Achilles tendon rupture treated with VACOped® Boot: rehabilitation programme and exercises
Information for patients
This booklet is designed to give you an outline of how your rehabilitation will progress as you recover from your Achilles tendon rupture. It is only a guide and can be changed to meet your specific needs.
The following time frame is a guide and may change depending on your individual progress.
If you are fitted into a VACOped® Boot, please contact the Physiotherapy Department on 01227 783065, and give your name, date of birth, and the date of your injury. We will make sure you are appropriately followed-up.
What is an Achilles tendon rupture, and what are the benefits of the VACOped® Boot?
An Achilles tendon rupture is a break of the tendon that is at the back of your ankle and connects the calf with the back of your foot. When that tendon breaks, you cannot push up onto your toes and your walking is affected.
In order to heal the tendon, you need both ends of the tendon to be brought closer together. For that to happen, you need to have your foot pointing down (equinus position) and to have your movement restricted for the first four weeks. After that, you can start moving gently. Wearing the VACOped® Boot can help this to happen more easily.
The treatment with the boot will take about nine to 10 weeks (unless you are told otherwise). However, full recovery can take up to a year, so you need to be aware and sensible about your affected leg, follow the advice from the professionals looking after you, and do not push yourself too much, as there is a risk that your Achilles tendon will re-rupture. Meanwhile, you will be using crutches (at least for the first few weeks).
What do I do if I need help using my crutches?
If you need any help using your crutches, visit the East Kent Hospitals website and see the Using crutches leaflet.
If using crutches causes you pain in your hands, you can put extra padding on the handles (such as a fleece sock) or buy some hand protectors.
How do I safely use the stairs while having a cast on or wearing my boot?
Using stairs while non-weight bearing / wearing a cast is not advised due to health and safety risks, unless you have been shown how to by one of the hospital’s physiotherapists.
-
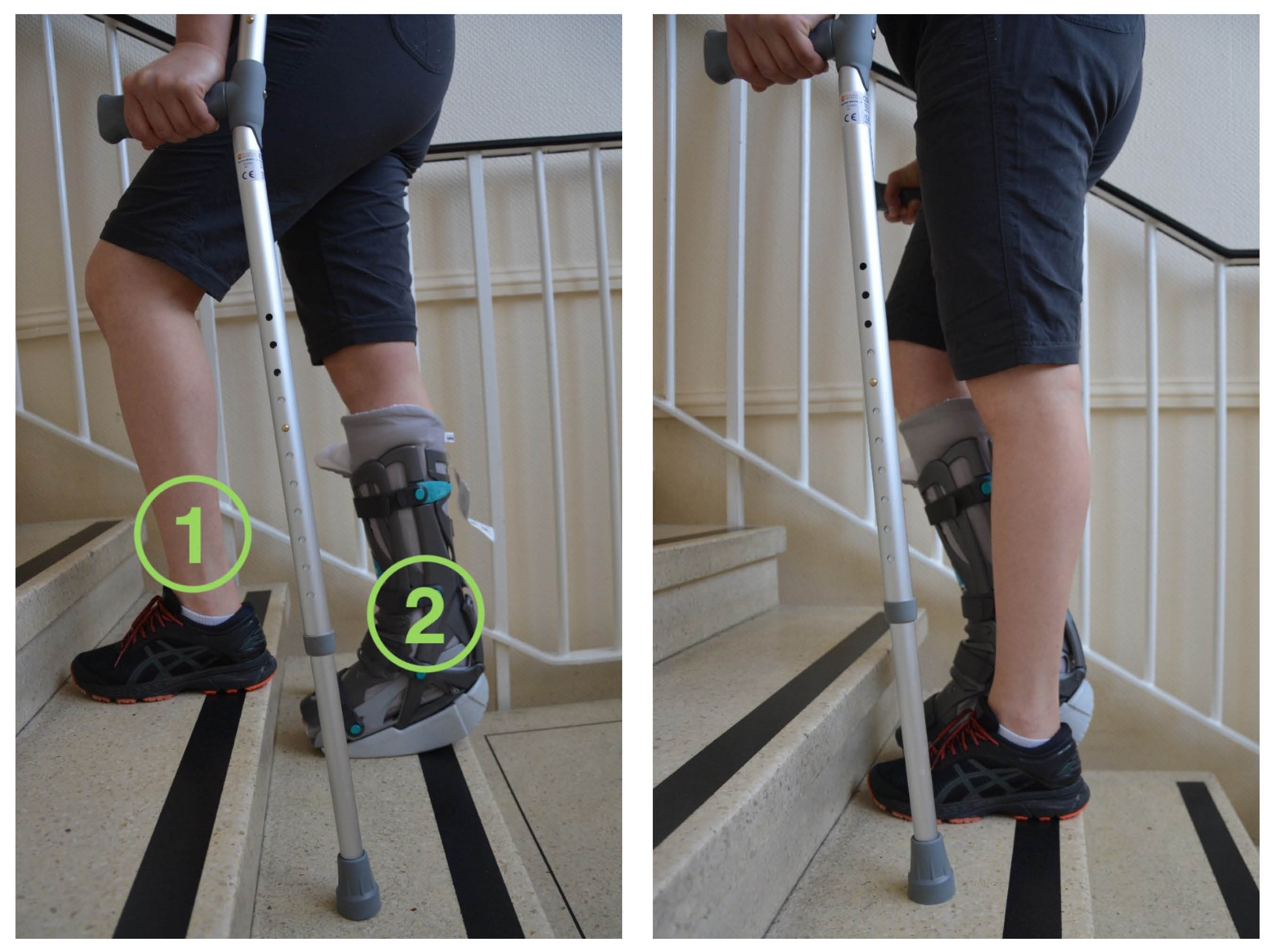 When going up the stairs, start with your non-affected leg first (1), follow with the affected leg (2) and then the crutches.
When going up the stairs, start with your non-affected leg first (1), follow with the affected leg (2) and then the crutches. -
 When going down the stairs, you should first put the crutches down, then your affected leg (1) and finally your non-affected leg (2).
When going down the stairs, you should first put the crutches down, then your affected leg (1) and finally your non-affected leg (2).
Why are exercises important while I am wearing my boot?
It is very important to keep moving ‘little and often’ whilst wearing your boot. This will help prevent your muscles wasting (becoming weak) and joint stiffness. It will also reduce your risk of developing blood clots.
Once you are referred to Physiotherapy, you will be given an appointment and the physiotherapists will help you with any questions or concerns you may have.
Looking after yourself
Make sure you use your pump every morning. The pump takes the air out from inside the liner, making it tight around your lower leg. This will help reduce your risk of blood clots.
The pump is connected and fully inflated, this means there is a lot of air in the liner. Keep squeezing the pump until it is squashed, this means the air has been removed from the liner, and will be squeezing your lower leg to improve blood flow.
-
Fully inflated pump
-
‘Squashed’ pump
If your boot is creating pressure sores on your skin, you can place a dressing on the affected area(s).
If you feel your hips or back are suffering because of the uneven gait that wearing the boot causes, there are products available to buy that can help (such as wedges) by giving extra elevation (height) under your non-affected leg. Those provided by the VACOped company (called EVEN up) are one of many options.
If you feel numbness, “pins and needles”, pain, swelling, or your toes go unusually red / white / blue, you can release the tightness of your boot and see if that helps. You can also try and raise your foot to help redness, swelling, and pain. If you need further help, call the Physiotherapy Department at the William Harvey Hospital.
Recovering from an injury can take a long time and it is normal to get frustrated and anxious. But remember that while you are recovering, there are some things you can do to help your tendon to heal. We suggest limiting the amount of alcohol you drink, stopping smoking, eating a healthy diet, drinking plenty of fluids (especially water), and staying as active as you can, please discuss this with your clinician. If you need any extra support, do not hesitate to get in touch with us.
Smoking advice
Studies have shown that tendon healing is significantly delayed by smoking / nicotine. If you need support to stop smoking you can ask your GP for advice, or contact the Trust’s Stop Smoking Service by calling 03001 231220, or text QUIT to 87023.
How does eating a healthy diet help my recovery?
The quality of the food you eat will affect your healing and recovery. We suggest you follow a healthy well-balanced diet, rich in fruit, vegetables (including green leafy vegetables), nuts, seeds, wholegrains, lean fish, poultry, and legumes, which contain the necessary proteins and fibre, and drink plenty of water. For more information on the importance of eating your 5-A-Day, please go to the NHS: 5 a day: what counts? web site.
How do I look after my boot?
Unless told otherwise, for the first four weeks following your surgery you should try and treat the boot like a plaster cast and keep it on at all times. You will be followed up in the Fracture Clinic by a clinical specialist physiotherapist between weeks 2 and 3. At this appointment a member of the team will reassess your tendon, and change the cushion liner for you (please bring all your VACOped® equipment with you to these appointments).
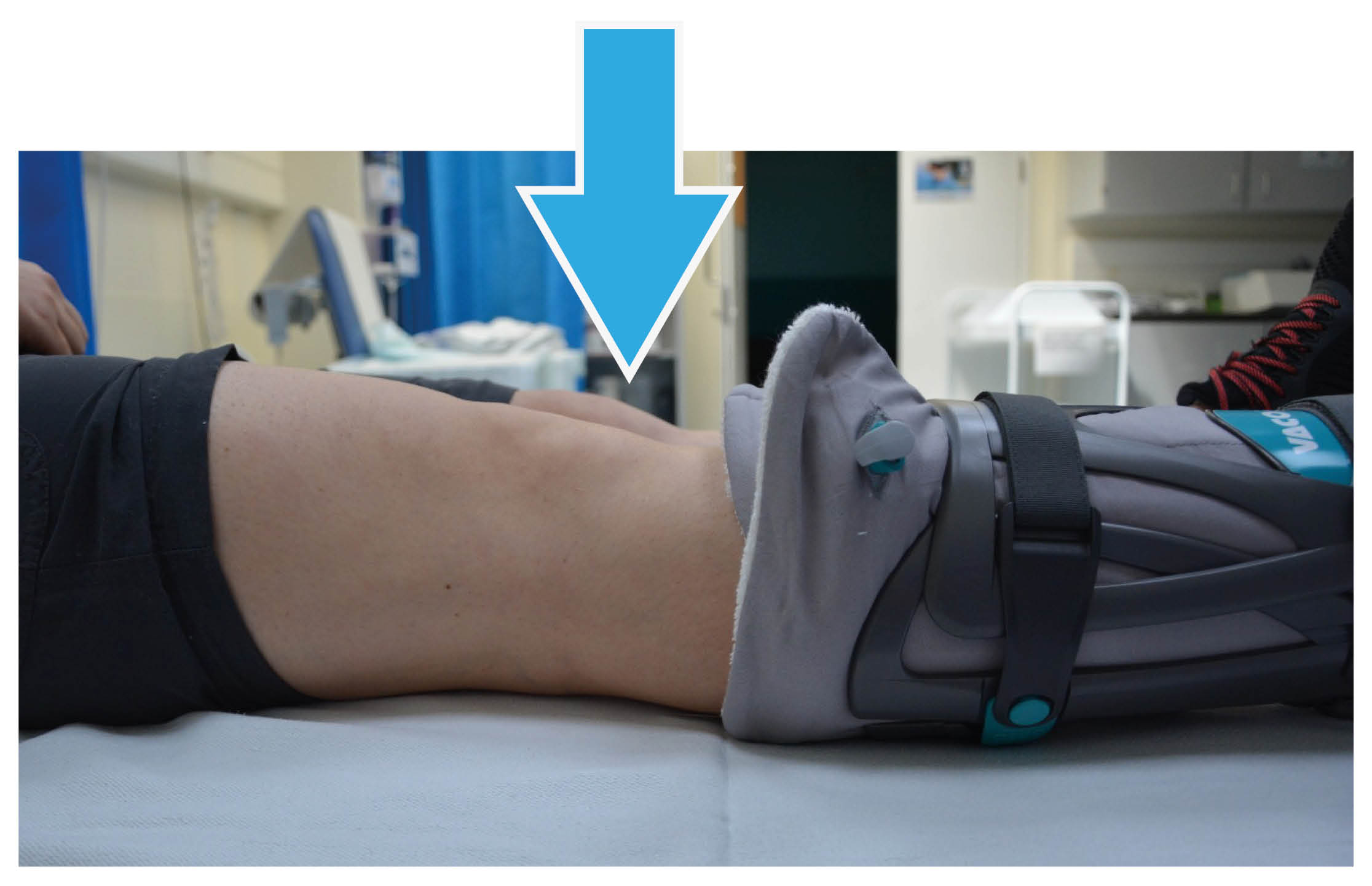
If the cushion liner gets wet or you notice your skin is becoming sore, you may remove the boot yourself to change the liner or check your skin. When removing the boot, you must keep your toes pointed down at all times. You may need someone to hold your foot to help you keep your ankle in this position.
After week 4, you may remove your boot each week to wash your leg and change the liner; remember to keep your foot pointed at all times. We suggest you have a seated wash until week 9, when the boot can be removed indoors, but we still advise you to be careful when showering after this point.
When removing your boot or changing the liner to wash it, you need to open the valve and give the inner liner a good shake to spread the beads equally all over. This is to make sure your boot works correctly, and avoids pressure areas. When putting the straps back on, follow the numeric order given on the tag under each strap. Remember that you should not remove your boot for the first four weeks following surgery, unless told otherwise.

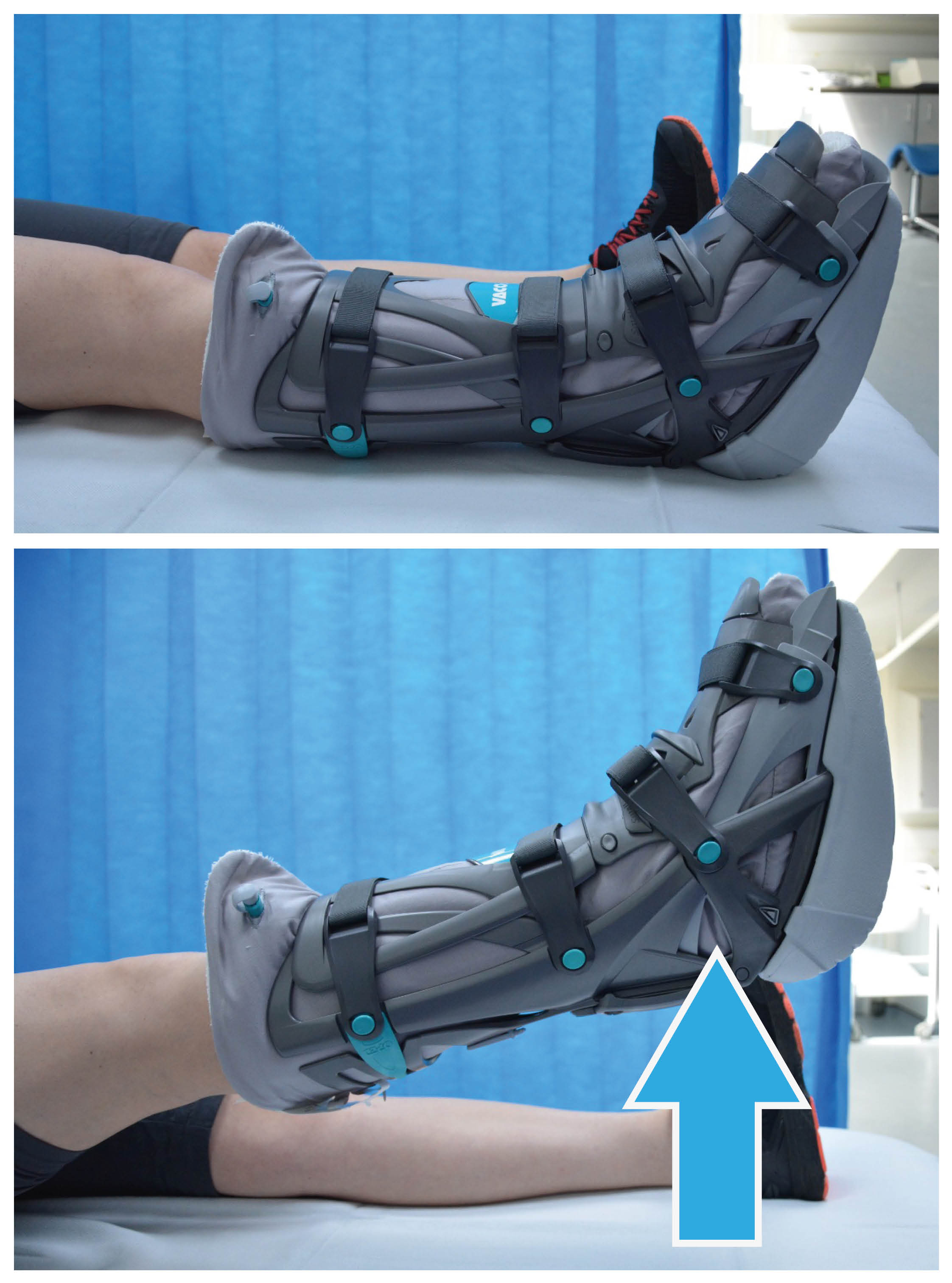
After week 4, you may remove the boot carefully to wash and change your sock, ideally no more than once a week. Whilst doing this you must keep your toes and ankle pointed down, as shown in the picture. Do not stretch your calf, as this could mean the tendon heals in a stretched position which will affect your overall rehabilitation.
Changing and washing the cushion liner
To change the cushion liner simply unzip it, remove the inner liner, and put in a clean cushion liner. Make sure each section comes in to the correct pouch in the cushion liner, and the valve comes out through the correct hole. Then zip it back and put it on.
You can wash the cushion liner in the washing machine up to 60°C.
You will be given two liners by the hospital. If you need any more, you can buy them from the OPED UK web site.
You can remove the sole of the boot before getting into bed, but remember to put it back on before getting up.
Do not throw away or loose the key that comes with the boot, you will need that later on in your treatment.
-
.jpeg) To remove the sole, press the “buttons” on both sides and it will disengage.
To remove the sole, press the “buttons” on both sides and it will disengage. -
.jpeg) When putting it back on, push it onto the bottom of the boot and you should be able to hear it “click” when in place.
When putting it back on, push it onto the bottom of the boot and you should be able to hear it “click” when in place.
Please remember you should not remove your boot at all for the first month, unless your skin becomes sore.
Afterwards, you must not put any weight through your affected leg at all while having the sole off (especially when waking up from bed at night), or when changing the sole, the liner, or showering / bathing.
For more information and explanatory videos on how to use the boot, please go to OPED UK web site.
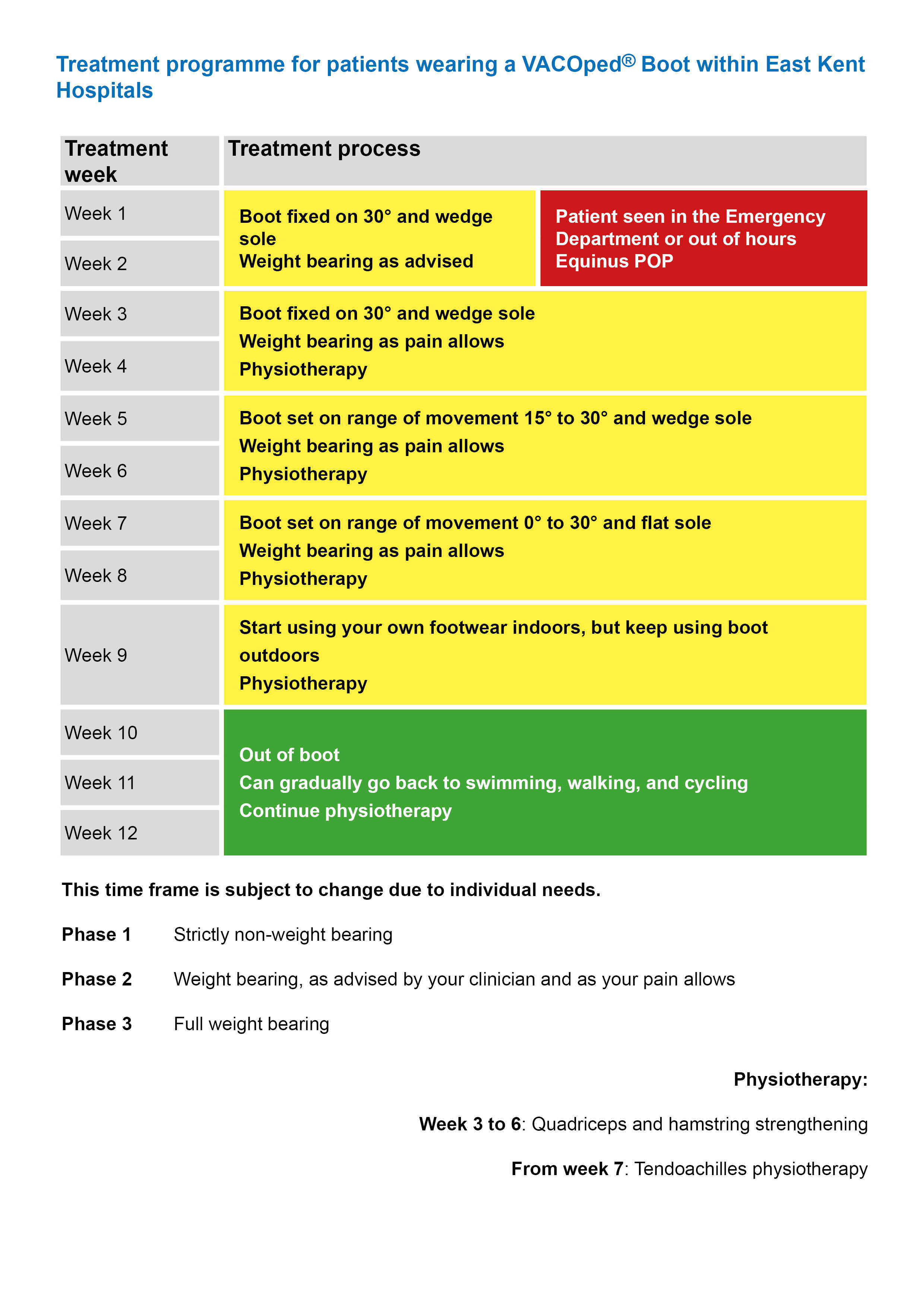
Weeks 1 and 2
If to start with, you are treated with a plaster cast:
You cannot weight-bear (put any weight on your affected leg) and you should help yourself by walking with crutches.
Your leg should be elevated (raised) above the level of your heart as much as possible.
You will be prescribed blood thinning drugs to take for the first six weeks following your surgery.
You will be referred for physiotherapy.
Your cast must not get wet; care needs to be taken when you are having a wash, bath, or shower, and pressure areas monitored.
Or, if you start being treated with a VACOped® Boot:
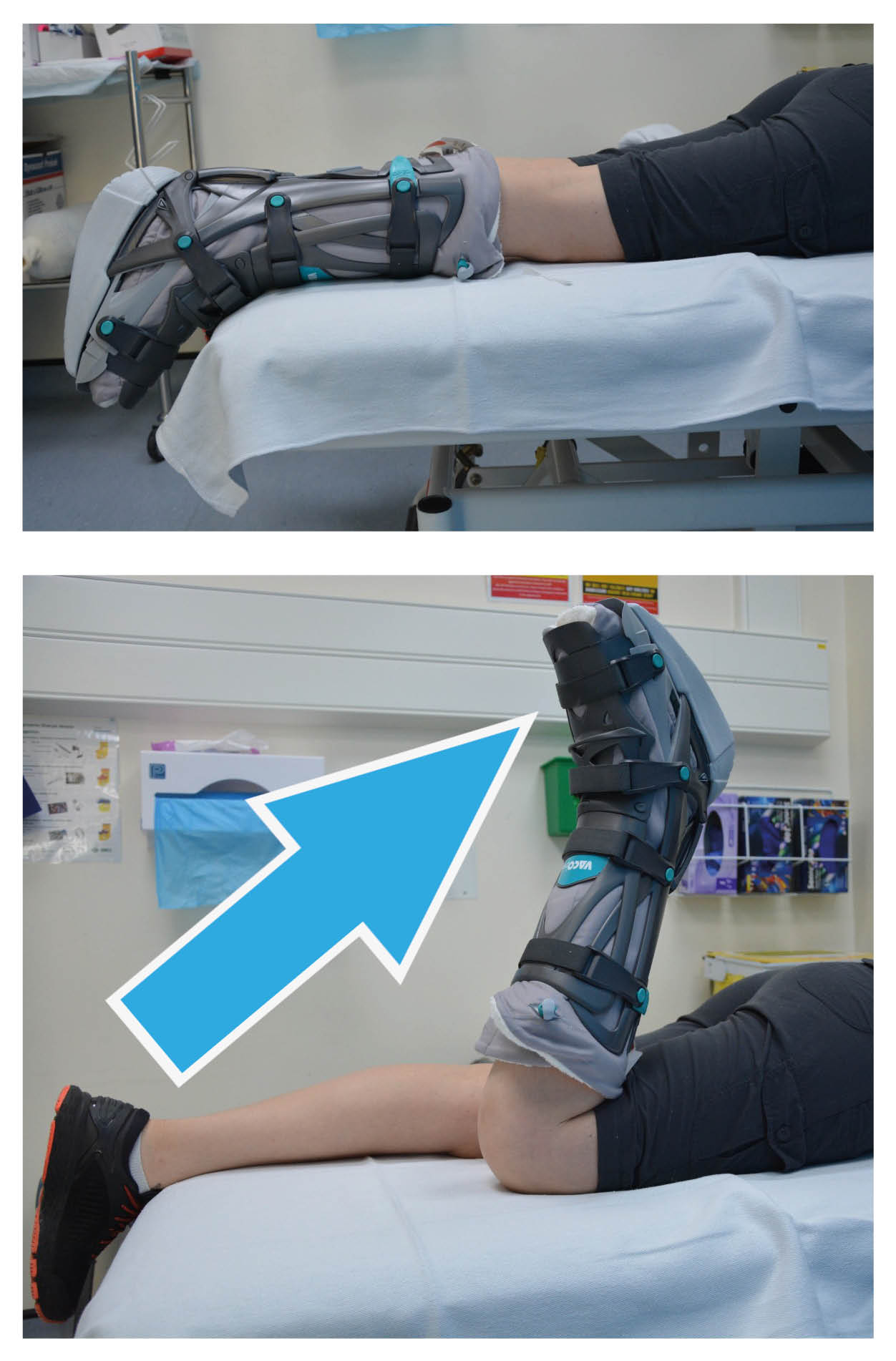
The boot will be locked with your foot pointing down at 30° and fitted with a wedged sole. The boot must be worn at all times.
You can weight-bear with crutches as advised by your clinician, depending on how much pain you are feeling and on the advice of the person treating you.
The boot must be worn at all times.
The sole of the boot can be removed overnight, but it must be put back on before putting any weight through it.
You will be trained on how to use the boot.
The boot must not get wet; care needs to be taken when you are having a wash, bath, or shower, and pressure areas monitored. You can have a dry wash for the first few weeks, buy a waterproof cover to protect your leg from getting wet, or if you have a bath keep your leg hanging outside. Home remedies, such as cling film or tape are not recommended, as water could still get through.
Your leg should be raised above the level of your heart as much as possible. To do this, you can use pillows when you sit or lay down. Or if you are laying on your sofa, you can rest your leg on the back of the sofa.
You will be prescribed blood thinning drugs to take for the first six weeks following your surgery.
You will be referred for physiotherapy.
The boot could cause blisters or wounds on the top of your foot and other areas. If your skin becomes sore make sure you put a padded dressing over the area and tell your clinician.
The boot needs to be tight enough to keep your foot in the right position, to avoid sliding and movement inside it. But not too tight that it may cause discomfort, pins and needles, or numbness.
At this stage you can wiggle your toes: it is important to keep your toes moving, so every two to three hours practice wiggling and spreading your toes.
Weeks 3 and 4
At this stage you will be reviewed by the Achilles clinical specialist physiotherapist
If you were treated in a plaster cast, this will be removed in the hospital and you will be given a VACOped® Boot, locked with your foot pointing down at 30°.
If you were treated in the VACOped® Boot you will remain in the boot, locked at 30°. You are allowed to weight-bear as your pain allows, with the help of crutches.
The boot must be worn at all times and must not get wet; care needs to be taken when you are having a wash, bath, or shower.
You should start quadriceps strengthening exercises at home.
Remember to bring your crutches, pump, and a clean liner (if it needs changing) to your clinic appointment.
There are several exercises you can start at week 3, whilst you are still in the boot. These exercises will help keep your leg strong.
Below you will find quadricep, hamstring, and gluteal strengthening exercises. You will need to work each muscle group separately, but the advise below will suggest how you should progress with each exercise.
Please complete each exercise at least 5 days a week for the best recovery possible.
Quadriceps strengthening exercises
1.Static quadriceps exercise
Either sitting or lying down, with your knee out straight on a flat surface, tighten the muscles on the front of your thigh by pushing the back of your knee down into the bed.
Hold for five to 10 seconds, then relax.
Repeat the exercise 10 times, then rest for 60 seconds.
Aim to do this two to three times.
2.Inner range quadricep exercise
Lie down and place a rolled towel under your knee for support.
Tighten your thigh muscle and lift your foot up to straighten your knee. Keep your knee on the towel at all times.
Hold for five to 10 seconds, then relax. Repeat the exercise 10 times, then rest. Aim to do this two to three times.
Do not move on to the next exercise until you can lift your knee completely straight for the full 10 repetitions.
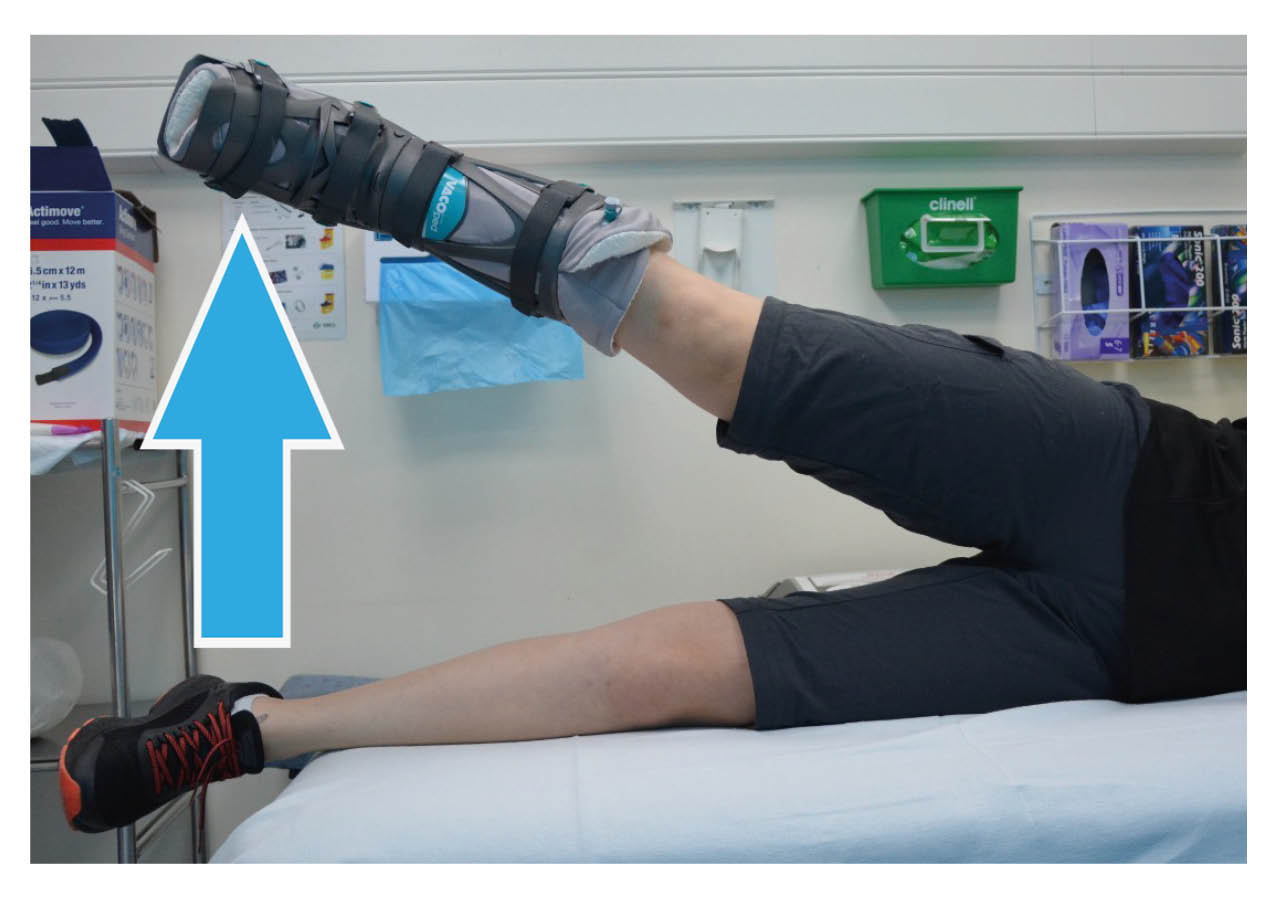
3.Straight leg raise
With your leg straight on a flat surface, tighten your thigh muscles to hold your knee straight and lift your leg up. Aim to lift your leg 30 to 40cm off the surface then lower it down gently.
Aim to hold your leg up for at least five seconds, and slowly lower it back down. Repeat the exercise 10 times, then rest for 60 seconds. Aim to do this two to three times.
Continue to do this exercise over the next seven weeks.

4.Seated knee extension exercise
Sitting down with your legs hanging over the edge of a bed or chair, raise your foot until you straighten your leg.
Hold for five to 10 seconds, then slowly lower it back down. Repeat the exercise 10 times, then rest for 60 seconds. Aim to do this two to three times.
Hamstring strengthening exercises
1.Prone knee bend exercise
Lay flat on your front.
Slowly bend your knee up to 90° and lower it back down again. Repeat the exercise 10 times, then
rest for 60 seconds. Aim to do this two to three times.
If you find this too easy, do this exercise standing up as shown below (see Standing exercises below).
2.Standing exercises
Stand up and hold on to something sturdy for support (for example your kitchen counter). Make sure you keep your back straight with every exercise.
Standing knee flexion
Stand with both legs straight and together.
Bend your knee, bringing your foot up behind you. Keep your hips straight and your knees together.
Relax your leg back down and repeat.
Repeat the exercise 10 times, then rest for 60 seconds. Aim to do this two to three times.
If this exercise becomes too easy, speak to your physiotherapist, who can give you a resistance band.
Gluteal strengthening exercises
1.Hip extension in prone
Lay on your front.
Tighten your bottom muscles and lift your thigh up off the floor. Keep your knee straight at all times. Do not allow your pelvis to lift off the floor.
Hold for five to 10 seconds then lower down gently.
Repeat the exercise 10 times, then rest for 60 seconds. Aim to do this two to three times.
Continue to do this exercise over the next seven weeks.

2.Hip abduction in standing
Standing up tall with your feet together, bring your leg out to the side whilst keeping your knee straight. Keep your body straight, do not lean to the side as you lift your leg.
Gently lower your leg back down again.
Repeat the exercise 12 times, then rest for 60 seconds. Aim to do this three times.
Do not move on to the next exercise until you can complete this one without your body leaning away from your affected leg.
Progress to side lying if this exercise is too easy.
3.Hip abduction in side lying
Laying on your uninjured side, lift your top leg up towards the ceiling. Keep your knee straight at all
times. Your hip should be in line with your knee and ankle. Do not allow your hips to roll back as
you lift your leg.
Repeat the exercise 12 times, then rest for 60 seconds. Aim to do this three times.
Continue to do this exercise over the next seven weeks.
Weeks 5 and 6
Your boot will be altered to give you more range of movement of 15° to 30°. This can be done either by a member of hospital staff or you can do it yourself. If you have been shown how to alter your boot by the hospital, please refer to the User Guide you were given.
You can start to gently bend your ankle up and down whilst wearing your boot. Your ankle may feel tight, so do not force the movement into any pain or too much of a stretch. Just gently start to get your ankle moving again.
Please continue to do the exercises from weeks 3 and 4, as well as those shown below.
From week 5, you may remove your boot to wash your foot. Only do this while sitting, and keep your foot pointing down at all times when the boot is off. Only do this once a week if possible. You must not stand up or take any weight through your foot without the boot on. Stay seated while drying your leg. Put the boot back on as quickly as possible, as care needs to be taken not to stretch or re-rupture your tendon.
When showering, the boot must be worn at all times. Make sure the boot is covered and does not get wet. Please speak to your therapist for advice on where to buy protective covers for your boot.
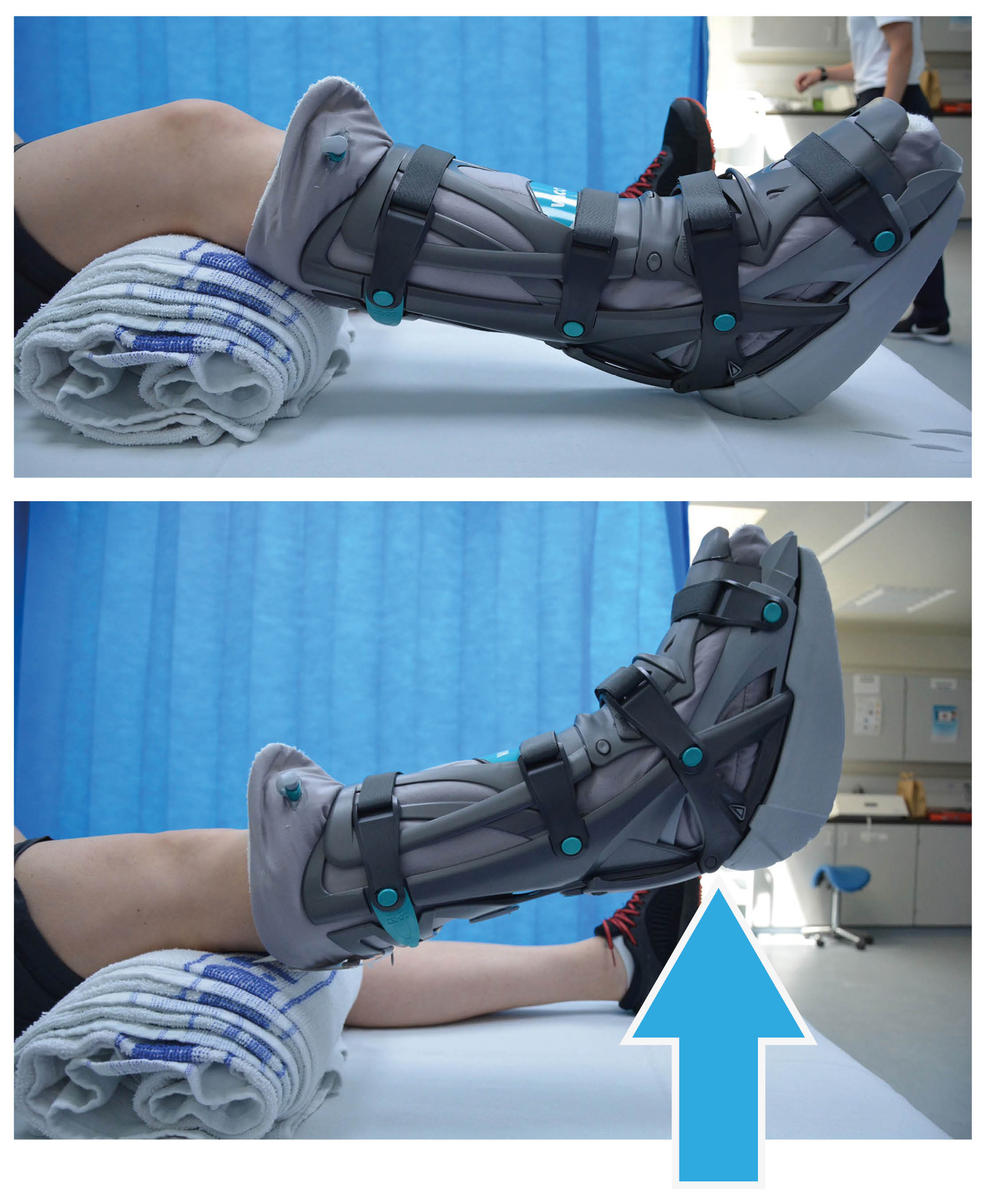
Ankle range of movement
You can bend your ankle up and down in the boot in any position, but you may find this most comfortable when laying on your front with your foot hanging over the edge of the bed.
Pointing your ankle down will be difficult as your muscles are weak, but keep practicing and focus on the movement coming from the back of your heel and not your toes. This will be discussed in more detail at your Achilles clinic appointment.
Complete this exercise 10 times, once or twice a day.
-
.jpg) Bend your ankle up
Bend your ankle up -
.jpg) Bend your ankle down
Bend your ankle down
Your aim at week 6 is to have a full range of movement in your hip and knee, and no pain in your Achilles tendon while you are resting.
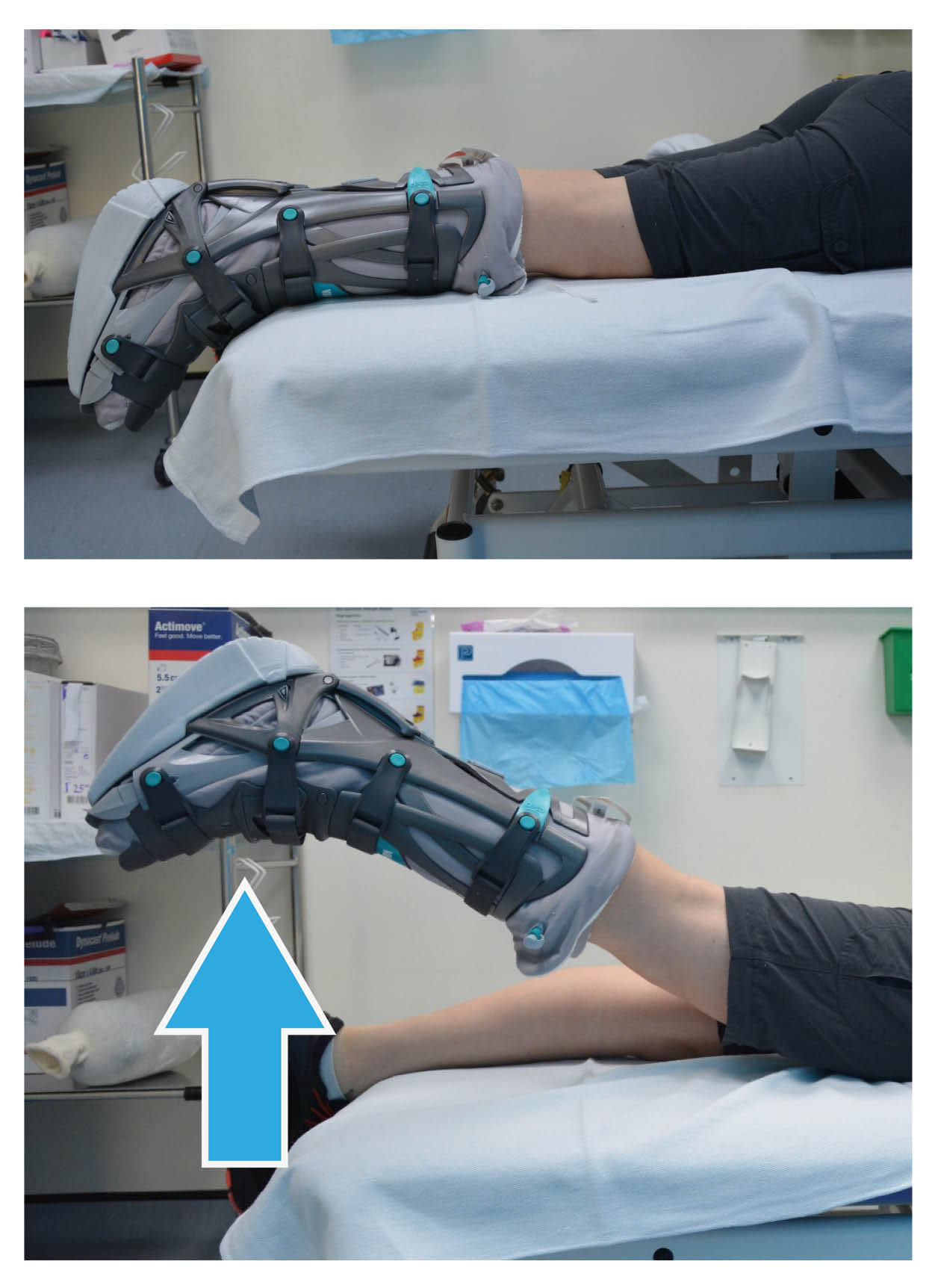
Weeks 7 and 8
At week 7, your boot will be altered again, this time providing you with 0° to 30° range of movement at your ankle, and the wedge sole will be swapped for a flat sole. This is where you will notice the biggest difference when walking in the boot.
1.Active ankle range of movement
You can remove your boot once a day to carry out the following gentle range of movement exercises for your ankle. These exercises should only be done if you are feeling no pain while doing them. Aim to complete each exercise 10 times, three times in a row. Rest for 60 seconds between each set of 10.
Active plantar flexion (pointing your toes)
Please note when bending your ankle up and down, do not bend your ankle up past its neutral position, we do not want to stretch your Achilles tendon at this stage. This is because the strength of the tendon is at its weakest at this time, and stretching it could mean elongating (over-stretching) or re-rupturing your tendon.
-
.jpg) Do not bend your ankle up past its neutral position (where the line is drawn)
Do not bend your ankle up past its neutral position (where the line is drawn) -
.jpg) Point your toes
Point your toes
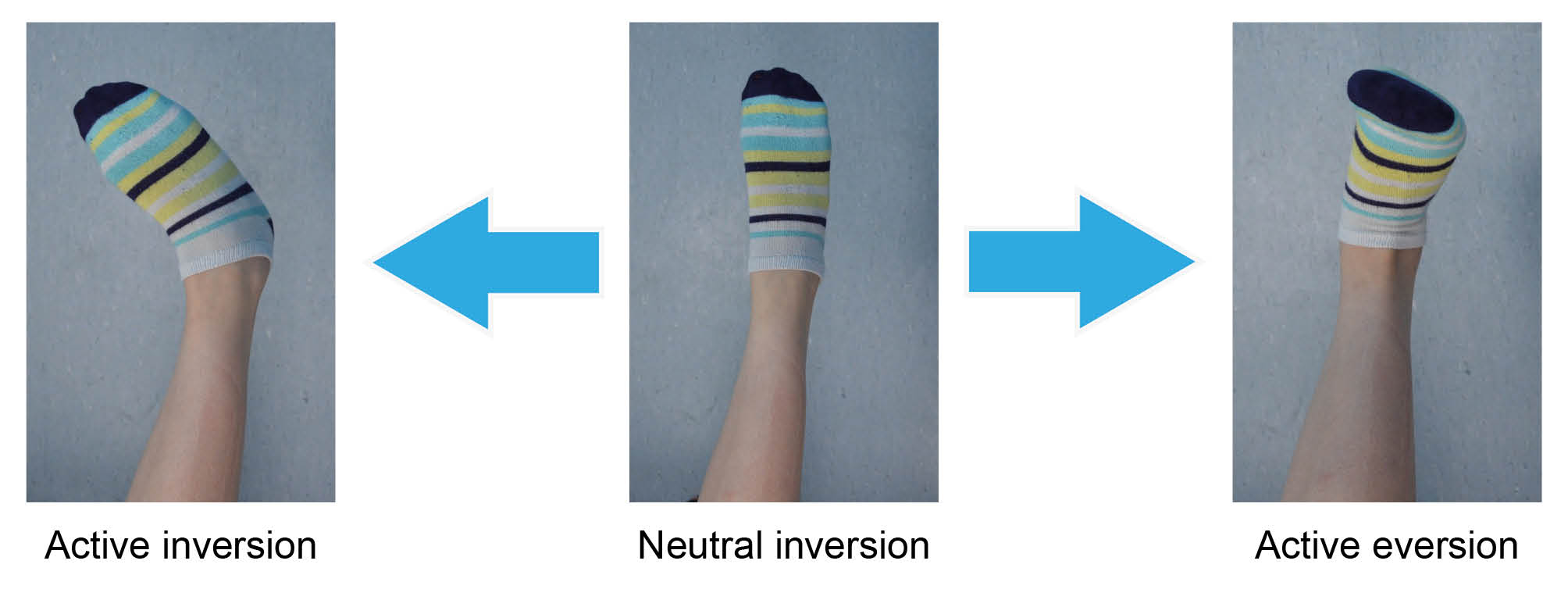
Inversion: keep your leg straight and turn your ankle inwards.
Eversion: keep your leg straight and turn your ankle out and up.
2.Isometric ankle strengthening exercises
With your boot on, you can now start to strengthen the muscles around your ankle. This is known as isometric strengthening, and is a way of strengthening the muscles around a joint without moving the joint itself.
The muscles in your lower leg move your ankle in four directions, so it is important to target all four of these muscle groups.
These exercises can be completed up to three times a day, if possible. For each exercise aim to hold the position for five to 10 seconds as you are able, then relax. Repeat each exercise five to 10 times.
Dorsiflexion
Place your uninjured foot over the top of the boot. Push the top of your injured foot up into the boot, resisting with your other foot. You should feel the muscles in the front of your lower leg tighten but your ankle should not move. Do not push if you feel pain.

Plantar flexion
In long sitting, place your hands behind you for support. Rest your feet against a wall or the end of the bed.
Push your toes into the wall, as if to try and push the wall away. Feel the muscles of your calf tightening. Your ankle should not move.
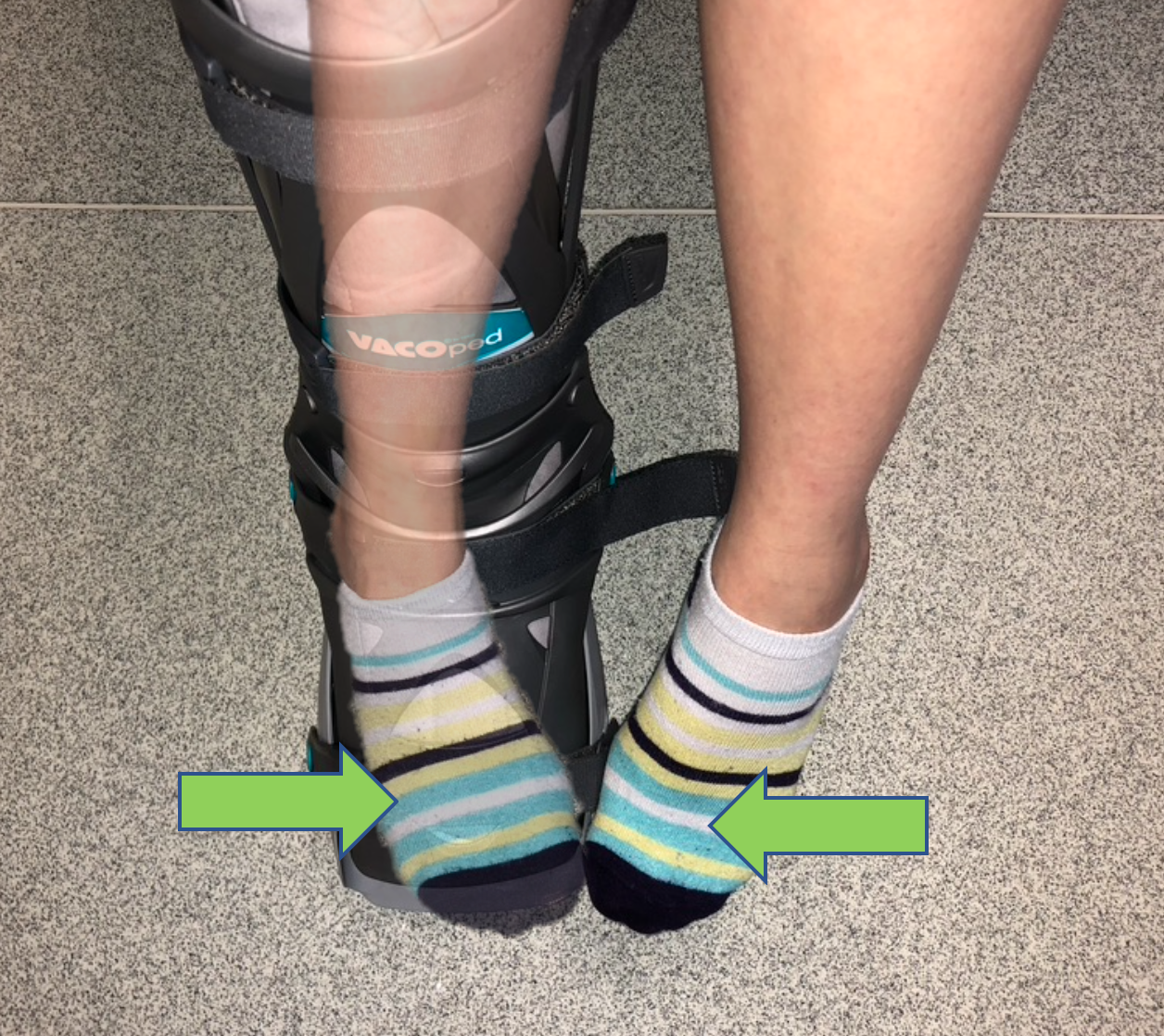
Inversion
Push in against your other foot (toe to toe). You should feel the muscles on the inside of your calf tighten. Do not push into any pain.

Eversion
Cross your injured leg behind your non-injured leg. Push your little toe of your injured leg into the heel of your non-injured leg. You should feel the muscles on the outside of your calf tighten. Do not push into any pain.
Remember, these exercises should not be painful. Please start with a gentle push, approximately half of your strength, and then gradually push harder if the exercise remains pain free.
Your aim by week 8 is to be walking as normally as possible with or without crutches.
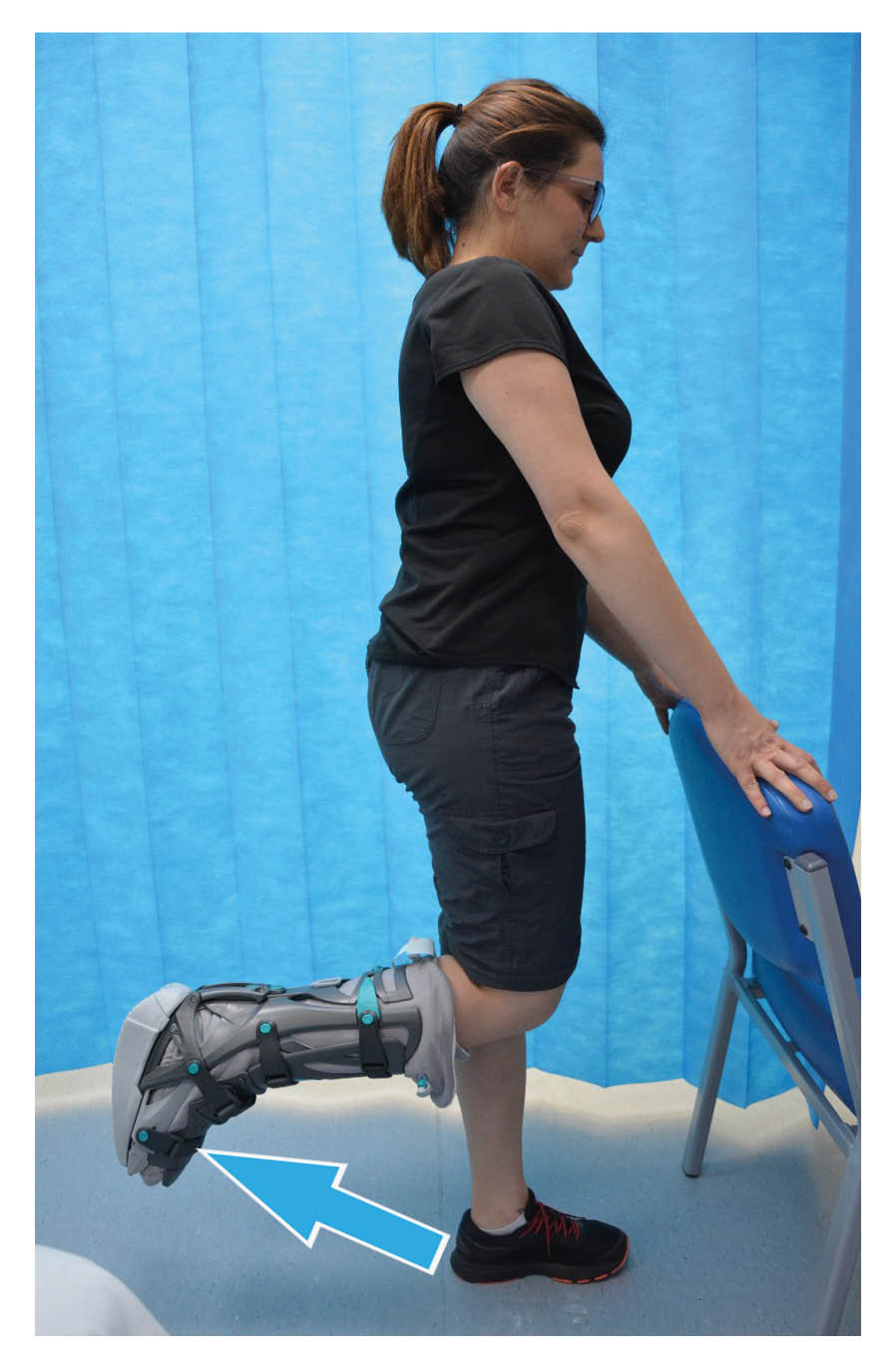
Week 9
You can remove the boot while indoors, but you must wear supportive footwear indoors at all times and continue to wear the boot outside. If the isometric ankle strengthening exercises above are too easy by week 9, you can stop them and move on to the exercises shown below.
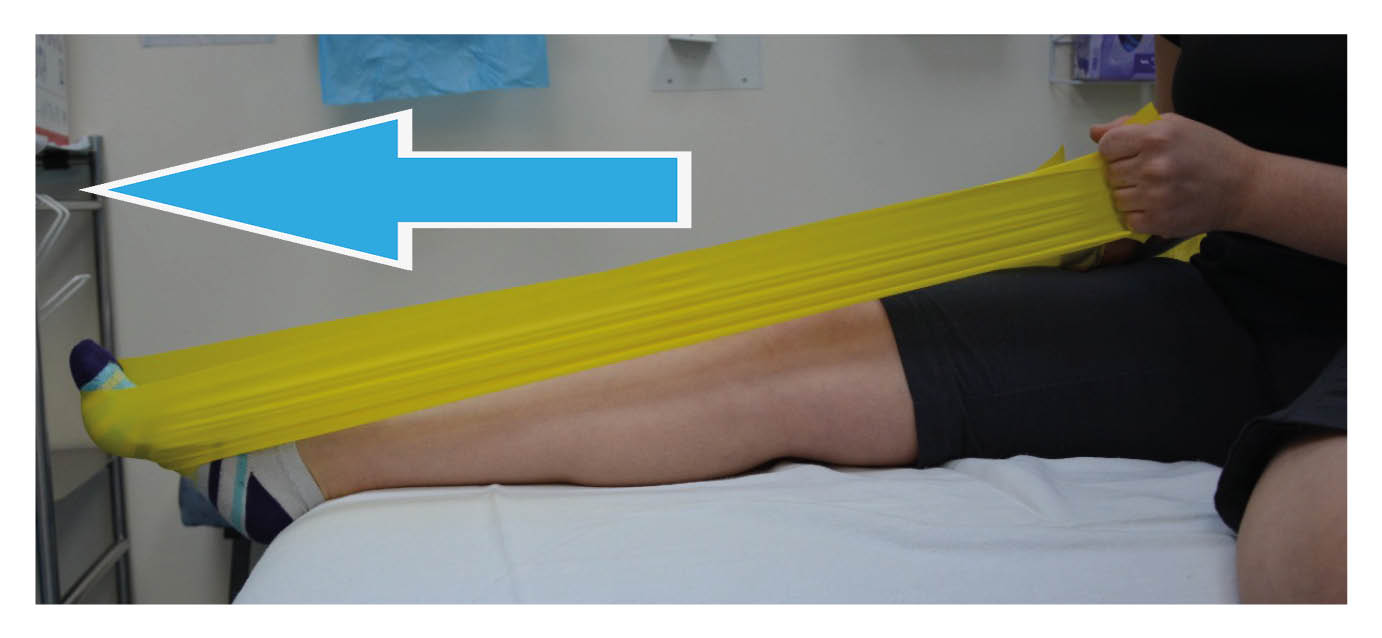
Isotonic ankle strengthening
The next exercises are isotonic strengthening exercises. They strengthen the muscles around your ankle joint by moving the joint into resistance.
Aim to complete each exercise 10 times, then rest for 60 seconds. Do this two to three times.
Avoid pulling the band too tight against the bottom of your foot, we do not want to stretch your tendon yet.
-
 1.Plantar flexion with the knee straight; Point your toes, pushing into the band.
1.Plantar flexion with the knee straight; Point your toes, pushing into the band. -
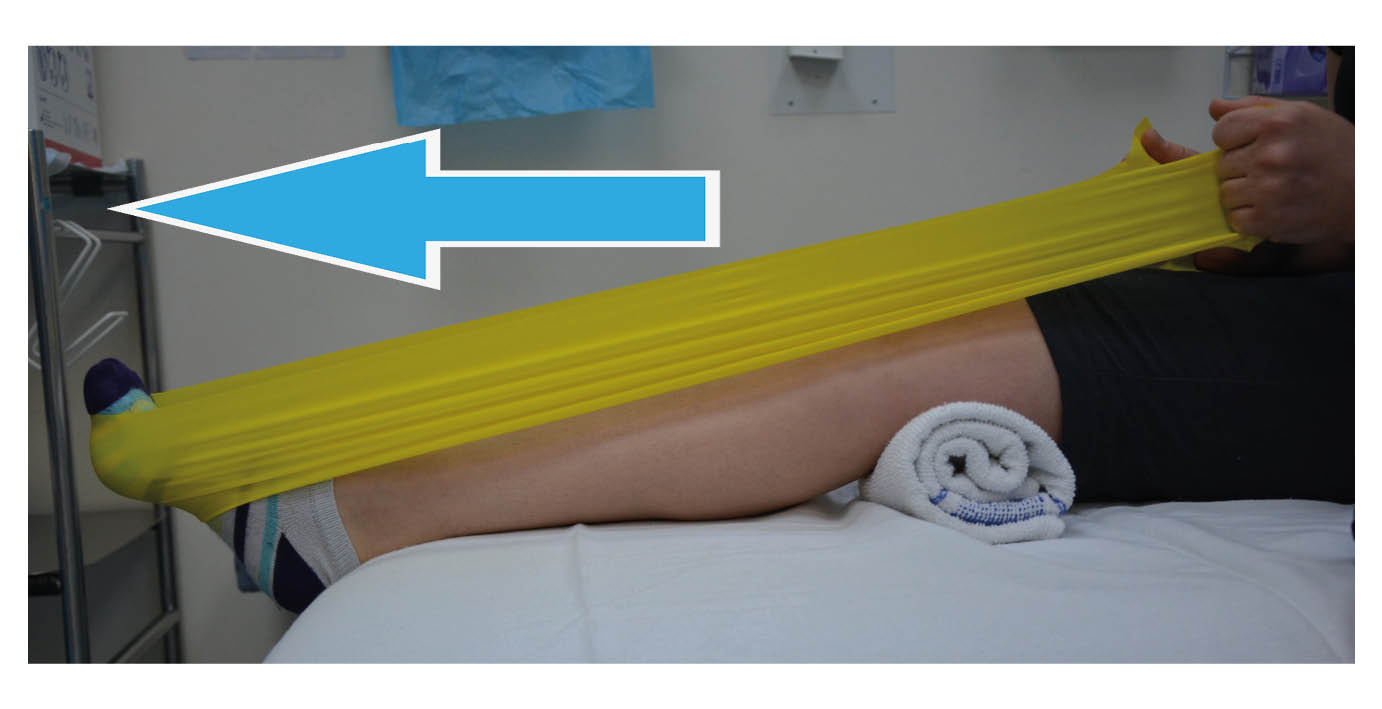 2.Plantar flexion with the knee slightly bent; Point your toes, pushing into the band.
2.Plantar flexion with the knee slightly bent; Point your toes, pushing into the band.
-
.jpg) 3.Inversion; Turn your ankle in, pulling in against the resistance band.
3.Inversion; Turn your ankle in, pulling in against the resistance band. -
.jpg) 4.Eversion; Turn your ankle out, pulling out against the resistance band.
4.Eversion; Turn your ankle out, pulling out against the resistance band.
5.Balance exercises

You must also start to challenge your balance. You can do this by practicing standing on one leg without holding on.
Aim to keep your balance unsupported for up to 10 seconds, then increase this as your balance improves. See how the balance on your injured leg compares to your non-injured leg.
If this gets too easy, try closing your eyes.
Your aim by week 9 is to have full side to side movement of your ankle, and to be able to point your toes down to 30° without the boot on.
You will now be referred for more formal physiotherapy in the Physiotherapy Department. At this stage your physiotherapist will progress your exercises accordingly.
Week 10
From week 10, the boot can be fully removed (indoors and outdoors) and your aim is to walk without a limp or crutches. At this stage you may return to swimming and cycling to help increase your fitness. It is common to have some heel pain at this time. Buying some gel heel cups can be very helpful to offload the tendon and reduce the forces through your heel whilst you walk. Your exercises will be progressed to further strengthen your leg and ankle and improve your balance.
Over the next three to nine months you will work closely with your physiotherapist to achieve your goals, whether that is performing day to day tasks or returning to sport.
We do not recommend that you start any sports again until nine to 12 months after your injury, depending on whether your milestones have been met. Your physiotherapist will discuss these milestones with you and re-assess your injury regularly.
Caution: for the first 12 weeks after your injury, your healing tendon will be at its weakest. It is therefore essential that you do not try to do too much, too soon. If you have any concerns or queries, please speak to your physiotherapist.

