Anterior resection
Information for patients from the Association of Coloproctology of Great Britain and Ireland (ACPGBI)
An anterior resection is an operation to remove the rectum or a part of it.
What is the rectum?
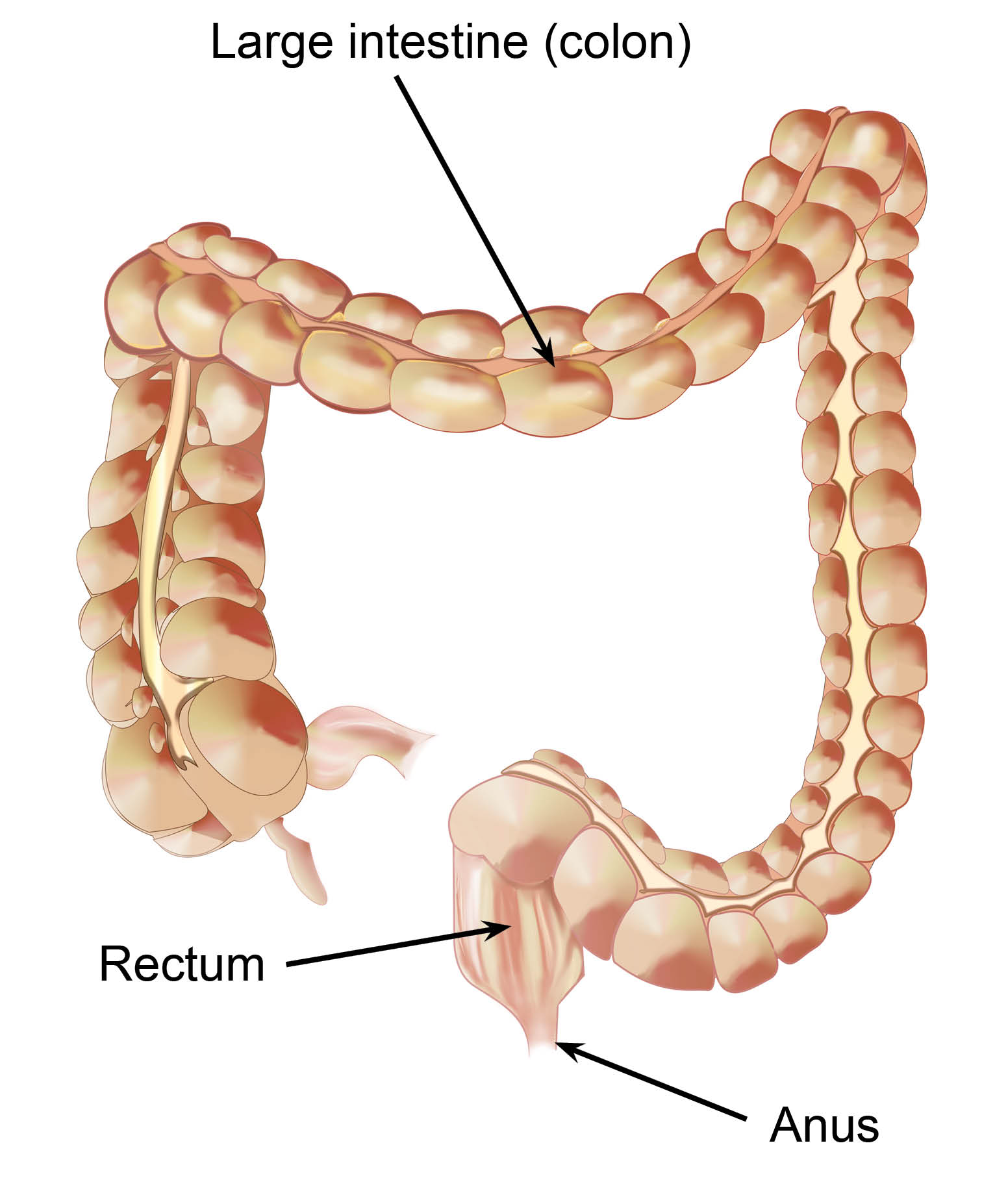
The rectum forms part of the large bowel, following on after the colon. It is the lowest part of the digestive system near your bottom, and it stores waste material. Emptying of the rectum is controlled by the anal sphincter muscles of your ‘back passage’.
What happens during the operation?
The operation can be done in two ways.
It can be done as an open operation, which means there will be one long incision (cut) down the middle of your abdomen (tummy). The other way is by laparoscopic (keyhole) surgery using a few small incisions.
After removing the portion of the rectum, your surgeon will join the two healthy ends together using either a series of sutures (stitches) or staples. This is called an anastomosis.
Whether you have open or laparoscopic surgery will depend on many things. Each case has to be looked at individually, and you will need to discuss your options with your surgeon and find out which way of operating is best for you.
If you have a laparoscopic (keyhole) operation
Your surgeon will make four or five small (1cm) cuts in your abdomen. They will put a telescope camera into one of these small cuts to show an enlarged image of the organs in your abdomen (on a television screen). The other cuts allow the surgeon to use special operating instruments. Your surgeon will make one of the cuts longer (8 to 10cms) so they can remove the portion of the bowel they have operated on.
Sometimes it is not possible or safe to finish the operation using laparoscopic surgery. If so, your surgeon will change to an open operation and make a larger incision to deal with this.
Will I need any special preparation before surgery?
You will have investigations and tests to prepare you for your operation. These are to confirm your diagnosis, to see how far the disease has spread, and to assess how fit and well you are for the proposed treatment.
It is likely though not always the case, that you will have to take a special prescribed drink (oral bowel preparation) in the 24 hours before your operation. You may be given this to take at home
before you go into hospital, or you may be given it in hospital. If you take the bowel preparation while you are at home make sure you can get to a toilet easily, since it will mean you will need to empty your bowels quite often and you may need to rush to the toilet. You should only drink clear fluids (such as water or flat lemonade) although the specialist nurse may give you high-energy drinks.
Will I need to have a stoma (bowel bag)?
Patients often need to have a stoma, even more so if they have had chemotherapy or radiotherapy leading up to a planned operation.
A portion of the bowel is brought out onto the abdomen to form an opening outside the body, known as a stoma. A stoma bag is then fitted around this opening to collect the contents of your bowel. The stoma ‘rests’ the anastomosis (the join where the bowel is connected back together) allowing it to heal and for you to fully recover. Despite the stoma you may pass a little old blood or mucus from your back passage.
The stoma may be permanent or temporary.
If you need a stoma or it is possible that you may need a stoma, you will be seen by a stoma nurse. These specialist nurses are skilled in caring for patients who have a stoma. They will be able to answer any questions you may have.
Are there complications with this operation?
The risks of this operation are small and much less likely to affect you than the risk of doing nothing. However, this is a major operation and some people (less than one in 20) do not survive the surgery.
There are sometimes complications. These may include:
Bleeding
Infection
A leak from the anastomosis (the join where the bowel is connected back together)
Injury to other organs within the abdomen (for example the small intestine, ureter, or bladder)
Problems passing urine (though this is usually only temporary)
A lack of sexual desire, and in men a difficulty in achieving an orgasm and maintaining an erection (though this is usually only temporary)
Deep vein thrombosis (blood clots in the veins in the legs)
Pulmonary embolisms (blood clots in the lungs).
You may also have the following:
A sore bottom
If you did not need a stoma, you may have difficulty in controlling your bowels in the first few weeks after surgery, which may mark your underwear. It may be helpful for you to do some pelvic floor exercises. These will help the muscles in your bottom cope with having a part of your back passage removed. Sometimes it takes several weeks to get back to normal, and occasionally you may have to make changes to your diet.
Anxiety due to the whole situation.
What should I expect after surgery?
Immediately after your operation (within the first 24 to 48 hours), you will need:
oxygen through a face mask
a drip into a vein in one of your arms to give you fluid
a catheter (tube) in your bladder to drain away urine, and
medication to deal with pain from the incisions; this may be given as an epidural (where the medicine is given through a fine tube in your back) or through the drip.
Later (the following day or so), you will need to:
start eating again, starting with liquids and gradually introducing solid foods, and
move around as soon as possible.
If you have laparoscopic surgery, you may recover more quickly after surgery and go home sooner.
How long will I need to be in hospital?
You will stay in hospital for as little time as possible, usually between five and seven days. Your surgeon or specialist nurse will discuss with you the daily achievements that you should try to meet. This programme is called ‘enhanced recovery after surgery’ (ERAS).
If after you leave hospital, you have any new concerns or problems (for example severe abdominal pain, a raised temperature, or bleeding from your back passage) it is important to contact your own doctor (GP) or the hospital. You will be given contact numbers when you leave hospital.