures inside the tummy or pelvis.
In most laparoscopic appendicectomy operations, surgeons operate through three small incisions (cuts), while watching an enlarged image of your internal organs on a television monitor. In some cases, one of the small openings may be made bigger to complete the procedure.
The appendix is usually removed through an incision in the right lower abdominal wall.
What are the advantages to having a laparoscopic rather than an open surgery?
Open surgery means cutting the skin and tissues, so the surgeon has a full view of the structures or organs involved.
Common advantages of having a laparoscopic surgery rather than an open surgery.
Less pain after surgery.
A shorter hospital stay.
A quicker return to bowel function (being able to go to the toilet).
A quicker return to normal activity.
Better cosmetic results (the scarring will be smaller).
Results may vary depending on the type of procedure you have and your general condition.
Can I have a laparoscopic appendicectomy?
This depends on how complicated your appendicitis is. If appendicitis is found early, most cases are treated successfully with keyhole surgery. Some patients who have complicated appendicitis may not be suitable for keyhole surgery. Complications can include inflammation or an abscess.
If your surgeon faces difficulties or they feel it is safer not to proceed with keyhole surgery, they will perform open surgery. Difficulties can include not being able to see or access your organs clearly. Having open surgery is not a complication, but rather a sound surgical judgment. This will happen to between 5 and 10 out of every 100 patients having an appendicectomy.
The chances you will have open surgery increase if:
You have an extensive infection and / or an abscess
You have a perforated appendix
You are obese (overweight, with a body mass index (BMI) of over 30)
You have already had abdominal surgery causing thick scar tissue to form
Your surgeon cannot see your organs
You have bleeding problems during your operation.
What will happen after my surgery?
After your operation, you will be taken to a ward to rest and recover.
You can start eating and drinking when you are fully awake, unless you are told not to.
Your surgical team will visit you on the ward to see whether you can go home. It is likely that you can cope at home, when:
your pain is well controlled
you do not feel dizzy; and
you have gone to the toilet.
How will I feel after my surgery?
Every patient is different but you should feel better each day. Some people feel better just a few days after their surgery. Remember to take it slowly, your body needs time to heal.
Try to get out of bed the day after your surgery and walk around. This will help reduce the risk of blood clots in your legs and soreness in your muscles.
You will probably be able to get back to most of your normal activities within a few days. These activities include showering, a gentle walk, and office-based work.
Shower with your dressings on until three days after your surgery. After each shower change the dressing for dry ones. After three days, it is ok to get your wound wet.
Your surgeon will use dissolvable sutures to close your skin, so your stitches will not need to be removed.
You will not need a follow-up appointment after your surgery.
Do not drive for at least one week after your operation. Before you can drive again, you must be able to perform an emergency stop without it hurting. If in doubt, speak with your GP or insurance company.
When can I return to work?
You can return to work when you feel well and comfortable enough. If you have an office-based job this is usually after two weeks. It can be at least a month if your job is physical or manual. If in doubt, ask your GP for advice.
When should I contact my GP or the hospital?
Contact your GP or the Surgical SDEC (Same Day Emergency Care) immediately if you develop any of the following symptoms.
Persistent fever over 101⁰F (39⁰C).
Bleeding from your wound or back passage.
Increasing abdominal distension (swelling) or bloating.
Pain that is not relieved by your usual painkillers, such as paracetamol.
Persistent nausea (feeling sick) or vomiting. You are unable to keep down anything you eat or drink.
Persistent cough or shortness of breath.
Pus in your wounds.
Redness surrounding any of your incisions, that is getting worse or bigger.
Contact details
Surgical SDEC (Same Day Emergency Care)
Queen Elizabeth the Queen Mother (QEQM) Hospital, Margate
Telephone: 01843 235143Surgical SDEC (Same Day Emergency Care)
William Harvey Hospital, Ashford
Telephone: 01233 651931