Anterior Cruciate Ligament (ACL) injury
Information for patients from the Physiotherapy Department
This booklet belongs to: _____________________________________________________
Your trauma and orthopaedic consultant / surgeon is: ____________________________
Orthopaedic appointment date: _____________________________________________
Orthopaedic appointment date: _____________________________________________
Orthopaedic appointment date: _____________________________________________
Orthopaedic appointment date: _____________________________________________
Surgery date (if applicable): ________________________________________________
Your physiotherapist is: _____________________________________________________
Physiotherapy appointment date: ___________________________________________
Physiotherapy appointment date: ___________________________________________
Physiotherapy appointment date: ___________________________________________
Physiotherapy appointment date: ___________________________________________
My personal goals that I want to return to (for example running and football). Please explain why you want to achieve this goal.
Goal 1: __________________________________________________________________
_________________________________________________________________________
_________________________________________________________________________
Goal 2: __________________________________________________________________
_________________________________________________________________________
_________________________________________________________________________
Goal 3: __________________________________________________________________
_________________________________________________________________________
_________________________________________________________________________
This booklet is designed to help you after an anterior cruciate ligament (ACL) injury.
It explains your injury.
Guides you through your options for treatment.
Advises you of exercises that you can start doing immediately after your diagnosis of an ACL injury or after ACL reconstructive surgery.
Depending on how bad your injury is, you may have options as to how your ACL injury is managed and whether surgery is needed. This decision will be made by you with advice from your surgeon, knee specialist, and physiotherapist. The options are:
Conservative (no surgery) management and rehabilitation of your ACL injury. You can change your mind about conservative management and choose to have surgery at a later date if you wish.
Surgical management and rehabilitation has two stages:
before your ACL reconstructive surgery (pre-operative); and
after your surgery (post-operative).
It is important you are as strong as possible before ACL reconstructive surgery and it is very important that you follow the exercise guidance for after your surgery. This booklet covers exercises for each of these stages.
You should follow the advice in this booklet with the guidance from your physiotherapist. It is your responsibility to complete the exercises described in this booklet depending on whether you have had surgery or not. The exercises will help your knee to recover, regain movement, and build muscle strength, within the appropriate time frame. The time frames given are average guidelines and it is important to remember that everyone will progress at different rates.
Contents
What is the ACL?
What can cause an ACL injury?
Can an ACL injury cause other problems?
How is an ACL injury diagnosed?
Will I need ACL reconstructive (ACLR) surgery?
What if I choose not to have surgery, and the non-surgical options have not worked?
How do I care for my knee after my ACL injury?
How will I recover from my ACL injury?
Who will refer me for physiotherapy?
I am waiting for ACL surgery, do I still need physiotherapy?
What exercises can I do when my ACL injury is diagnosed? Will these exercises hurt?
What happens in ACL reconstructive surgery?
What is ACL reconstructive surgery?
How successful is ACL reconstructive surgery?
How long does it take to recover from ACL reconstructive surgery?
What are the risks of having ACL reconstructive surgery?
What should I do after having ACL surgery?
Will I have a follow-up appointment?
When can I start my exercises after surgery?
Phase 1: week 0 to week 2 after surgery
Phase 2 (on average 2 to 6 weeks after surgery)
Useful contact details
What is the ACL?
The knee is made up of two joints: one between the thigh bone (femur) and the shin bone (tibia), and one between the femur and knee cap (patella). The knee is also made up of lots of muscles, ligaments, and cartilage. Muscles and cartilage help the knee to move, while ligaments provide most of the stability of the knee.
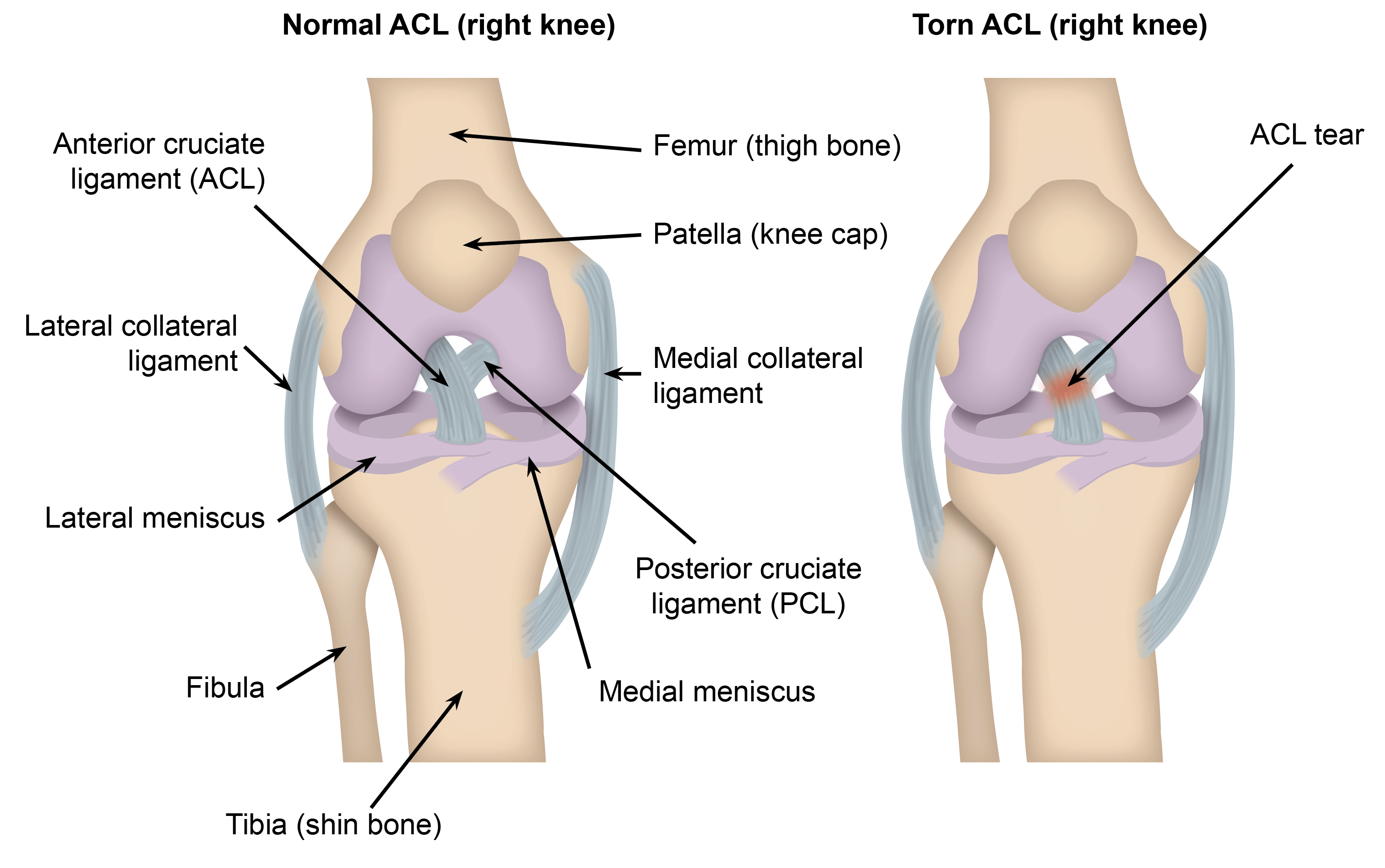
The ACL is a tough band of tissue that runs diagonally within the knee. It helps to prevent forward movement and twisting of the tibia (shin bone) on the femur (thigh bone). Also with the help of your muscles, it provides most of the knee’s stability.
The other main function of the ACL is to provide your brain with information about your knee’s movement and your balance. This is called ‘proprioception’ and happens mostly without us knowing.
What can cause an ACL injury?
An ACL injury happens when the ACL is torn (ruptured), or stretched beyond its normal ability (partial tear or sprain). This usually happens during sport, most commonly due to a twisting of the knee. An injury can also be caused by suddenly stopping or changing direction, or if you bump into someone.
To start with, this can cause your knee to swell, be difficult to move, and painful to walk on. After this, as the stability of your knee is reduced it might feel unstable or give way.
Can an ACL injury cause other problems?
When you injured your ACL, you may have also injured other parts of your knee. The most common injuries are listed below.
The meniscus. One of the most common injuries linked to an ACL injury occurs to the meniscus. The meniscus is a C shaped structure within both sides of the knee which acts as a shock absorber, its main role is to protect the bone. Tears to the meniscus can lead to pain, ongoing swelling of the knee, and the knee locking and clicking. The meniscus has a poor blood supply, so certain tears do not heal which can lead to the early development of arthritis in the knee.
The collateral ligaments are a complex group of ligaments found on either side of the knee, known as the medial collateral ligament (MCL) on the inside of the knee, lateral collateral ligament (LCL) on the outside of the knee, and the posterolateral corner complex (PLC). Due to their complex structure, different parts of the ligament can be injured. Injuries can range from a sprain, all the way to a full tear (a rupture) of the ligament.
Chondral injuries. The bones around the knee are all covered in a thick layer of cartilage, which helps the knee move with as little friction as possible. It is the “wear and tear” of this cartilage that leads to osteoarthritis, which is when there is loss of this cover exposing the underlying bone. Due to the mechanism of injury when tearing the ACL, this lining can be damaged in isolated areas leading to loose bodies within the knee joint, or flaps of cartilage which can lead to clicking and pain within the knee.
The posterior cruciate ligament (or PCL) sits next to the ACL in the centre of the knee. Its main role is to stop the thigh bone (femur) sliding forward on the shin bone (tibia). Injuries to this ligament usually heal well but when it happens with other injuries (such as with an ACL injury) it may heal with laxity (some looseness). This laxity can cause problems with instability, particularly when going downstairs, and can lead to long-term problems with knee cap (patella) pain.
Bone injuries can happen in almost all ACL injuries, due to the bone against bone impact that occurs at the time of the injury. What happens is that the bone around the knee is a similar texture as honeycomb, and when there is an impact injury the holes in the honeycomb can get damaged. Sometimes there are fractures linked with an ACL injury, the most common one is known as a Segond fracture. This happens when a ligament around the knee is pulled off the outside of the shin bone (tibia). It does not need treatment as other fractures would, but may be looked at during an operation as it can lead to increased instability.
Less common injuries. Other injuries linked with ACL injuries are far less common, but include injuries to the quadriceps tendon (muscle on the front of your thigh), the patella, and neurovascular injuries (injuries to nerves and bloods vessels) around the knee.
Injuring your ACL on the other side. Research shows that around 16 in every 100 people can injure their ACL in the other leg to their original injury.
How is an ACL injury diagnosed?
In order to diagnose ACL injury, your surgeon or knee specialist will talk to you about the history of your injury, examine your knee, and arrange for scans to be taken. Most patients with an ACL injury will have an x-ray at the time of their injury, but their diagnosis will be confirmed with an MRI scan. This will usually be organised by a surgeon or knee specialist rather than the Emergency Department team. Your surgeon or knee specialist will explain any associated injury and what the next steps are.
Will I need ACL reconstructive (ACLR) surgery?
The body cannot repair a fully ruptured ACL, but not everyone with a ruptured ACL needs to have ACL reconstructive surgery. This is because some people’s injured knee will not keep ‘giving way’ or have instability issues, or you might be happy to make changes to your activities to stop this from happening, or you have not significantly damaged any other areas of your knee.
You can choose to have ACL reconstructive surgery or choose not to have surgery (conservative management). Decisions about your ACL injury management should be made jointly with your surgeon, knee specialist, and physiotherapist. ACL surgery is completed by trauma and orthopaedic surgeons.
What if I choose not to have surgery, and the non-surgical options have not worked?
In some cases, conservative management does not always help your pain and mobility, and you may continue to feel pain and instability in your knee. If this happens, you can choose to have surgery to stabilise your knee or continue to manage without surgery. However, it is unlikely that your condition will get better on its own, and if you choose not to have surgery you could develop early onset osteoarthritis. If you still choose not to have surgery, it is important for you to continue your exercises regularly, to keep as much strength and stability in your leg as possible.
How do I care for my knee after my ACL injury?
In the first few days after an ACL injury, it is important to cut down your activity levels, but you can begin the exercises under the heading Will these exercises hurt?. If you have had ACL surgery, please go to the exercises under the heading Phase 1: week 0 to week 2 after surgery.
You can also use pain relief or a knee support / tubigrip to help with your pain.
If your knee is swollen, please use ice. For more information, please ask a member of staff for a copy of the Trust’s Ice Treatment leaflet.
Unless you have been told by a surgeon or knee specialist not to, you can walk full weight-bearing (you can put weight through the injured leg or foot when you are walking). A member of the Emergency Department staff, surgeon, or knee specialist may give you crutches if you are struggling to walk, or a brace if they think this is necessary.
How will I recover from my ACL injury?
Whether you choose to manage your injury conservatively (no surgery) or choose to have ACL reconstructive surgery, your rehabilitation after your ACL injury will:
Be guided and informed by your surgeon or knee specialist. They will discuss how to manage your ACL injury and discuss whether they recommend you have surgery, and / or give you a knee brace or guidance on weight-bearing for your knee.
Be managed by your physiotherapist, who will outline which exercises you need to complete to achieve your personal goals. The exercises you are given will depend on your knee injury, any weight-bearing restrictions you have, or any limitations of movement you have from the knee brace given to you by surgeon or knee specialist.
Who will refer me for physiotherapy?
Your surgeon in Trauma and Orthopaedics (T&O) or knee specialist (Fracture Clinic) will refer you to physiotherapy, whether you are having ACL surgery or not.
You will have an appointment with a physiotherapist, and have the option to join our specialist ACL class. These classes will allow you to come to physiotherapy appointments more often, where we can support you to achieve your personal goals. The ACL classes are run by physiotherapists at the Physiotherapy Outpatient Department at William Harvey Hospital in Ashford, Kent and Canterbury hospital in Canterbury, and Queen Elizabeth the Queen Mother hospital in Margate.
It is important for your recovery to make every effort to go to your physiotherapy appointments.
Your physiotherapist will guide you through the exercises that you need to complete at each appointment. To start with, the aim is to regain full active range of movement of your knee, and be able to walk without using a walking aid or limping. Your physiotherapist will be working with you to regain full and equal strength and balance in your injured leg, and building power and endurance with control so that you can achieve your personal goal.
I am waiting for ACL surgery, do I still need physiotherapy?
Yes, definitely.
Evidence shows that by taking part in physiotherapy and doing rehabilitation with physiotherapists before having any potential surgery, you will be more likely to return to sport after surgery. The stronger you are going in to surgery, the stronger you will be after surgery. Depending on whether you have injured other parts of your knee and the type of surgery that you may need, your surgeon may say that you can only partially or non-weight-bear after surgery, meaning you must limit how much weight you put through your injured leg after surgery. If this applies to you, physiotherapists will support you to build up your arm strength as well as strengthening your legs before surgery.
It is possible to injure the ACL in your other knee (see What can cause an ACL injury? section). Starting physiotherapy straight after any injury and after surgery can help prevent further injuries.
What exercises can I do when my ACL injury is diagnosed?
If you have had an ACL injury diagnosed you can start doing the exercises on the next page, as long as you have not been given specific instructions by a surgeon or knee specialist to not move your knee and / or weight-bear through your knee. If you have been told this, please wait until you have seen a physiotherapist before you start doing any exercises.
The aims of these exercises are to:
Reduce swelling and pain in your knee
Regain your full range of movement, for example bending and straightening your knee as far as possible
Regain strength in your injured leg, so that it is the same strength as your uninjured leg
Improve your balance
Walk without support, such as elbow crutches or without limping
These first exercises aim to help you regain full active range of motion and keep a good blood flow after your injury. You need full range of movement to walk without limping and achieve your personal goals.
Start the exercises gently, increasing the stretch a little each time. Aim to practice each exercise:
two to three times a day (set), with eight to 12 repetitions (reps) each time; rest for 60 to 120 seconds between each set (rather than doing one set in the morning, one at lunch, and one in the evening).
at least three days a week, but no more than five days.
Will these exercises hurt?
It is normal to feel sore during or the day after you exercise.
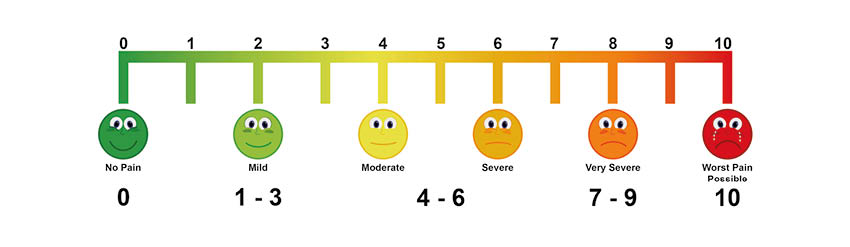
If 0/10 is no pain and 10/10 is the worst pain you have ever felt, any pain that you have up to 4/10 when you are doing these exercises or afterwards is acceptable. However, if your pain level increases above 4/10, or you have swelling during or immediately after exercise, please do the following until your pain is reduced and manageable.
Reduce the number of repetitions or sets you do.
Reduce the speed at which you are completing the exercises.
Increase the rest time in-between repetitions or sets.
You should not have to take more pain relief tablets to complete your exercises. If your pain is very high or unbearable, and you have not had recent surgery, please talk with a pharmacist or GP. If your pain is very high due to these exercises, please email the Physiotherapy Team. Please note this email account is not checked over the weekend and it may take 24 to 48 hours to get a reply. Once your pain has settled, gradually increase the number of repetitions, sets, or speed over time.
Exercises
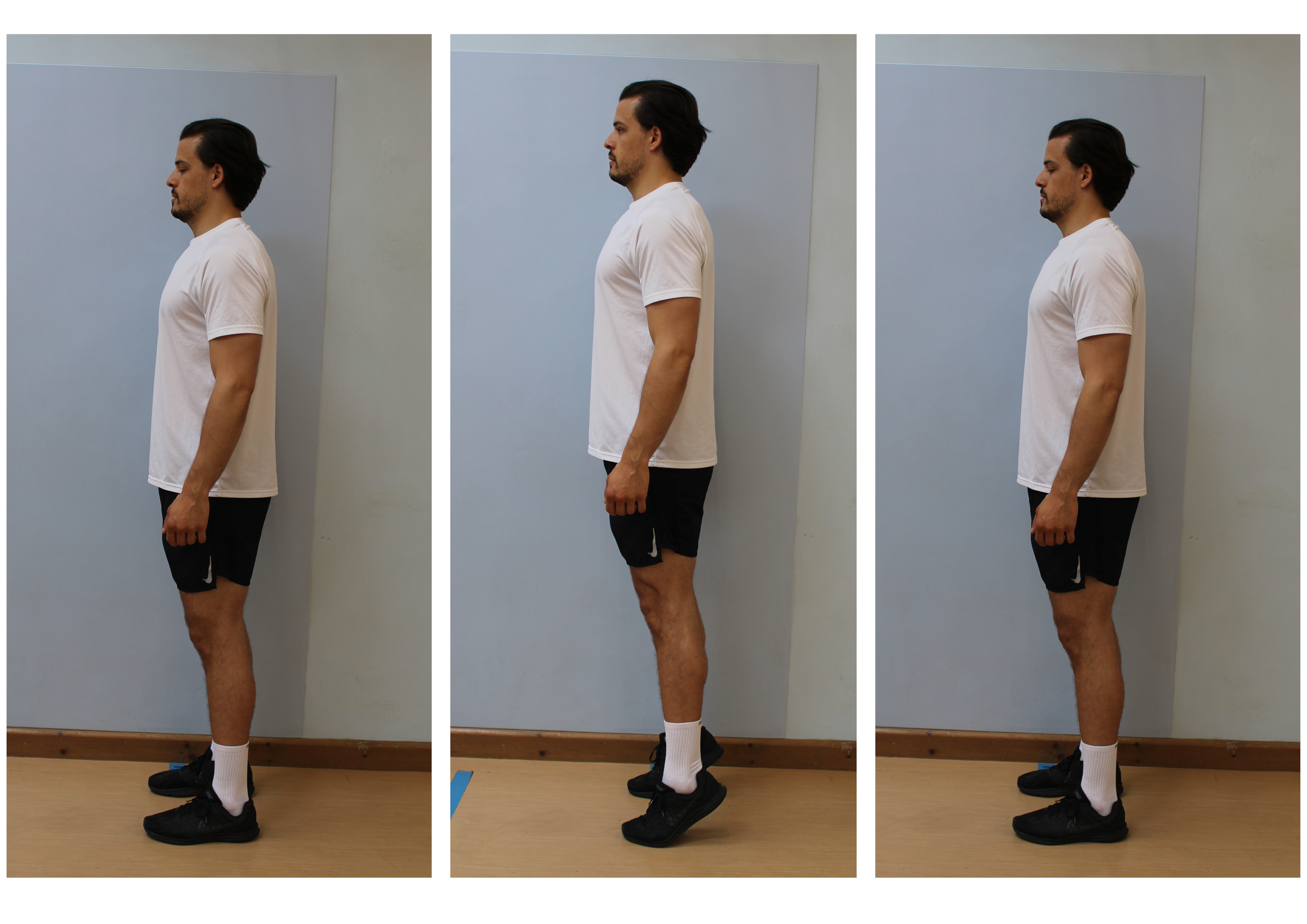
These exercises are shown with the model’s left knee. Please complete the exercises on whichever leg is injured. These exercises are for you to complete before any surgery that you may have. If you have already had ACL surgery, please go to Phase 1: week 0 to week 2 after surgery.
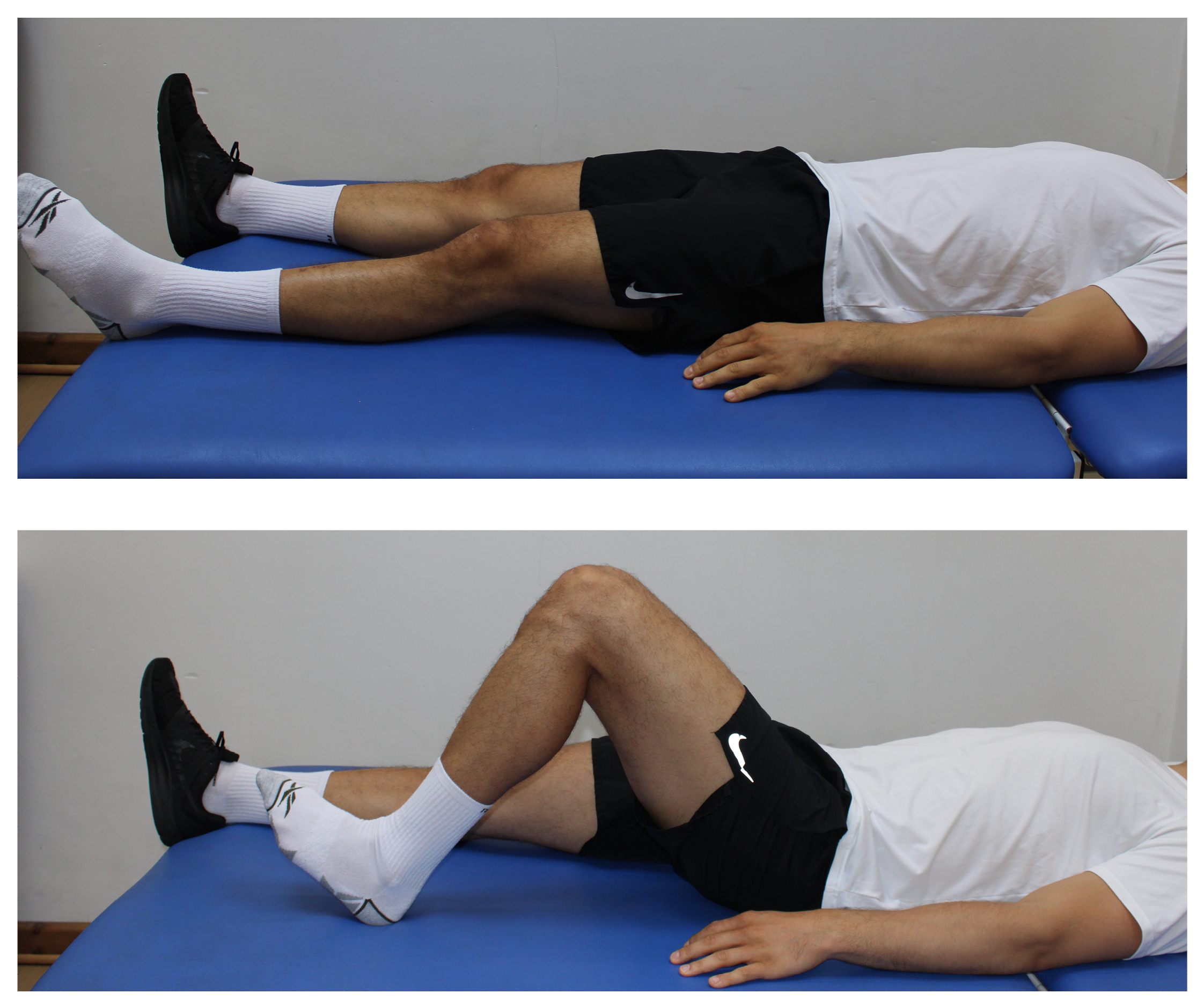
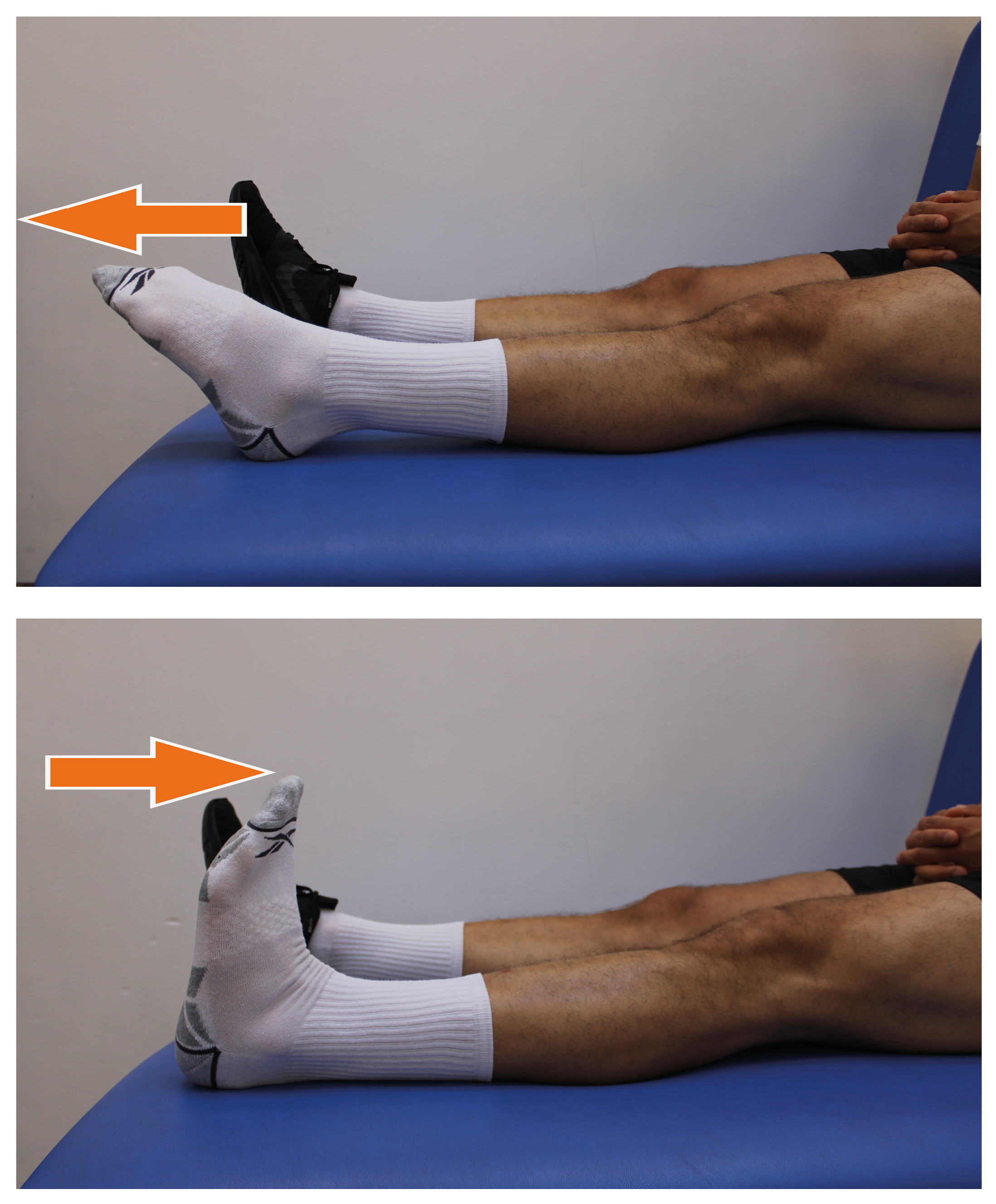
1.Heel slides
Lie down.
Gently slide your heel up and down, allowing your knee to bend and straighten as far as possible.
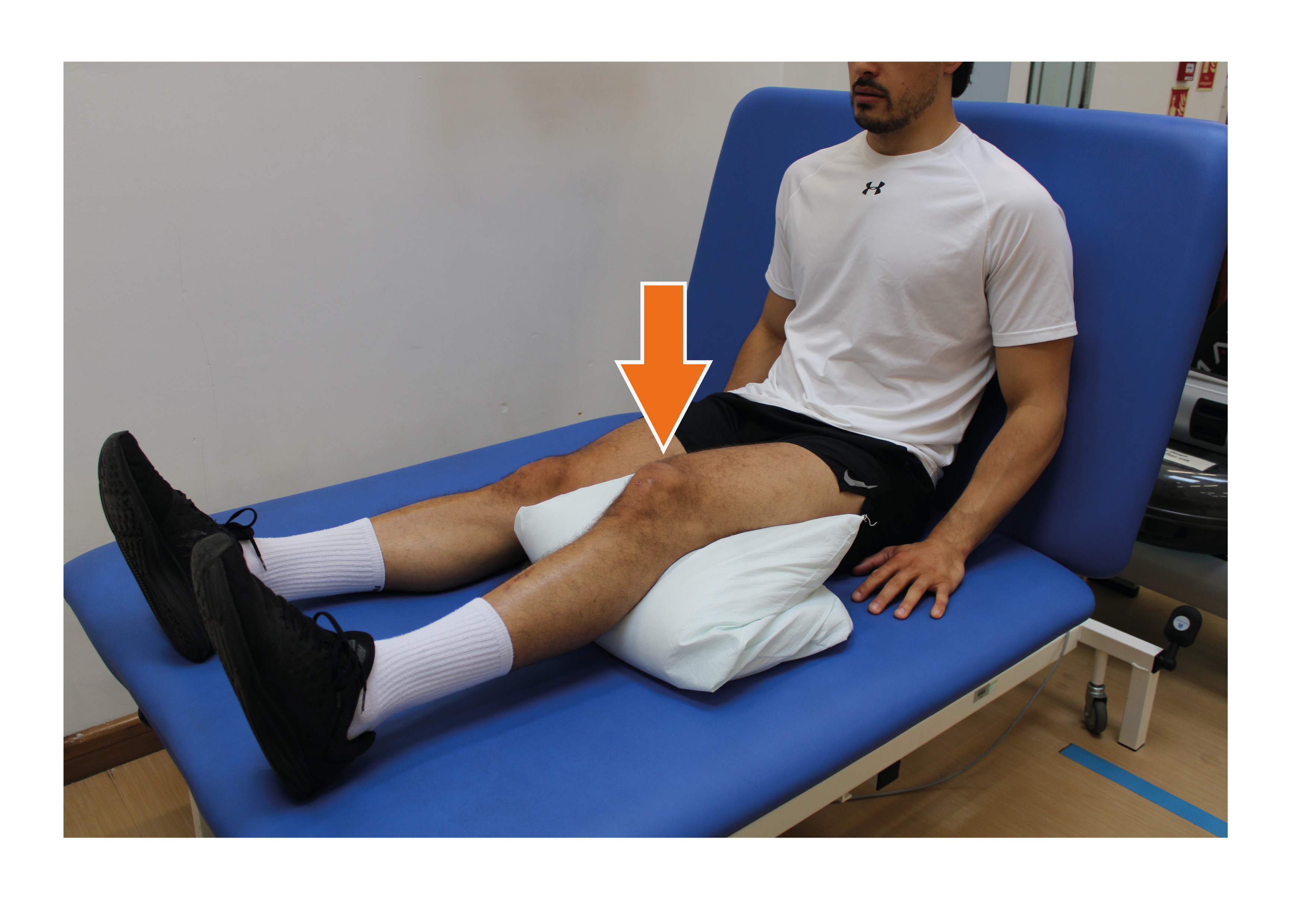
2.Knee sags
Sitting with your legs straight, place the injured leg’s heel on a cushion and let gravity pull the knee straight.
If comfortable, gently push on the knee to try and straighten it.

3.Static quads
Sit with your legs straight.
Gently tense and relax your thigh muscle, without moving your knee.
4.Ankle pumps
Sitting or lying down, quickly bend and straighten your ankles.
Once you have completed the following three points, you can move on to the strengthening exercises below.
Achieved full range of movement of your knee (you can bend and straighten your injured knee as much as your un-injured side).
Completed the exercises above, and are finding them easy to do.
Have seen your knee specialist or physiotherapist who has given you the OK to start the strengthening exercises below.
Aim to practice each exercise:
two to three times a day (set), with eight to 12 repetitions (reps) each time; rest for 60 to 120 seconds between each set (rather than doing one set in the morning, one at lunch, and one in the evening).
at least three days a week, but no more than five days.

1.Inner range quads
Sit with your legs straight out in front of you.
Place a cushion or rolled-up towel underneath your knee.
Tighten your thigh muscle, lifting your heel off the surface that you are on.
Press the back of your knee into the towel to lift your heel; do not try and lift your whole leg up.
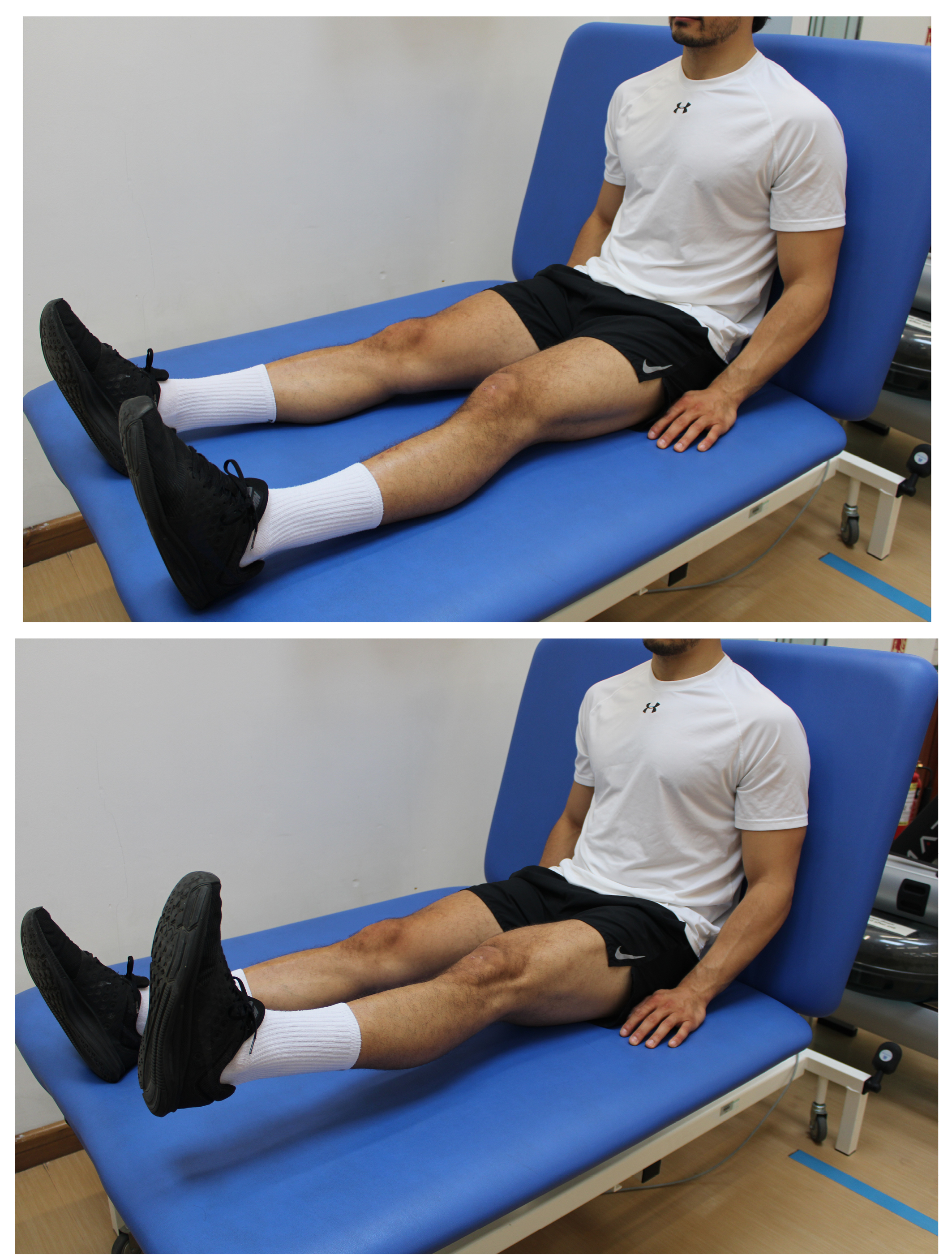
2.Straight leg raises
Sit with your legs straight out in front of you.
Tighten your thigh muscle, and with a straight leg lift as shown in the picture. Try and lift your heel above your hip.
Slowly lower your leg back down. You can either do this exercise lying flat or sitting upright as the picture shows.
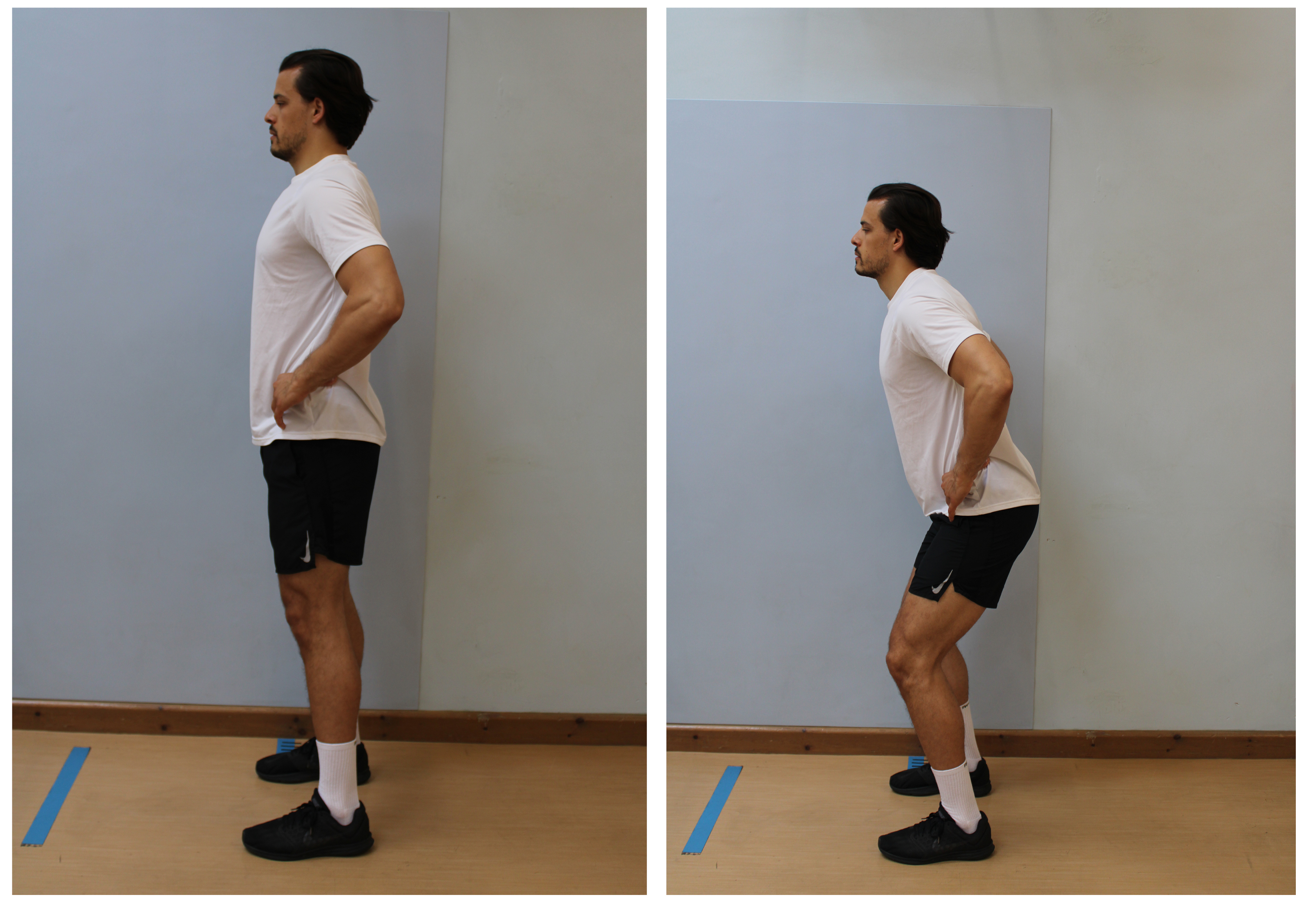
3.Quarter squat
Stand with your feet shoulder width apart.
Place your hands on your hips and keep your chest upright.
Slowly bend your knees a little. Return to the starting position.

4.Step ups
Leading with your injured leg, step up onto the step in a controlled manner. Try not to pull yourself up with your hands.
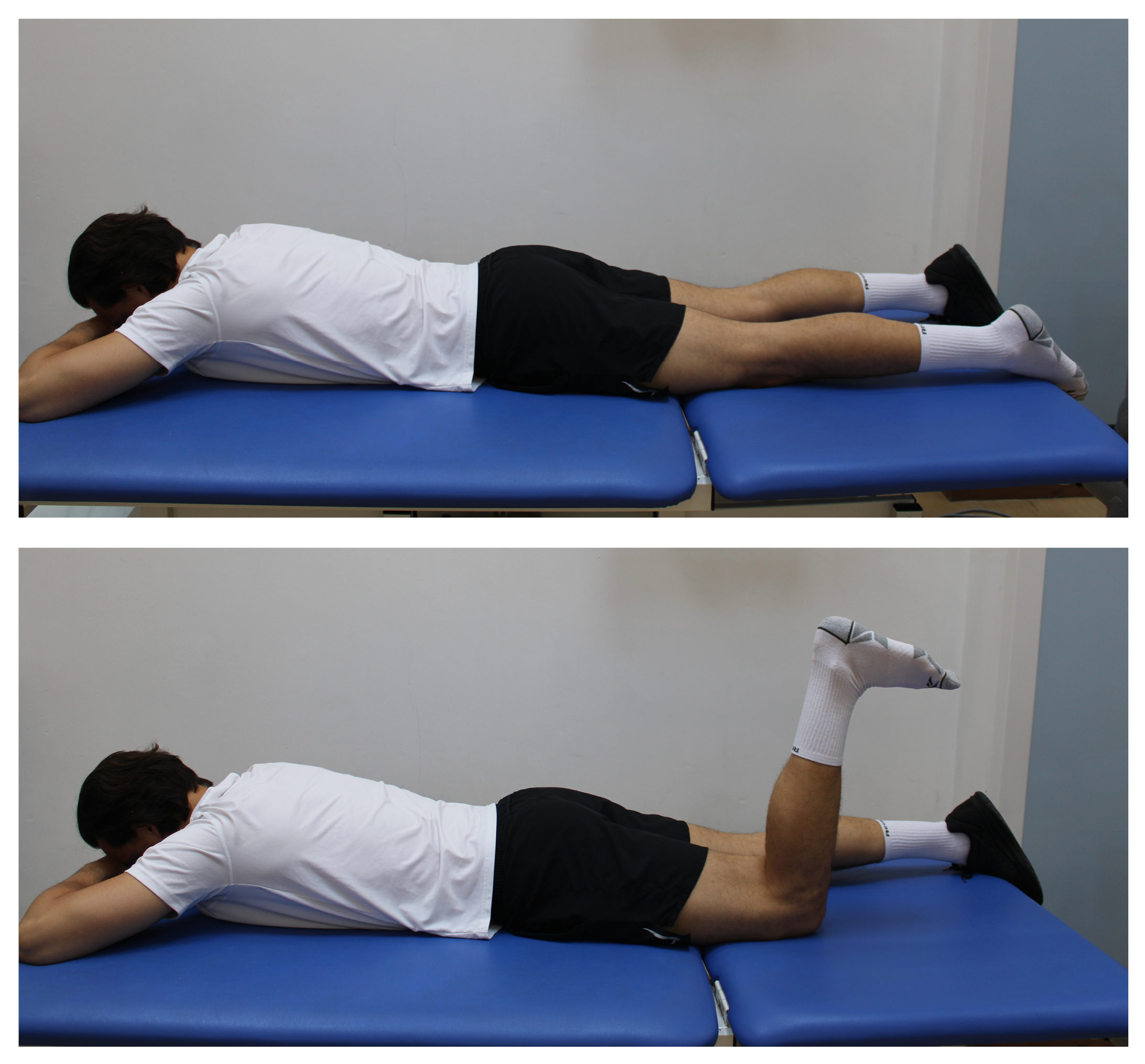
5.Hamstring curl
Lie on your front, with your head resting on your hands.
Bend your knee.
Slowly lower your leg back down.
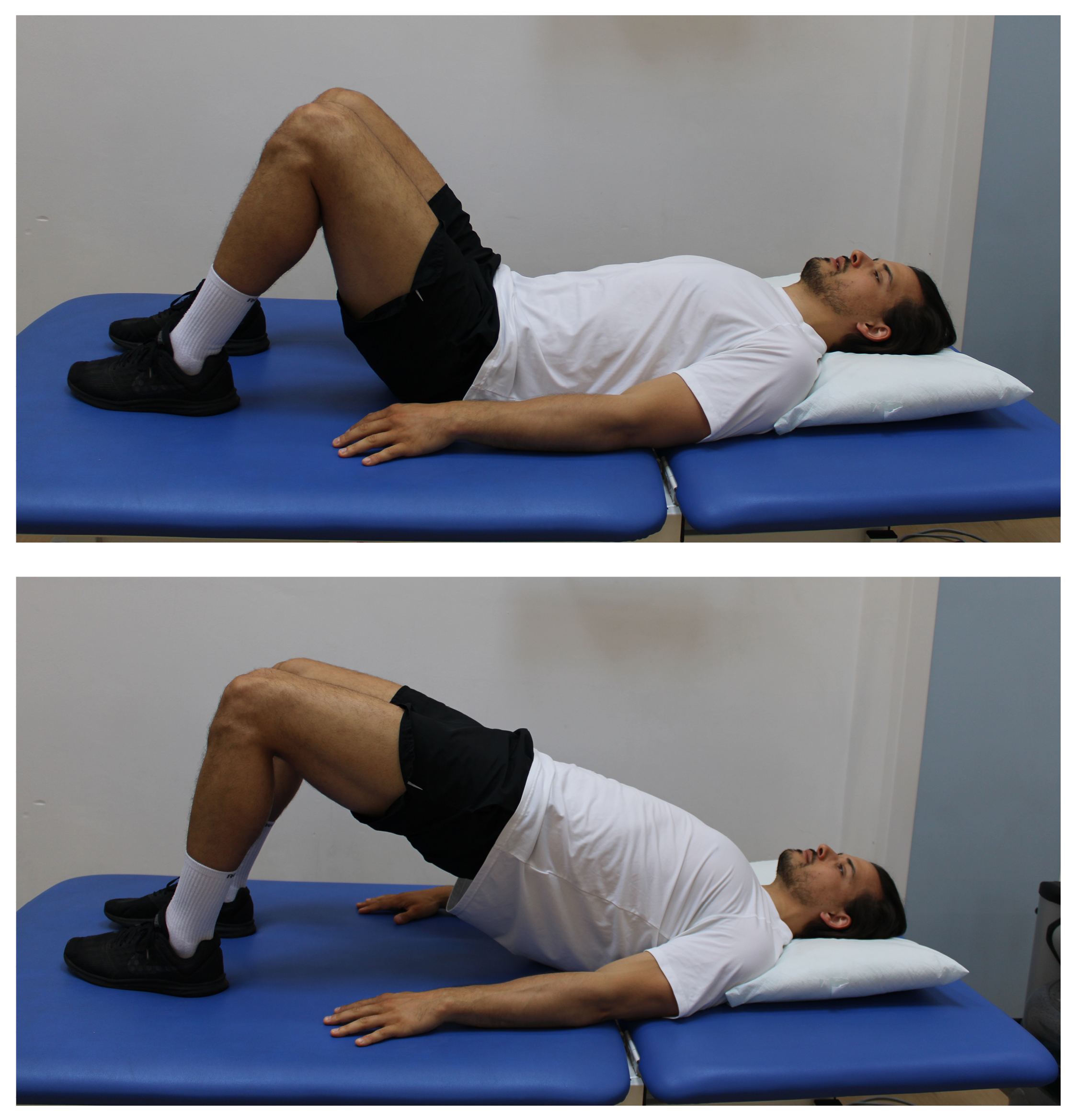
6.Bridge
Lie on your back with your knees bent.
Squeeze your bottom and lift up and slowly lower down.
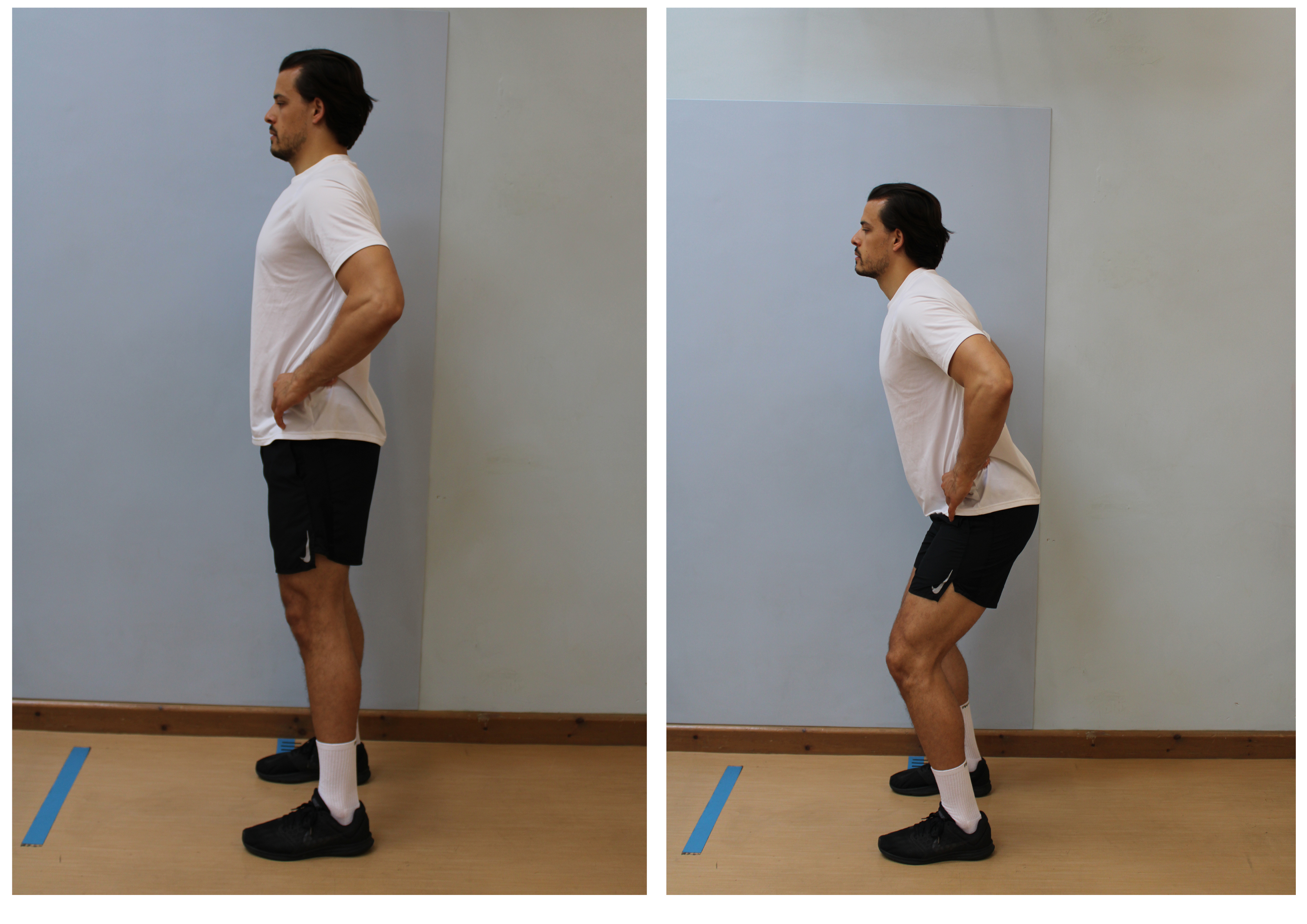
7.Romanian deadlift
Stand with your feet hips width apart.
Keep your back straight, bend at your hips until you feel the backs of your thighs tighten.
Return to start position.
To progress with this exercise, add a small weight and increase as able.
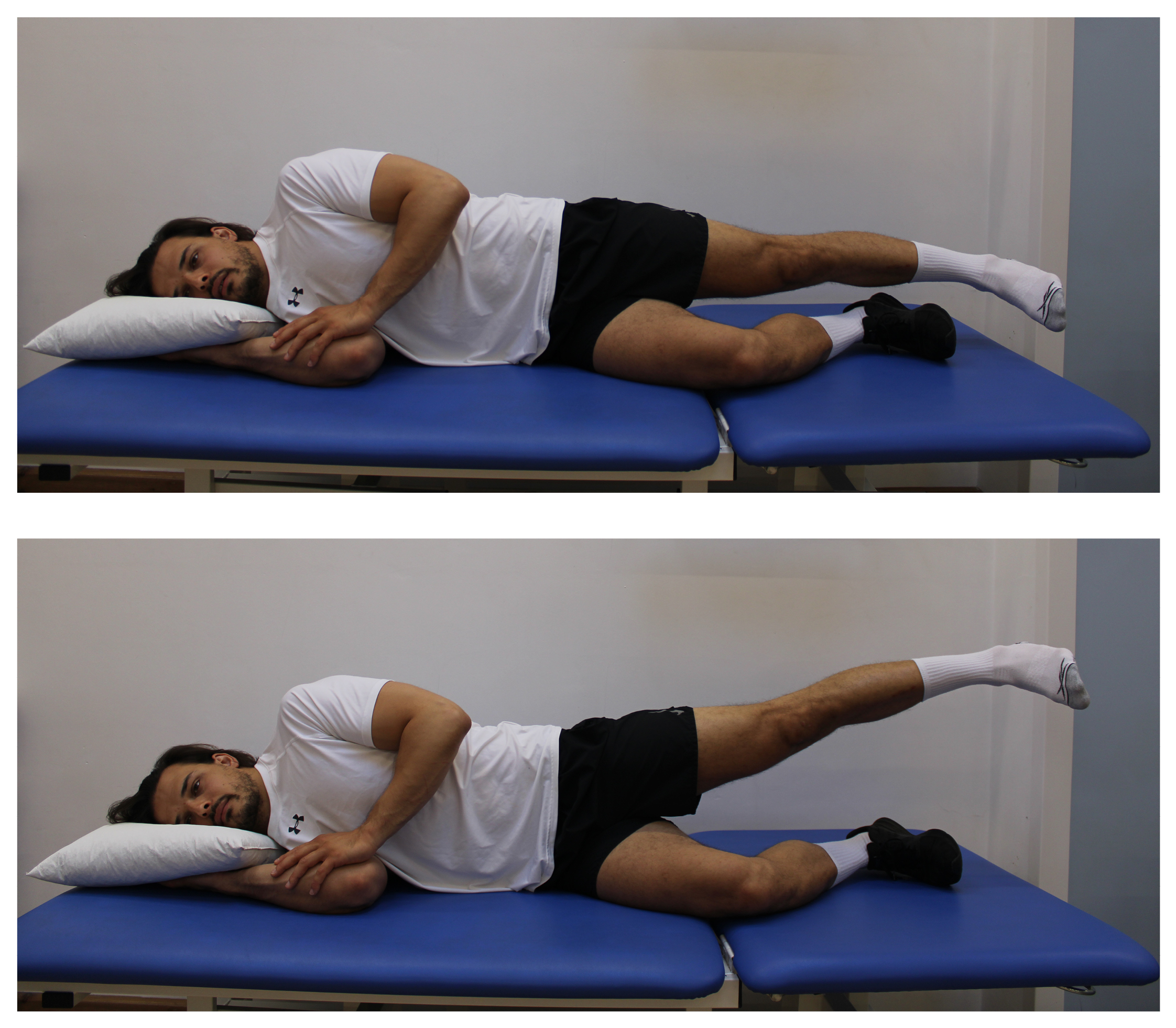
8.Side lying leg lifting (hip abduction)
Lie on your side, keep your leg straight.
Lift up to the side approximately 5cm.
Return to start position.
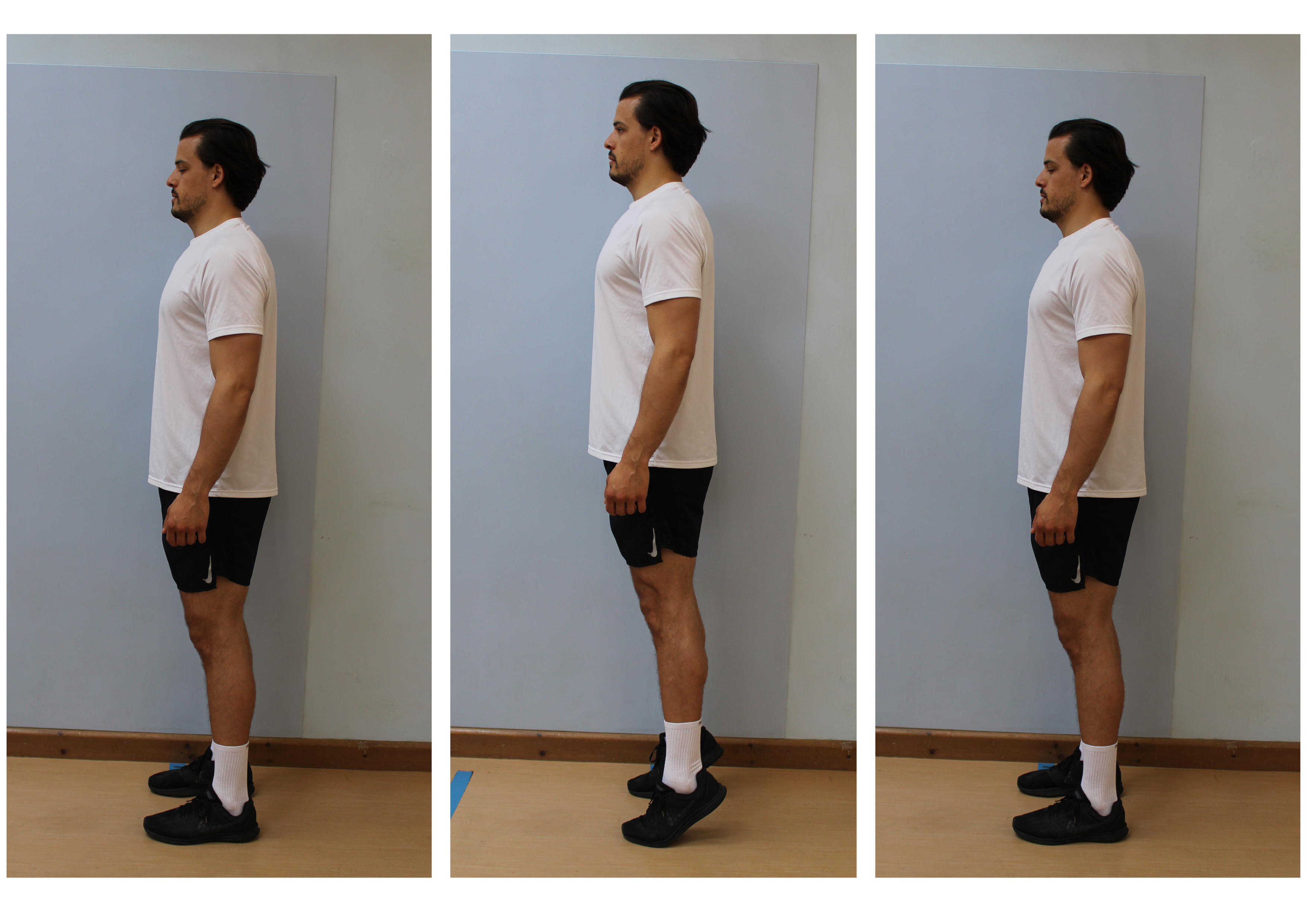
9.Heel raise
Stand with your feet hip width apart.
Push up and down on to your toes.
10.Single leg balance
Stand on one leg.
Use the least support needed to keep your balance.
Hold for 30 seconds, and return your foot to the ground.

11.Cardiovascular exercise
Alongside the above exercises, when you have enough range of motion, you can start some light cycling on a static bike.
Start off with 5 minutes at an easy pace and aim to build up slowly as your fitness and knee allows.
You could also use a cross trainer or go swimming.
What happens during ACL reconstructive surgery?
Surgery may be recommended if, after your best efforts with rehabilitation your knee continues to give way, feels unstable, or you are unable to return to your normal activities. You may also have other symptoms from other injuries such as pain and recurrent swelling, or locking or catching of your knee. If this is the case, surgery may help.
The second half of this booklet explains ACL surgery, and guides you through the rehabilitation needed after your surgery. Although surgery may be recommended, it is your choice whether to proceed with surgery. Remember you can withdraw your consent for treatment at any time.
What is ACL reconstructive surgery?
ACL surgery is a keyhole procedure known as an arthroscopy. It is usually performed as a day case under a general anaesthetic (you are asleep for the procedure).
Two small incisions (cuts) are made just below and either side of the knee cap. In most operations, the ligament needs to be re-built (reconstructed) as only a small number are suitable for repair. For the ligament to be reconstructed, a graft is needed. This graft can either be a tendon that is taken from yourself (known as an autograft) or someone else (known as an allograft).
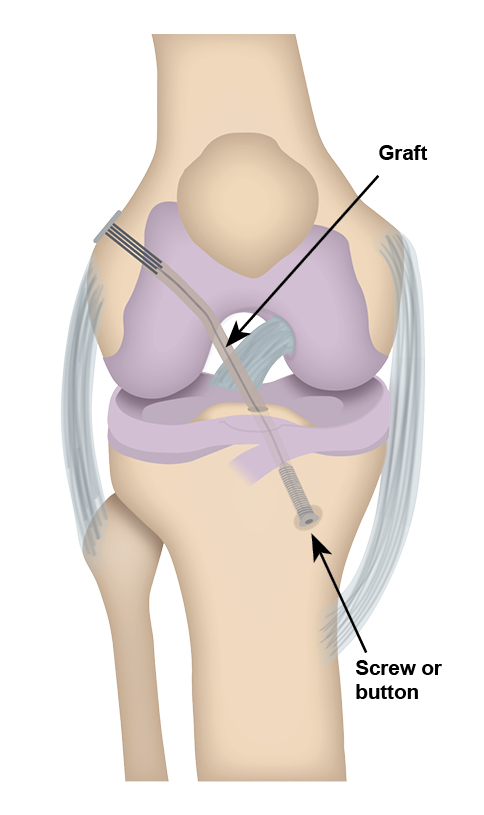
Most ACL reconstructive surgery is done using an autograft, so another incision will be made either on the same leg, the opposite leg, or both. If using an autograft, this can either be from your hamstring on your injured leg or your opposite leg. Or your surgeon may choose to use a patella graft, which is from the front of your knee. The graft is then threaded through the tibia (shin bone) and up into the thigh bone (femur) through the middle of your knee (as shown in the diagram). It is secured in place with either an absorbable or non-absorbable screw in the shin bone and a button or screw on the thigh bone.
How successful is ACL reconstructive surgery?
Just over nine in every 10 patients (90%) will have a good result from ACL surgery.
Between seven and nine in every 10 patients (73% to 83%) will be able to return to sports following their ACL reconstructive surgery.
Five to seven in every 10 patients (50% to 65%) will get back to the fitness level they were at before their surgery (their pre-injury level).
How long does it take to recover from ACL reconstructive surgery?
Recovery after having ACL reconstructive surgery depends on a number of things, including the following.
Your age. Unfortunately, the older you are the longer it can take to recover.
How long ago you injured your knee and whether you have had any physiotherapy to strengthen your leg before surgery.
Whether you have damaged any other structures in your knee, (see Can an ACL injury cause other problems? above).
Whether you need to wear a knee brace after surgery or are advised that you cannot put weight through your operated leg while your knee heals (called being ‘non-weight bearing’).
Whether you go to your physiotherapy appointments and compete the exercises your physiotherapist gives you.
Any complications you have had during or after surgery (see What are the risks of having ACL reconstructive surgery? below). This can also include tendon graft site injuries, for example straining your hamstring after a hamstring tendon graft has been used to reconstruct your ACL.
Your general health, including how healthy your diet is and whether you are a smoker. Quitting smoking is the best thing any patient can do to improve surgical outcomes, please look at the One You Kent web site.
Your rehabilitation after surgery will be guided by the knee surgeon, knee specialist, and a physiotherapist. Your return to sport will be determined by the factors listed above, and whether you engage in your physiotherapy rehabilitation.
As recommended by your consultants and surgeons, you cannot fully return to sports until at least 12 months after your surgery. Evidence shows that patients have better outcomes if return to sports is delayed beyond 12 months.
What are the risks of having ACL reconstructive surgery?
Risks or complications can happen with any surgery. After ACL surgery there is particular concern with the following types of problems.
Rupture of the graft can happen after ACL reconstructive surgery over a five-year period in five to eight of every 100 reconstructions.
Five in every 100 patients have ongoing instability of their knee after surgery. It can either be due to the graft not healing in a tight enough position, or stretching of the graft if excessive force occurs to the knee in the first few days following surgery (you do too much too early).
Having surgery can increase your risk of developing a deep vein thrombosis (DVT). A DVT is a blood clot which forms within a deep vein, usually in your legs. The blood clot can cause the leg to become painfully swollen and hot to touch, with skin discolouration. In some cases, part of the blood clot breaks off and becomes lodged in a blood vessel in the lungs. This is known as a pulmonary embolism (PE) and can cause symptoms including shortness of breath, chest pains, and coughing up blood.
Your clinical team will assess your risk of developing a blood clot. You may be prescribed medication, or advised to wear compression stockings to reduce your risk of developing a clot during your hospital stay. When you leave hospital, you may need to continue taking the medication at home; this will be discussed with you on discharge. For more information, ask a member of staff for the Reducing the risk of a blood clot for patients with a leg injury needing immobilisation leaflet.
Deep infection happens to one to two in every 100 patients. Precautions are taken during surgery to reduce this risk. However if you did develop a deep infection, you would need to return to hospital for a washout of your wound / joint. If your knee becomes very hot, inflamed, swollen, or yellow pus comes from your wound, please either call 111 or go to your nearest Emergency Department.
Knee stiffness can develop in two to five in every 100 patients, due to scar tissue within the knee. Some people are more likely to develop a lot of thick scar tissue. This can be treated with a surgical cut of the scar tissue.
Swelling is common for up to the three months following surgery. It can be treated with ice therapy and compression. However, if the swelling continues it may mean that you have ongoing problems within your knee and may need further investigations.
Patella (knee-cap) pain or discomfort can happen to two in every 10 patients who have had a bone-patella-bone graft compared to a hamstring graft. This normally happens when the patient squats or kneels down. This can usually be treated with physiotherapy, but it can be prevented if you follow the rehabilitation exercises you have been given.
Nerve damage is common following ACL surgery. Symptoms include numbness around your scar and in your leg. This may last a few months or continue for longer. It should not stop your leg working properly.
Sometimes the graft that is taken from your injured leg for the reconstruction does not work. If this is the case, a graft may be taken from your other leg during surgery.
If you have concerns about any of the risks listed above, please speak to your surgeon.
What should I do after ACL surgery?
Following your surgery you will be given elbow crutches to help you walk, and your surgeon will tell you whether you are allowed to:
fully weight bear (put normal weight through your operated leg); or
partial weight bear (only put a certain amount of weight through your operated leg); or
non-weight bear (not be allowed to put any weight through your operated leg) for a period of time; or
whether you have to wear a brace, and how long you must wear the brace for, which may limit how much you can bend or straighten your knee.
You must follow your surgeon’s guidance.
You will be seen by a physiotherapist on the ward, who will make sure you are able to walk safely with your elbow crutches. For further information on how to use your crutches, please ask a member of staff for a copy of the Trust’s Using crutches leaflet.
You must ice your operated knee daily to reduce the swelling, this will help you to regain full movement in your knee. For further information, please ask a member of staff for a copy of the Trust’s Ice treatment leaflet.
Will I have a follow-up appointment?
You should be given an outpatient physiotherapy appointment within two weeks of your surgery. If not, please contact the Physiotherapy Central Booking Office on 01227 783065.
You will have an appointment with a physiotherapist to review your knee and progress your exercises after surgery. During this appointment you will be offered the chance to either join a specialist ACL rehabilitation class which is run by physiotherapists, or if you are unable or not keen on attending the class you can have on-going 1:1 appointments with a physiotherapist instead.
You will also have a follow-up appointment with your consultant or knee specialist. If you do not have an appointment booked after surgery, please contact the relevant Fracture Clinic (their contact details are on the final page of this booklet).
When can I start my exercises after surgery?
You must start the exercises marked Phase 1 below before your physiotherapy appointment. These exercises are safe to do.
Please note, if you have been given a brace to wear or are have been told that you cannot put full weight through your operated leg, you cannot complete all the exercises in Phase 1.
The following exercises are designed to help you regain full range of movement, and maintain good blood flow in your legs following your surgery.
Start gently, increasing the stretch a little each time.
Aim to practice each exercise two to three times a day (set), with eight to 12 repetitions (reps) each time; rest for 60 to 120 seconds between each set (rather than doing one set in the morning, one at lunch, and one in the evening).
Aim to practice each exercise at least three days a week, but no more than five days.
Please stick to the time frames given, unless told otherwise.
Phase 1: week 0 to week 2 after surgery
You may be given and advised to wear a brace after your ACL surgery. The brace will limit how far you can bend or straighten your knee. If you have been given a brace after ACL surgery, please only do the following four exercises until you have seen your physiotherapist.
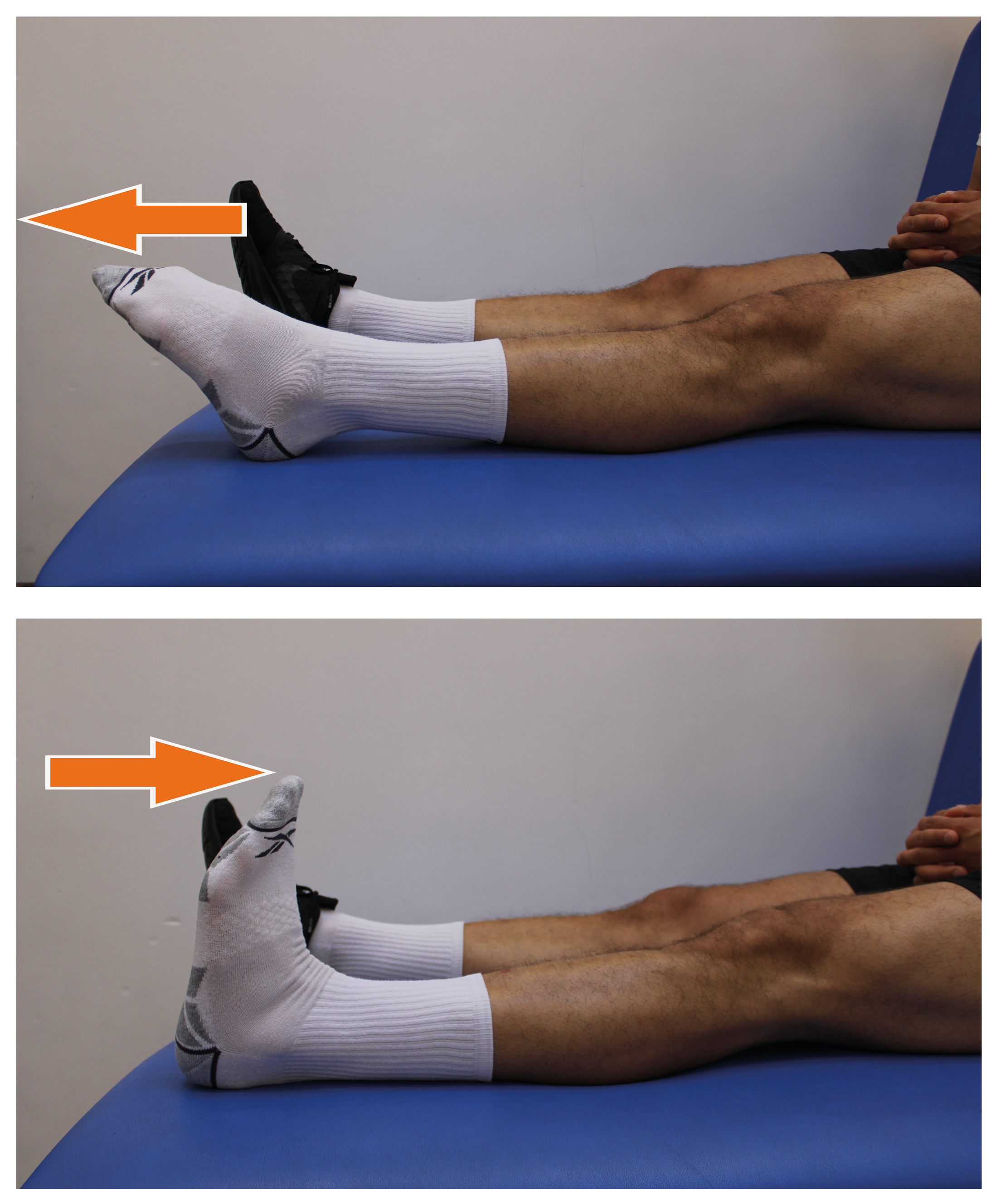
1.Ankle pumps
Sitting or lying down, quickly bend and straighten your ankles.
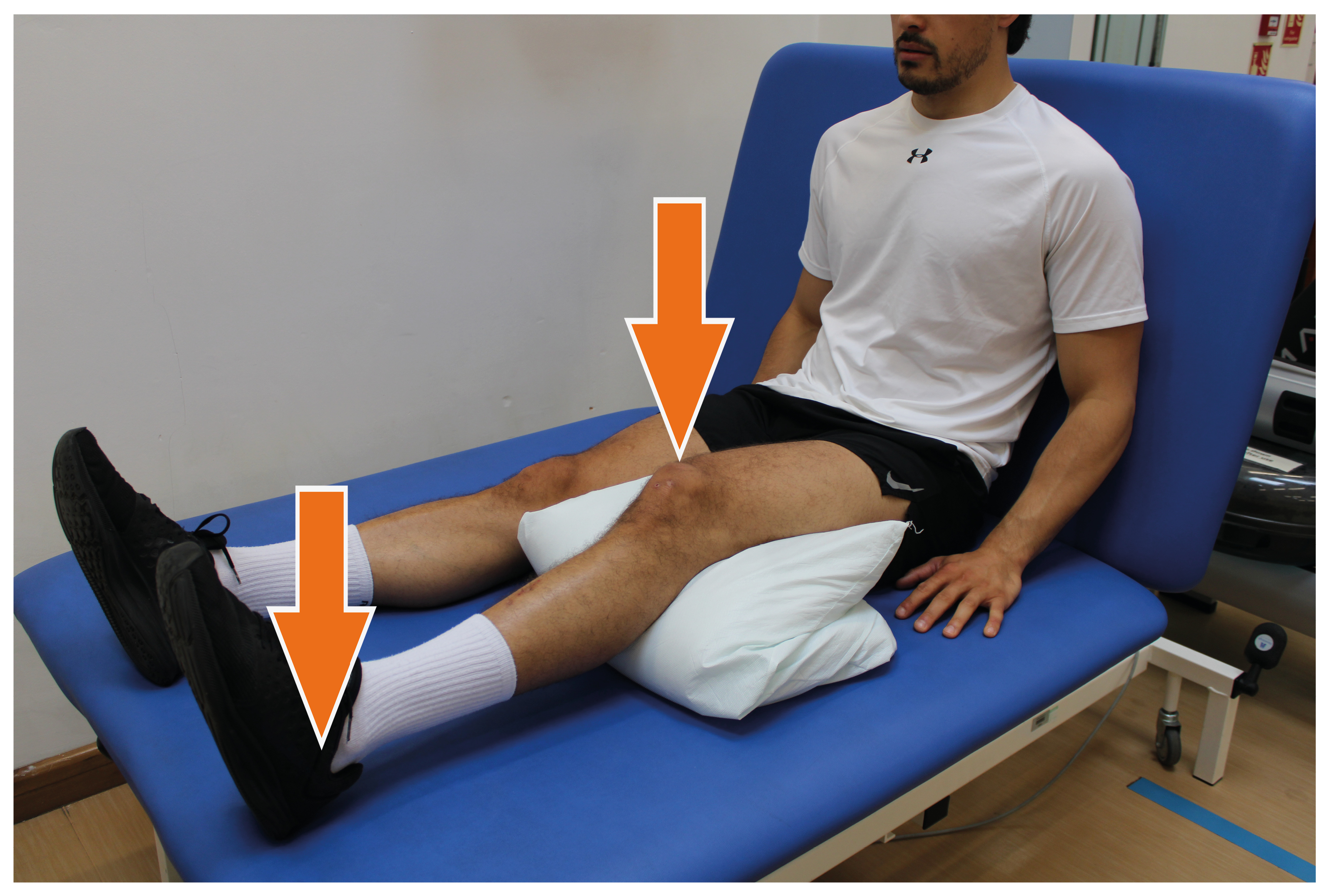
2.Quadricep (quads) and hamstring co-contraction (contracting the quadriceps (front thigh muscles) and the hamstrings (muscles at the back of the thigh) at the same time).
Bend your knee over a pillow or rolled-up towel.
Push your heel into the floor, and push your knee down into the pillow. Keep the pressure on the heel. Do not move your knee.
Hold for 5 seconds.
Repeat 10 times.
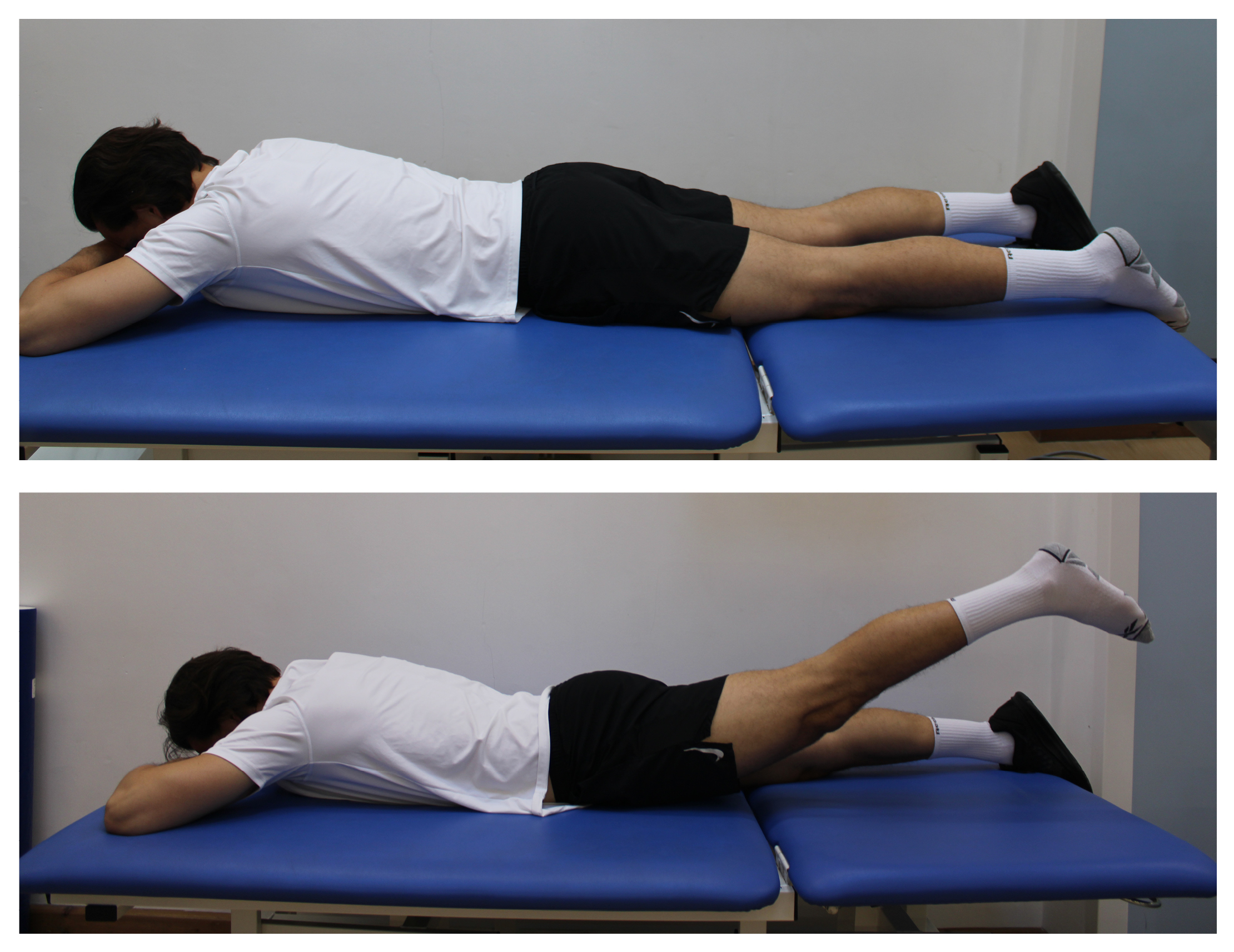
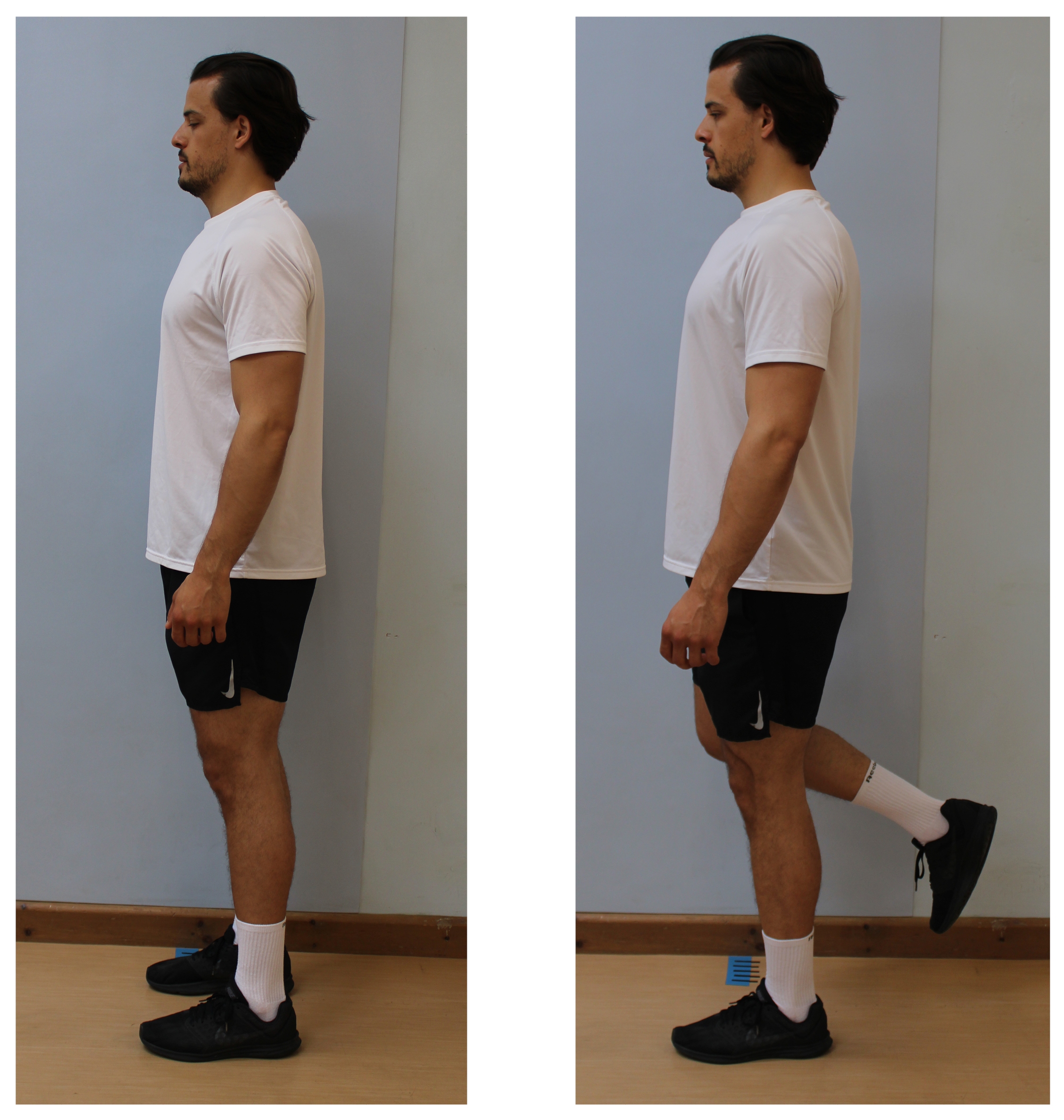
3.Prone hip extension
Lay on your front, with your head supported on your arms or a pillow.
Lift your leg up towards the ceiling.
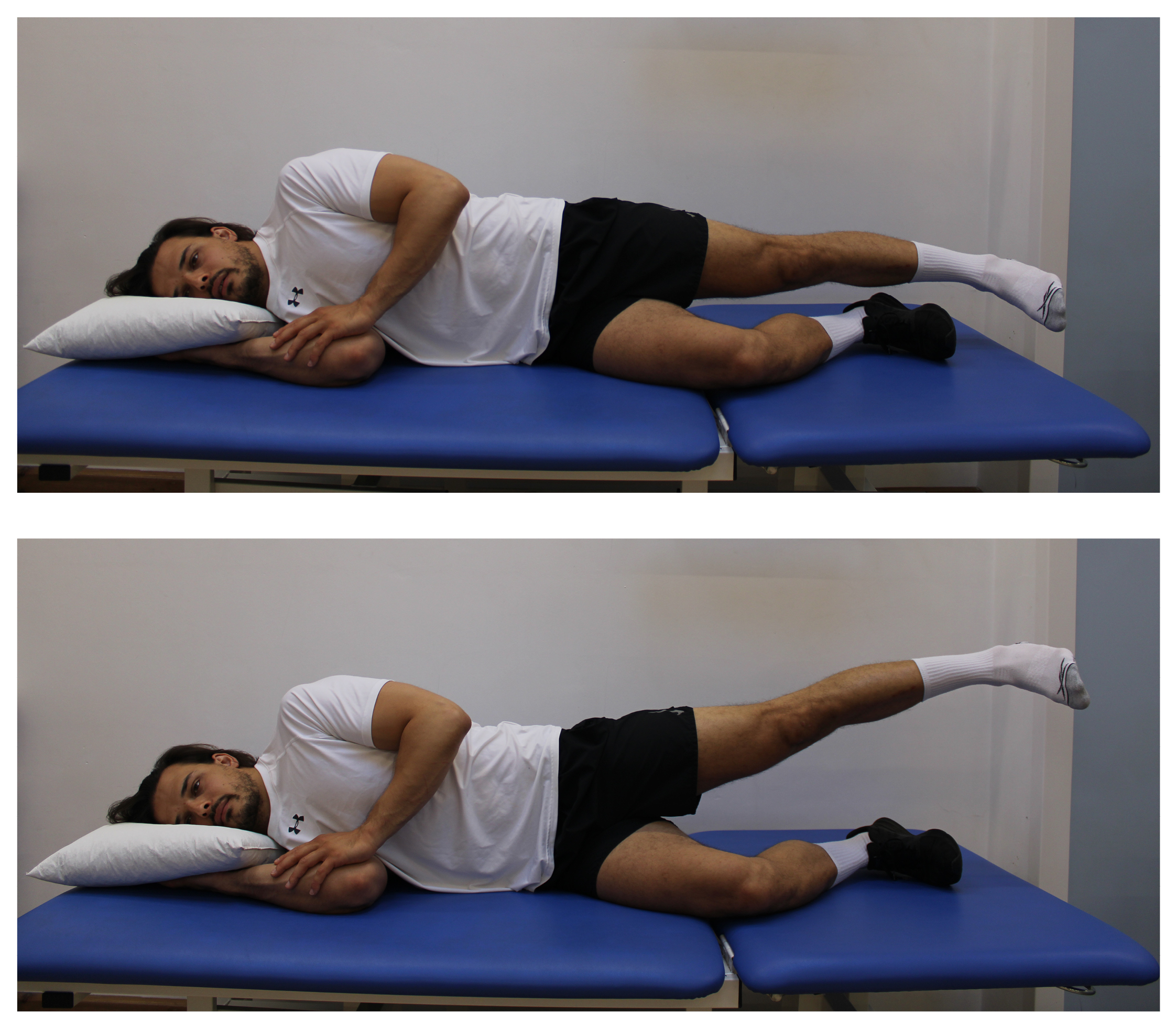
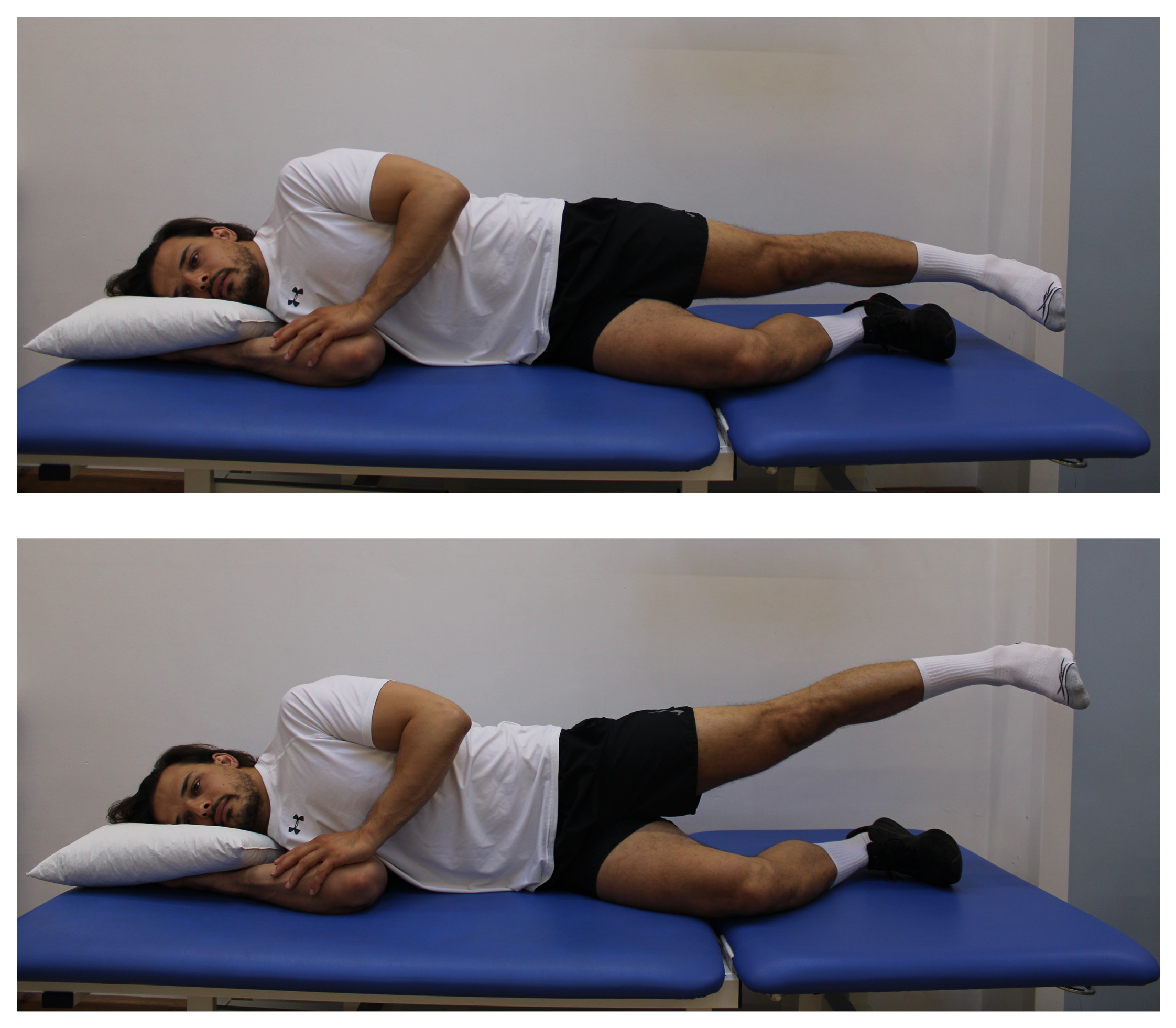
4.Side lying abduction
Lay on your side, keeping your injured leg straight. Bend your uninjured leg.
Lift your injured leg up to the side by approximately 5cm.
Lower your leg to your start position.
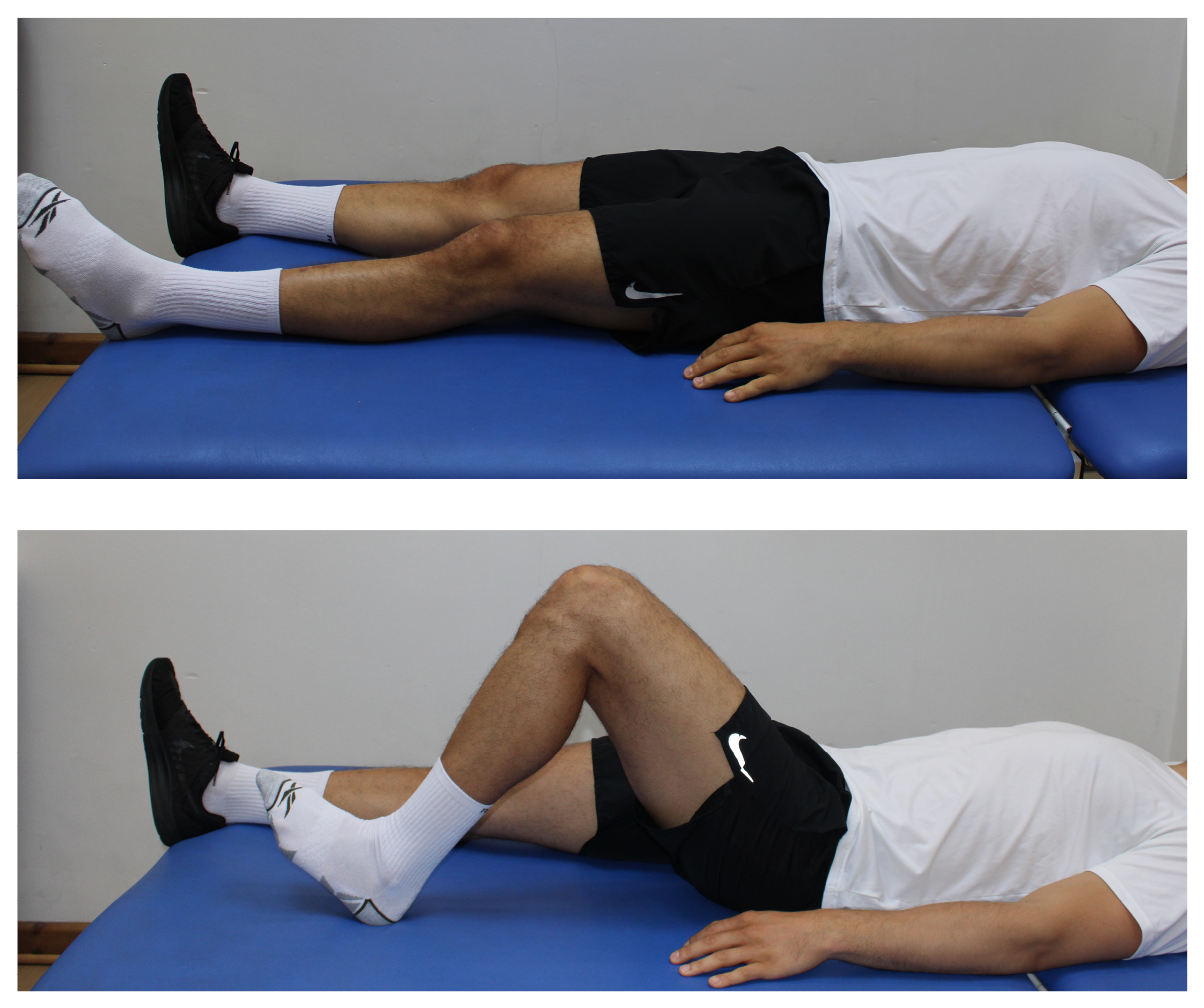
5.Heel slides
Only do this exercise if you are not wearing a brace and have been told that you can fully weight bear after surgery.
Lay on your back.
Gently slide your heel up and down the bed or floor, bending and straightening your knee.
If you are not wearing a brace and are allowed to fully weight bear through your operated leg after surgery, please also complete the next four exercises.
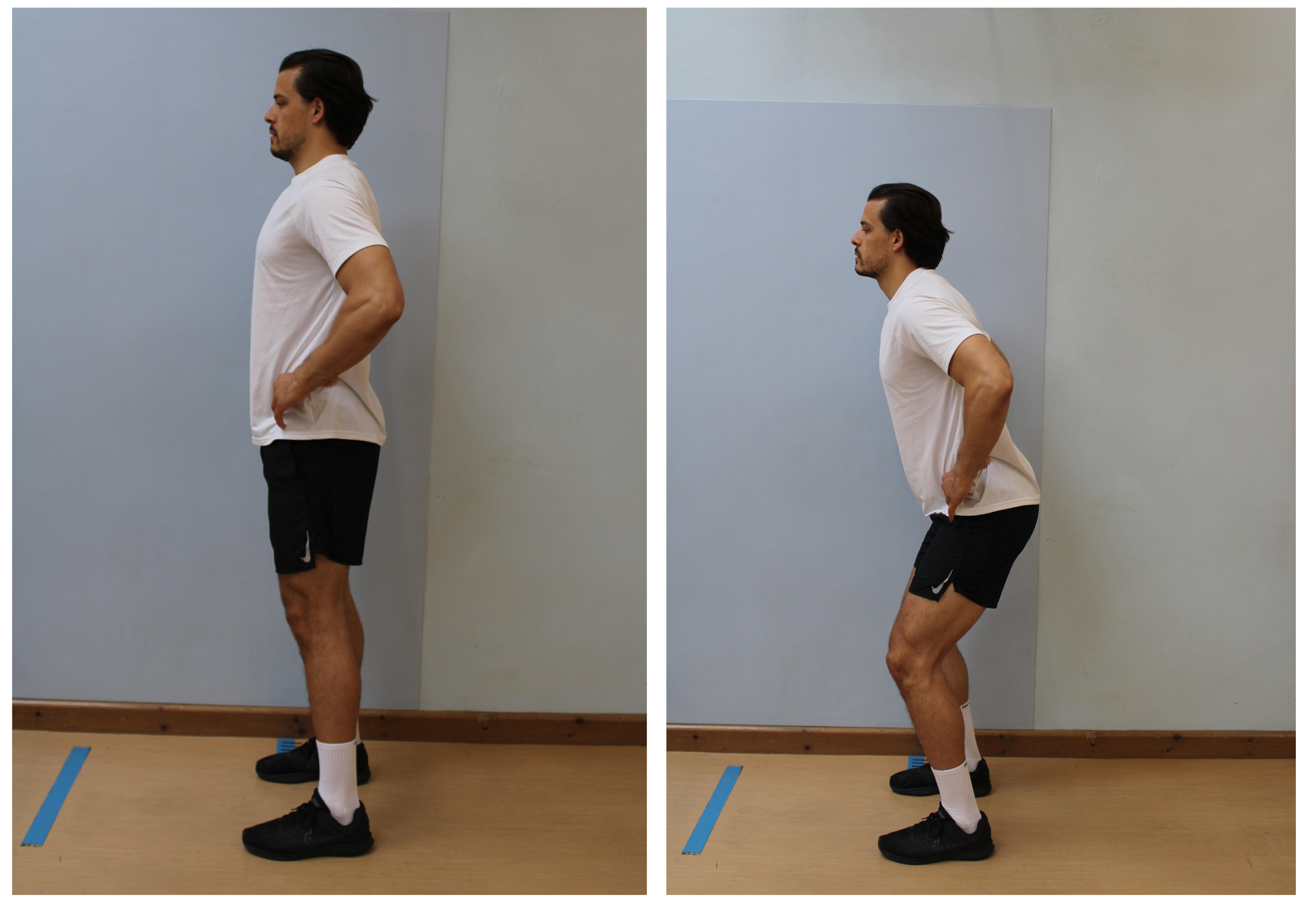
1.Quarter squat
Only do this exercise if you are not wearing a brace and have been told that you can fully weight bear after surgery.
Stand with your feet shoulder width apart.
Place your hands on your hips, keep your chest upright.
Slowly bend your knees a little.
Return to your start position.
2a. Heel raise
Only do this exercise if you are not wearing a brace and have been told that you can fully weight bear after surgery.
Stand with your feet hip width apart.
Push up and down on to your toes
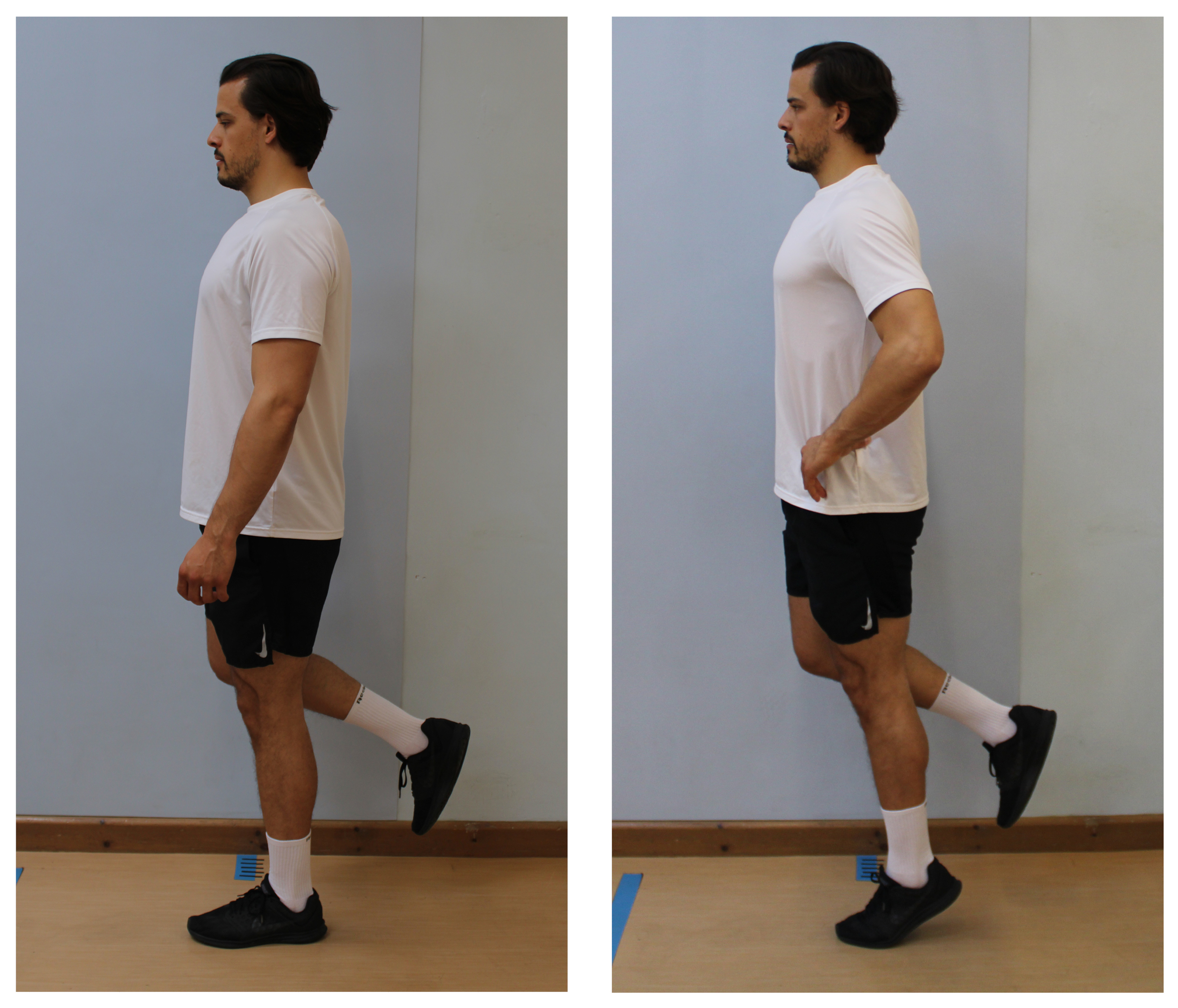
2b. Single-leg heel raise: progression
Stand on one leg.
Use the least support needed to keep your balance.
Hold for 30 seconds, then lower your leg to the floor.
When this exercise becomes easy, progress to doing it balancing on one leg.
3.One leg stand
Only do this exercise if you are not wearing a brace and have been told that you can fully weight bear after surgery.
Stand on one leg.
Use the least support needed to keep your balance.
Hold for 30 seconds, then lower your leg to the floor.
Phase 2 (on average 2 to 6 weeks after surgery)
Your physiotherapist will tell you when you can start the following exercises. Please do not start these exercises before seeing your physiotherapist.
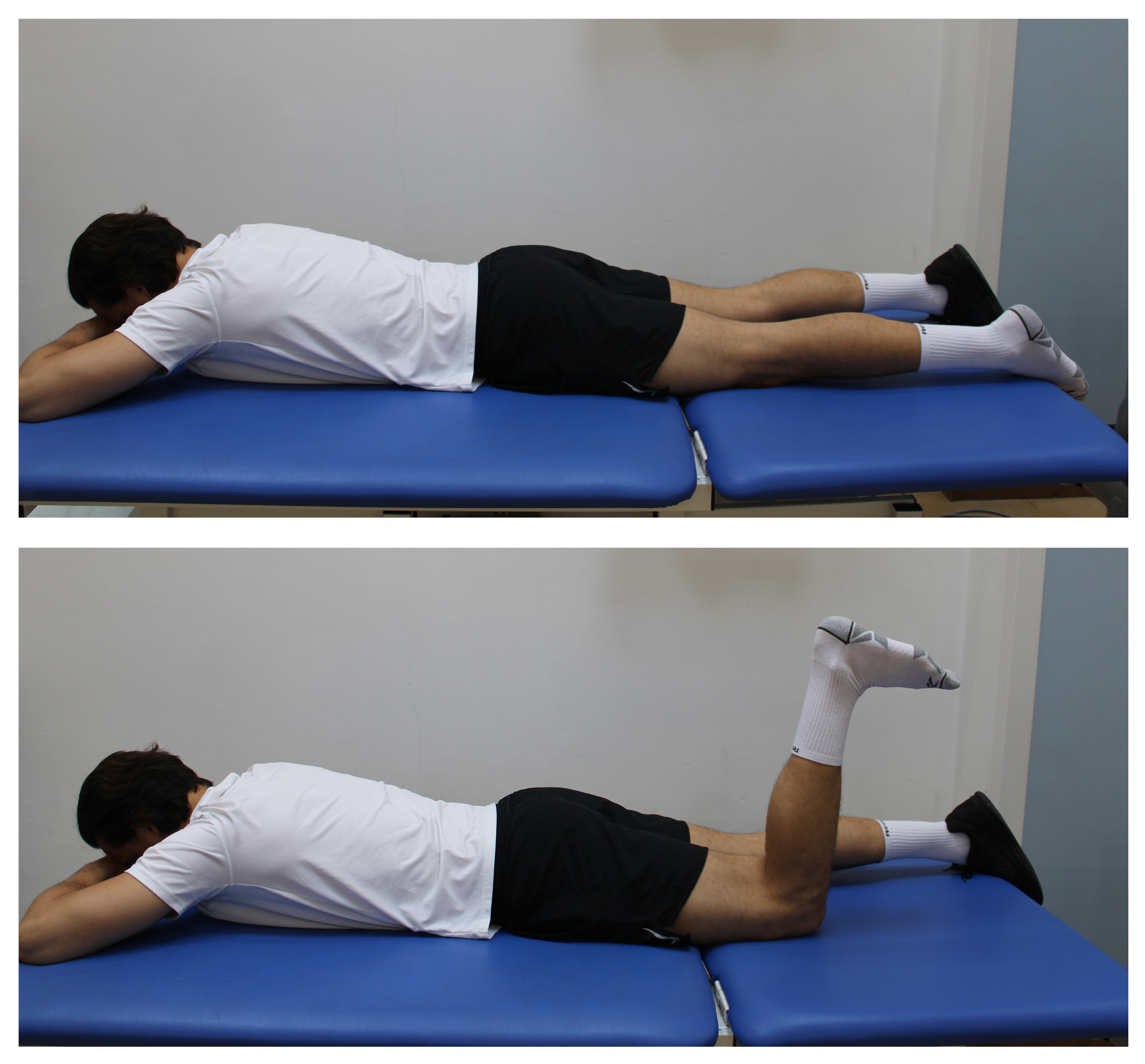
1.Hamstring curl
Lie on your front, with your head resting on your hands.
Bend you knee.
Slowly lower back down.
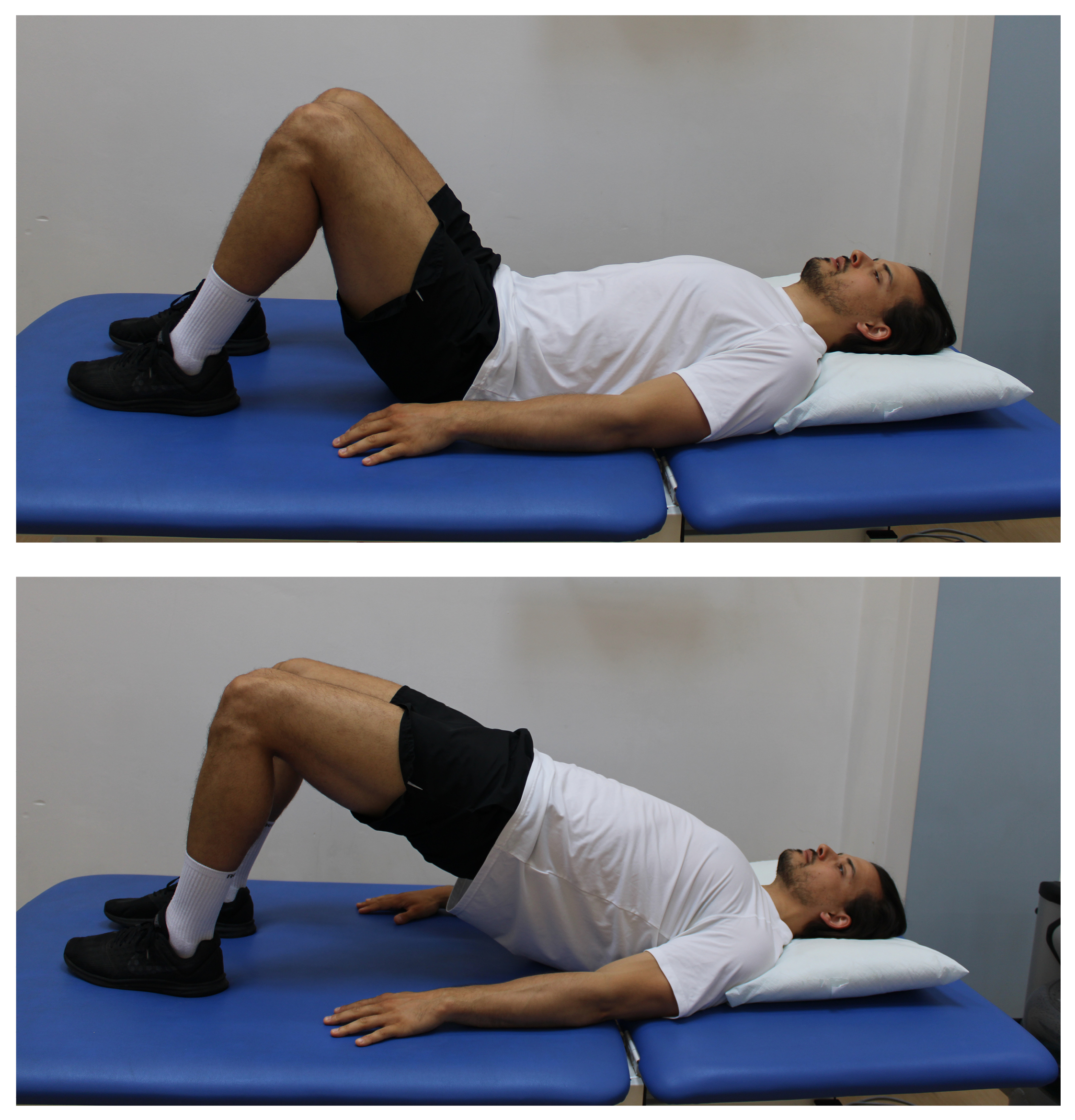
2.Bridge
Lie on your back with your knees bent.
Squeeze your bottom and lift up and slowly lower down.
When this exercise becomes easy, progress to using one leg only.
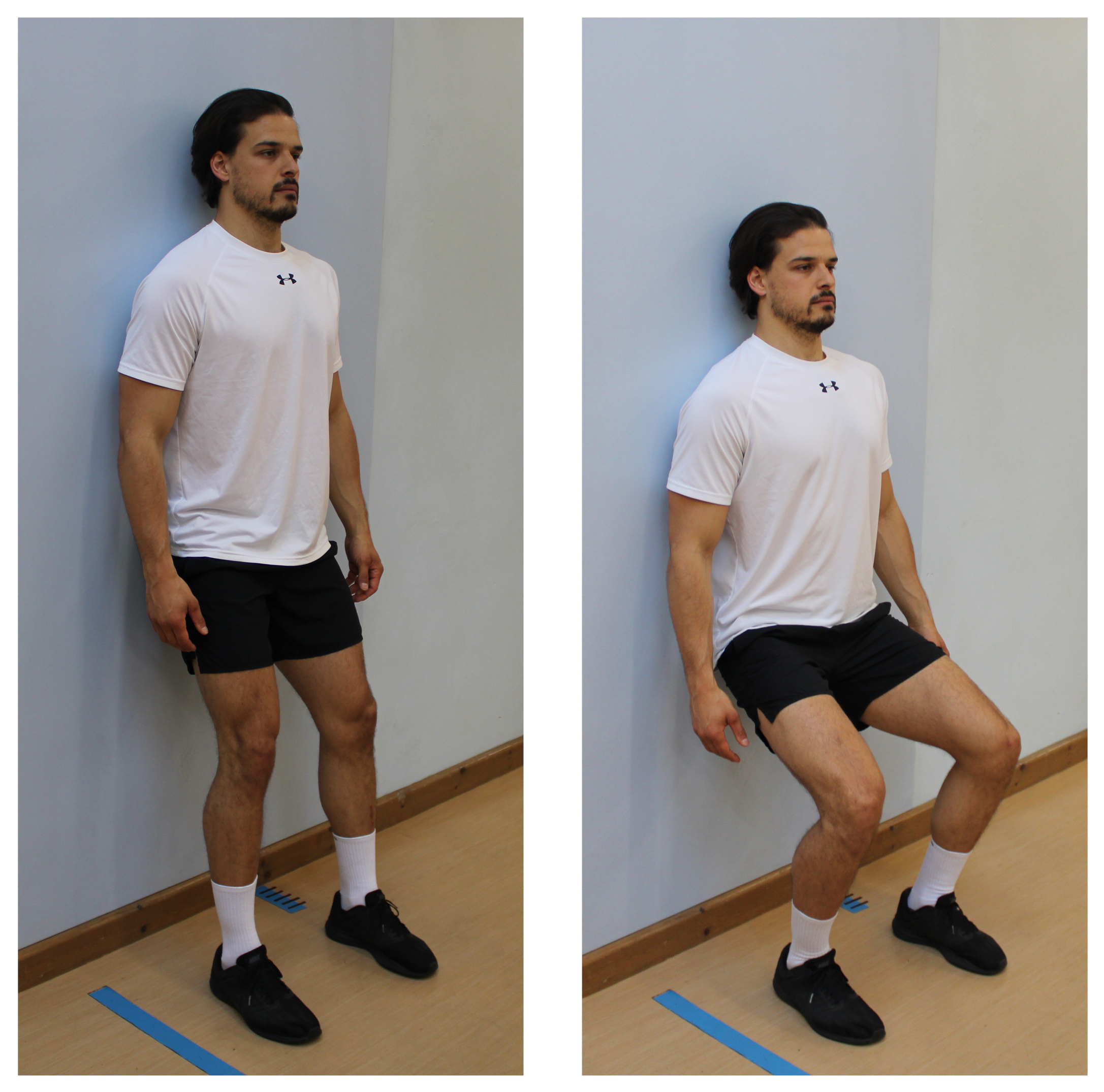
3.Wall squats
Stand leaning against a wall.
Slide down the wall, keeping your heels on the floor.
Push yourself back up to your starting point.

4.Step ups
Step up and down on one step
Useful contact details
If you wish to cancel or change your physiotherapy appointment, or you have any urgent concerns about your physiotherapy rehabilitation, please contact:
Physiotherapy Central Booking Office
Telephone: 01227 783065You can change or cancel your appointment with your surgeon or knee specialist, by clicking on the QR code or:
Telephone: 01227 868686
WebYou can contact the Physiotherapy team by email if you have any other concerns or questions regarding your rehabilitation. Please note that this email account is not checked over the weekend or on public holidays and it may take 24 to 48 hours to get a reply.