Age-related Macular Degeneration (AMD)
Information for patients from Ophthalmology
What is Age-related Macular Degeneration (AMD)?
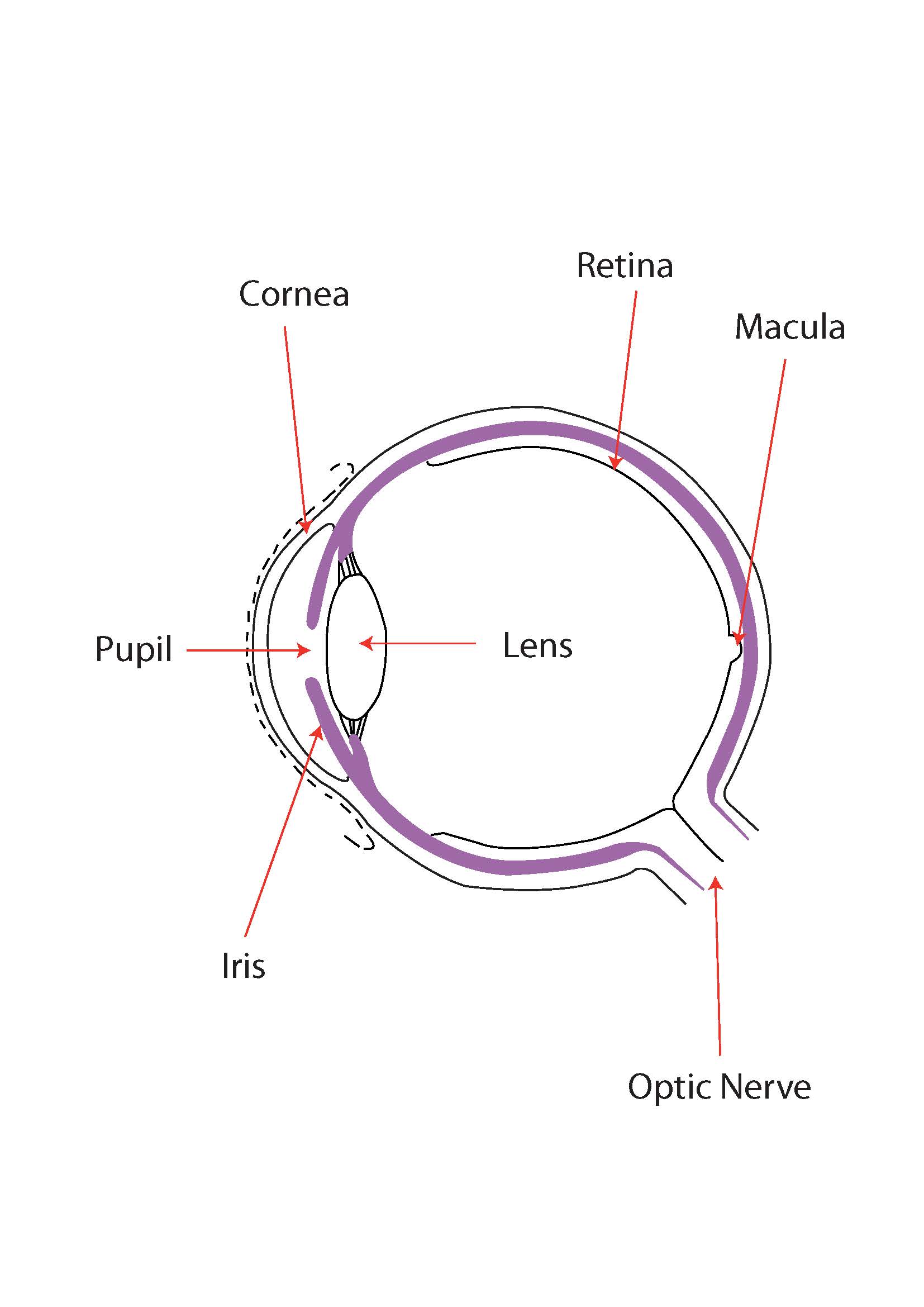
The eye has often been compared to a camera, with the retina being the film which captures the image.
The macular is the centre most point of the retina, where the light comes into focus when you are looking at an object. If the macular area is damaged, you will probably see a blurred spot at the centre of your vision. This is known as macular degeneration and can cause certain tasks, such as reading, to become more difficult.
What causes Age-related Macular Degeneration?
In most cases there is no known cause. It is more common in older people though, and is therefore referred to as Age-related Macular Degeneration.
It is possible for macular degeneration to be hereditary, and it can affect younger people. This is usually known as macular dystrophy.
What are the types of Age-related Macular Degeneration?
There are two types of Age-related Macular Degeneration.
Dry is the most common type of macular degeneration. It is caused by slowchanges to the macula over many years. In most cases, some useful vision (eyesight) is kept throughout life.
Wet is the less common type of macular degeneration. It is usually caused by abnormal blood vessels under the retina, which bleed and leak causing sudden loss of vision.
What is the treatment?
Treatment depends on the type of macular degeneration you have.
Unfortunately, in the case of dry macular degeneration there is no treatment. There is some evidence to suggest that eating fish, fruit, and vegetables (such as broccoli, spinach, and carrots), and not smoking could help. In advanced dry AMD, high doses of vitamins (AREDS (Age Related Eye Disease Study) preparations) have been shown to reduce the rate of progression.
Wet AMD can be treated by injections given within the eye, of drugs that reduce the leakage and stop the progression of the disease. To begin with we recommend three injections a month, however based on four to eight weekly assessments more treatments may be needed for up to two years.
What risks are linked to having the injection?
Complications include inflammation and raised pressure in the eye. More rarely you may develop an infection, a retinal detachment, or bleeding.
Any of these complications can result in loss of vision.
What do I do after my injection?
After your injection, lubricating drops will be put in your eye. If your eye feels uncomfortable following your injection, you will be given drops to put into your injected eye for up to three days.
You may have some blurred vision (often described as ‘seeing spots floating in the eye’) for up to two weeks following your procedure.
You may feel some discomfort in your injected eye. Taking your usual painkillers may help.
If you have increased blurring, pain, or redness in the few days after your injection, you should contact us.
Ophthalmology Clinic contact details
Monday to Friday 8:30am to 4pm, contact the AMD Co-ordinator at Kent and Canterbury Hospital on telephone 01227 783172.
Or if they are not available, please go to your nearest Emergency Department.
Is there any practical help that may help me cope with my condition?
Yes.
Use large print books for reading.
Use angle poise lamps and brighter bulbs, although you may not be able to tolerate bright light. You may find that photochromatic lenses in your glasses help stop some of the glare.
Magnifiers may be useful; ask at your local Low Vision Aid Clinic.
Try looking at objects from the side of your vision, rather than looking directly at them.
Sit closer to the television; this should not adversely affect your vision.
If your consultant considers your vision to be bad enough, you may be registered as partially sighted or as blind. This may entitle you to additional help, such as rent rebates, a disabled parking permit, reduced television licence fees, and a free radio / cassette player.
It is important to remember that AMD does not lead to total blindness, although your central vision will become increasingly difficult to maintain. Your peripheral vision (side vision) should remain less affected.